Abstract
Purpose
The outcomes of open surgical repair (OR) or endovascular aneurysm repair (EVAR) for abdominal aortic aneurysm (AAA) are favorable; however, pre-existing chronic renal insufficiency (CRI) is considered to be a risk factor that can affect the long-term outcome. We evaluated our surgical strategy for AAA in patients with CRI by analyzing their pre- and postoperative renal function.
Methods
We conducted a retrospective chart review of CRI patients who underwent OR (n = 28) or EVAR (n = 31) for infra-renal AAA in our institution between 2009 and 2013. Our operative strategy included pre- and postoperative adequate hydration, postoperative diuretics and low-dose dopamine for both groups, intravascular ultrasonography and carbon dioxide angiography to reduce the amount of contrast media needed in the EVAR group, and occasional intraoperative mannitol for the OR group.
Results
The preoperative estimated glomerular filtration rate (eGFR) increased significantly in the postoperative period and remained similar 6 months later in both groups, without any difference in changes between the groups. In-hospital postoperative complications included leg occlusion in one EVAR patient. There were no complication-related deaths in either group.
Conclusions
Postoperative renal function was similar after the two approaches, indicating that both procedures could be performed safely using our strategy for patients with CRI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Open surgical repair (OR) has been the first line treatment for abdominal aortic aneurysm (AAA) for approximately half a century, with low postoperative mortality and morbidity rates as a result of improved perioperative care and operative techniques [1]. However, pre-existing chronic renal insufficiency (CRI) is known to increase the long-term risks of mortality and renal deterioration postoperatively [2, 3]. Vascular surgeons have adopted various renal protection methods, including perioperative hydration, acetylcysteine, and mannitol; however, the effects of these methods are controversial and the protection strategies differ among institutes [4–6].
Although the outcomes of AAA repair have improved since the emergence of endovascular aneurysm repair (EVAR), preoperative CRI is still a comorbid factor, potentially caused by the use of contrast medium during the EVAR procedure and repeated serial computed tomography scans during the follow-up, which may have adverse effects on renal function [7–9]. In Japan, EVAR was approved for use in 2006, and gained popularity as a minimally invasive treatment for AAA [10, 11]. Moreover, the outcomes associated with EVAR have been excellent, largely because of technical and device improvements through two decades of EVAR experiences in other countries [12]. In Japan, we have also adopted intravascular ultrasonography (IVUS) and carbon dioxide (CO2) angiography for renal protection since its inception [12–14].
A recent large randomized study revealed that neither OR nor EVAR was associated with deteriorating renal function in the long term [15]. However, AAA repair in patients with pre-existing CRI is strongly associated with procedure-related adverse effects, with renal impairment reported to occur in approximately 30 % of these patients [8]. CRI patients have also been found to be at increased risk of mortality [16], with moderate renal dysfunction (estimated glomerular filtration rate (eGFR): 30–60 mL/min/1.73 m2) associated with a 5.2-fold higher risk of dialysis after OR than after EVAR [17].
We have recently established a perioperative strategy for both OR and EVAR, focusing attention on renal protection. We conducted this study to evaluate our strategy by analyzing and comparing AAA patients with pre-existing CRI undergoing OR with those undergoing EVAR.
Methods
We collected data on 59 patients with CRI, who underwent OR or EVAR for infrarenal AAA between January, 2009 and April, 2013, retrospectively, from our institution’s medical records. The same group of vascular surgeons working at the same institution treated all patients. Renal function was assessed by the eGFR, calculated by the chronic kidney disease epidemiology collaboration formula. Patients with an eGFR <60 mL/min/1.73 m2, classified as ≥ chronic kidney disease (CKD) stage 3, according to the National Kidney Foundation, were defined as having CRI and were included in the analysis. Hemodialysis patients diagnosed preoperatively were excluded from the analysis.
All patients provided informed consent, and all procedures were performed in accordance with the ethical standards of the institutional ethics committee under the Declaration of Helsinki 1975, as revised in 2000. Our perioperative strategy included pre- and postoperative adequate hydration (100 ml/h/50 kg body weight for at least 24 h before the operation), postoperative diuretics and low-dose dopamine in both groups (when the urine output was less than 200 ml/4 h), IVUS and CO2 angiography to reduce the amount of contrast media needed in the EVAR group, and the occasional intraoperative use of mannitol in the OR group. Moreover, patients were hospitalized for 1–2 weeks preoperatively, so that we could assess their cardiac, respiratory, liver, and cerebrovascular function and check for other systemic comorbidities (Table 1).
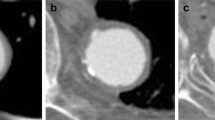
For patients with normal renal function, OR is generally the first surgical option, based on the patients’ age and the absence of comorbid conditions. EVAR is offered to patients with suitable anatomy, including a proximal landing zone of at least 15 mm and proximal neck angulation less than 60°, without shaggy aorta or extreme tortuosity. The surgical indication for CRI patients is basically the same as that for patients with normal renal function. OR was performed in 28 patients (22 men, 6 women), and EVAR was performed in 31 patients (23 men, 8 women). OR was performed via a transperitoneal approach in all except two patients in whom it was performed via a retroperitoneal approach. All patients received intravenous heparin before aortic clamping. With EVAR, 23 Excluder (W. L. Gore and Assoc., Flagstaff, AZ, USA) and 8 Zenith (Cook Diagnostic, Bloomington, IN, USA) endografts were used. IVUS was performed in 23 (74.1 %) patients, and a combination of IVUS and CO2 angiography was performed in 3 (9.6 %) patients.
Table 2 summarizes the patient demographics and intraoperative variable data of the OR and EVAR groups. The analyzed postoperative variables included postoperative length of stay, chronological renal function, and in-hospital postoperative complications.
We identified preoperatively that AAA had induced disseminated intravascular coagulation and blue toe syndrome in one OR patient. The mean follow-up period was 25 months (range, 4–53 months). Renal function was assessed preoperatively, on postoperative day (POD) 1, and during follow-up examinations at 1 and 6 months, by checking for changes in the eGFR. Comparisons of continuous variables between the OR and EVAR groups were conducted using t tests. We also used t tests to compare the groups over time. All analyses were conducted using JMP Pro (version 11.2.1; SAS Institute, Cary, NC), and significance was set at P < 0.05.
Results
The EVAR patients were significantly older than the OR patients (80.1 ± 6.4 vs. 75.8 ± 7.0 years, respectively; P < 0.01). The EVAR patients had shorter operative times (180 ± 80 vs. 246 ± 50 min; P < 0.0001), were less likely to require an intraoperative transfusion (25.3 ± 8.7 vs. 54.0 ± 17.1 mL/kg; P < 0.0001) or intraoperative blood transfusion (36 ± 95 vs. 770 ± 676 mL; P < 0.0001), were less likely to bleed (147 ± 123 mL vs. 1384 ± 538 mL; P < 0.0001), and had a shorter hospital stay (8.6 ± 2.9 vs. 15.4 ± 4.7 days; P < 0.0001). In the EVAR group, the mean volume of contrast administered intraoperatively was 62.4 ± 38.4 mL (range 3–162 mL). There were no significant differences in other comorbidities (Table 2).
The CKD stages were classified as 3, 4, and 5 in 49 (83 %), 9 (15.3 %), and 1 patients (1.7 %), respectively. CKD stage 3 was diagnosed in 22 patients (78.6 %) from the OR group and 27 patients (87 %) from the EVAR group, while CKD stage 4 was diagnosed in 5 patients (17.8 %) from the OR group and 4 patients (12.9 %) from the EVAR group. CKD stage 5 was only present in the OR group (Table 2).
The eGFR increased significantly from the preoperative value of 43.1 ± 12.4 mL/min/1.73 m2 to 47.2 ± 13.7 mL/min/1.73 m2 (P < 0.0001) on POD1 and 46.1 ± 12.9 mL/min/1.73 m2 (P = 0.002) at the 1-month follow-up, but returned to baseline by 6 months postoperatively (42.0 ± 12.7 mL/min/1.73 m2, P = 0.29; Fig. 1). In the OR group, the eGFR increased significantly from the preoperative value of 43.5 ± 14.4 mL/min/1.73 m2 to 47.3 ± 16.0 mL/min/1.73 m2 (P = 0.01) on POD1, but returned to the baseline values by the 6-month follow-up (42.9 ± 13.4 mL/min/1.73 m2, P = 0.77; Fig. 2). In the EVAR group, the eGFR increased significantly from the preoperative value of 42.7 ± 10.4 mL/min/1.73 m2, to 47.1 ± 11.6 mL/min/1.73 m2 (P = 0.001) on POD 1 and to 47.2 ± 11.5 mL/min/1.73 m2 (P = 0.001) at the 1-month follow up, but returned to baseline by 6 months postoperatively (41.4 ± 12.3 mL/min/1.73 m2, P = 0.21; Fig. 2). There were no significant differences in the eGFR levels between the OR and EVAR patients preoperatively (P = 0.81), or on POD 1 (P = 0.93), or at the 1-month follow-up (P = 0.49), or the 6-month follow-up (P = 0.67; Fig. 2).
Two patients from the OR group (7.1 %), required hemodialysis after surgery, which was permanent for one (eGFR: preoperative, 12.2 mL/min/1.73 m2; postoperative, 11.7 mL/min/1.73 m2) and temporary for the other (eGFR: preoperative, 17.1 mL/min/1.73 m2; postoperative, 12.7 mL/min/1.73 m2). The physicians had recommended permanent dialysis from the beginning for the former patient, whereas the latter patient required temporary dialysis for anuria and prolonged fluid retention. However, both patients recovered well postoperatively. The only in-hospital postoperative complication was a leg occlusion in one EVAR patient (3.2 %). This patient required re-intervention with thrombectomy accompanied by a stent graft in the affected leg. There were no complication-related deaths.
Discussion
Our perioperative strategy prevented a deterioration in the renal function of patients with pre-existing CRI, postoperatively and for up to 6 months, with similar results in the OR and EVAR groups. In both groups, transient postoperative increases in the eGFR were observed, which subsequently returned to the baseline levels. This temporary increase was also observed in our previous study, which focused on patients with juxtarenal AAA [5]. We assumed that this unique phenomenon may be due to an increase in renal arterial flow. Thus, perioperative sufficient hydration and low-dose dopamine should be reasonable strategies for this purpose.
The permanent or temporary postoperative dialysis rates of CRI patients have been reported to range from 8–28 % after OR and from 9–29 % after EVAR [3, 8]. In the present study, very few patients required dialysis (7.1 %), which might be attributable to our operative strategy and recent improvements in the devices used. We speculate that the one case of leg occlusion might have been related to procedural or device-related failure.
Acute renal failure caused directly by the operative procedure in OR contributes to consequent renal deterioration. Previously, we found that once OR patients overcome the initial postoperative invasive period, few suffer adverse renal effects [5]. Mills et al. compared OR and EVAR by CKD stages, and observed an initial and transient decrease in the eGFR in the OR group but not in the EVAR group; however, the renal deterioration during the long-term follow-up was more severe in the EVAR group [18]. Their results indicate that the renal function of EVAR patients is impaired by a factor not derived from the operative procedure itself, such as nephropathy caused by the repetitive use of contrast media during follow-up examinations.
To reduce the adverse effect of contrast media, we used IVUS and CO2 angiography during EVAR. We previously revealed that using IVUS reduced the need for contrast media and was associated with good outcomes; hence, we have been using this routinely since 2011 [13]. In the present series of CRI patients, 74 % of those who underwent EVAR were supported by the IVUS method. CO2 angiography is also considered valuable for patients with CRI or those with contrast allergy [14]. EVAR accompanied by CO2 reportedly preserves the eGFR without affecting the technical success rate, with a similar 1-year endoleak rate to iodinated-contrast EVAR [19]. We do not use CO2 routinely because of the possible risk of air embolism, so CO2 use for EVAR was only 9.6 % in the present study. Furthermore, although various drugs have been reported to be useful for renal protection, including acetylcysteine and bicarbonate infusion, which have been associated with decreased incidences of contrast nephropathy [4, 20], we did not use these agents as their effects are still controversial. A previous meta-analysis revealed that low-dose dopamine can improve renal physiology transiently, but it is not of clinical benefit to patients with, or at risk of, acute renal failure [21]. Conversely, Sirivella reported that the infusion of a solution of mannitol, furosemide, and dopamine promoted diuresis in patients with postoperative acute renal failure and reduced the need for dialysis [22]. Based on these previous studies, we consider that the postoperative use of diuretics and low-dose dopamine for both groups and the occasional intraoperative use of mannitol for the OR group may still be reasonable strategies.
The definition of CRI is still controversial. Recent studies have tended to adopt eGFR as a more sensitive prognostic indicator than serum creatinine values [16, 18, 23, 24]. Walsh et al. reported that the eGFR data indicated CRI in a greater percentage of patients with aortic aneurysms than the serum creatinine data (33 vs. 11 %, respectively) [25]. In this study, we based our definition of CRI as CKD stages 3 and 4 on the findings of a previous report that compared OR and EVAR and analyzed long-term renal function using CKD stages [18].
In the present study, we excluded patients undergoing suprarenal clamping from the OR group as the outcome of OR accompanied by suprarenal clamping compared favorably to that of usual OR in our previous study [5]. However, some authors have reported harmful effects of the suprarenal clamp, which can cause renal artery complications, the release of cytokines, and ischemia–reperfusion [26], with an even further increased risk of renal dysfunction with prolonged renal ischemia (≧23 min) [27]. Thus, we decided that EVAR patients, all of whom were treated at the infrarenal site, should be compared with OR patients without suprarenal clamping to avoid selection bias.
According to a systematic review, the changes in renal function after OR and EVAR are still conflicting, and the results of our study do not appear to corroborate these reviewed studies. The outcomes relating to postoperative renal function during the 6 months of follow-up were similar between OR and EVAR in this study, indicating that both these procedures when performed under our strategies are safe for maintaining renal function. McCullough reported that reasonable goals for patients with CKD include diagnostic cardiac catheterization contrast doses of <30 mL and <100 mL for percutaneous coronary intervention, computed tomography, and other intravascular studies [28]. The intraoperative contrast dose given to the EVAR patients in the present study (62.4 ± 38.4 mL) was within this range and seemed to be adequate, so this should be helpful for improving our operative strategy further. A previous study reported that the contrast dose given to AAA patients with normal renal function who underwent EVAR was 148 ± 20 mL [29]. Hence, the contrast dose given to the EVAR patients in the present study was half of that given to the patients with normal renal function. We always try to give as low a dose of contrast as reasonably practicable during EVAR to patients with CRI. Advances in digital image processing have done much to keep contrast doses lower than before. Recent studies show that the routine use of image fusion during EVAR significantly reduces contrast volume during complex EVAR [30].
This study has some limitations. First, the sample size was small. A larger study sample would have allowed sub-analysis based on the degree of renal dysfunction severity and analysis of postoperative events, including the risk of dialysis. Second, the follow-up was not long enough as at least 2 years is recommended to confirm declines in renal function [24]. Third, patients with diffuse massive atheroma lining along the aortic wall on CT, known as “shaggy aorta” [31] underwent OR due to the risk of peripheral or visceral embolization which can be induced by EVAR. Although there were only three (10.7 %) patients with massive atheroma in the OR group, we should not ignore this selection bias.
In conclusion, eGFR remained unchanged after OR and EVAR, even 6 months postoperatively, and only one patient required permanent hemodialysis during the follow-up period. The outcomes relating to postoperative renal function were similar after OR and EVAR, indicating that both these procedures can be performed safely using our surgical indications and with our own strategy, to preserve renal function in patients with CRI. Further studies are warranted to confirm our findings.
References
Crawford ES, Saleh SA, Babb JW 3rd, Glaeser DH, Vaccaro PS, Silvers A. Infrarenal abdominal aortic aneurysm: factors influencing survival after operation performed over a 25-year period. Ann Surg. 1981;193:699–709.
Nathan DP, Brinster CJ, Jackson BM, Wang GJ, Carpenter JP, Fairman RM, et al. Predictors of decreased short- and long-term survival following open abdominal aortic aneurysm repair. J Vasc Surg. 2011;54:1237–43.
Powell RJ, Roddy SP, Meier GH, Gusberg RJ, Conte MS, Sumpio BE. Effect of renal insufficiency on outcome following infrarenal aortic surgery. Am J Surg. 1997;174:126–30.
Birck R, Krzossok S, Markowetz F, Schnulle P, van der Woude FJ, Braun C. Acetylcysteine for prevention of contrast nephropathy: meta-analysis. Lancet. 2003;362:598–603.
Hoshina K, Nemoto M, Shigematsu K, Nishiyama A, Hosaka A, Miyahara T, et al. Effect of suprarenal aortic cross-clamping. Circ J. 2014;78:2219–24.
Miller DC, Myers BD. Pathophysiology and prevention of acute renal failure associated with thoracoabdominal or abdominal aortic surgery. J Vasc Surg. 1987;5:518–23.
Alsac JM, Zarins CK, Heikkinen MA, Karwowski J, Arko FR, Desgranges P, et al. The impact of aortic endografts on renal function. J Vasc Surg. 2005;41:926–30.
Parmer SS, Fairman RM, Karmacharya J, Carpenter JP, Velazquez OC, Woo EY. A comparison of renal function between open and endovascular aneurysm repair in patients with baseline chronic renal insufficiency. J Vasc Surg. 2006;44:706–11.
Saratzis A, Sarafidis P, Melas N, Saratzis N, Kitas G. Impaired renal function is associated with mortality and morbidity after endovascular abdominal aortic aneurysm repair. J Vasc Surg. 2013;58:879–85.
Kyuragi R, Matsumoto T, Okadome J, Kawakubo E, Homma K, Iwasa K, et al. Endovascular aneurysm repair for an abdominal aortic aneurysm and a left ruptured common iliac artery aneurysm in a patient with hepatocellular carcinoma: report of a case. Surg Today. 2014;44:1548–51.
Maeda T, Ito T, Kurimoto Y, Watanabe T, Kuroda Y, Kawaharada N, et al. Risk factors for a persistent type 2 endoleak after endovascular aneurysm repair. Surg Today. 2015;45:1373–7.
Hoshina K, Hashimoto T, Kato M, Ohkubo N, Shigematsu K, Miyata T. Feasibility of endovascular abdominal aortic aneurysm repair outside of the instructions for use and morphological changes at 3 years after the procedure. Ann Vasc Dis. 2014;7:34–9.
Hoshina K, Kato M, Miyahara T, Mikuriya A, Ohkubo N, Miyata T. A retrospective study of intravascular ultrasound use in patients undergoing endovascular aneurysm repair: its usefulness and a description of the procedure. Eur J Vasc Endovasc Surg. 2010;40:559–63.
Morito H, Hoshina K, Hosaka A, Okamoto H, Shigematsu K, Miyata T. Endovascular surgery for inflammatory abdominal aortic aneurysm with contrast allergy-usefulness of carbon dioxide angiography and intravascular ultrasound: a case report. Ann Vasc Dis. 2012;5:104–8.
de Bruin JL, Vervloet MG, Buimer MG, Baas AF, Prinssen M, Blankensteijn JD, et al. Renal function 5 years after open and endovascular aortic aneurysm repair from a randomized trial. Br J Surg. 2013;100:1465–70.
Patel VI, Lancaster RT, Mukhopadhyay S, Aranson NJ, Conrad MF, LaMuraglia GM, et al. Impact of chronic kidney disease on outcomes after abdominal aortic aneurysm repair. J Vasc Surg. 2012;56:1206–13.
Nguyen BN, Neville RF, Rahbar R, Amdur R, Sidawy AN. Comparison of outcomes for open abdominal aortic aneurysm repair and endovascular repair in patients with chronic renal insufficiency. Ann Surg. 2013;258:394–9.
Mills JL Sr, Duong ST, Leon LR Jr, Goshima KR, Ihnat DM, Wendel CS, et al. Comparison of the effects of open and endovascular aortic aneurysm repair on long-term renal function using chronic kidney disease staging based on glomerular filtration rate. J Vasc Surg. 2008;47:1141–9.
Criado E, Upchurch GR Jr, Young K, Rectenwald JE, Coleman DM, Eliason JL, et al. Endovascular aortic aneurysm repair with carbon dioxide-guided angiography in patients with renal insufficiency. J Vasc Surg. 2012;55:1570–5.
Merten GJ, Burgess WP, Gray LV, Holleman JH, Roush TS, Kowalchuk GJ, et al. Prevention of contrast-induced nephropathy with sodium bicarbonate: a randomized controlled trial. JAMA. 2004;291:2328–34.
Friedrich JO, Adhikari N, Herridge MS, Beyene J. Meta-analysis: low-dose dopamine increases urine output but does not prevent renal dysfunction or death. Ann Intern Med. 2005;142:510–24.
Sirivella S, Gielchinsky I, Parsonnet V. Mannitol, furosemide, and dopamine infusion in postoperative renal failure complicating cardiac surgery. Ann Thorac Surg. 2000;69:501–6.
Azizzadeh A, Sanchez LA, Miller CC 3rd, Marine L, Rubin BG, Safi HJ, et al. Glomerular filtration rate is a predictor of mortality after endovascular abdominal aortic aneurysm repair. J Vasc Surg. 2006;43:14–8.
Saratzis A, Sarafidis P, Melas N, Khaira H. Comparison of the impact of open and endovascular abdominal aortic aneurysm repair on renal function. J Vasc Surg. 2014;60:597–603.
Walsh SR, Tang T, Sadat U, Varty K, Boyle JR, Gaunt ME. Preoperative glomerular filtration rate and outcome following open abdominal aortic aneurysm repair. Vasc Endovasc Surg. 2007;41:225–9.
Saratzis AN, Goodyear S, Sur H, Saedon M, Imray C, Mahmood A. Acute kidney injury after endovascular repair of abdominal aortic aneurysm. J Endovasc Ther. 2013;20:315–30.
Knott AW, Kalra M, Duncan AA, Reed NR, Bower TC, Hoskin TL, et al. Open repair of juxtarenal aortic aneurysms (JAA) remains a safe option in the era of fenestrated endografts. J Vasc Surg. 2008;47:695–701.
McCullough PA. Radiocontrast-induced acute kidney injury. Nephron Physiol. 2008;109:61–72.
Chao A, Major K, Kumar RS, Patel K, Trujillo I, Hood BD, et al. Carbon dioxide digital subtraction angiography-assisted endovascular aortic aneurysm repair in the azotemic patient. J Vasc Surg. 2007;45:451–60.
Maurel B, Hertault A, Sobocinski J, Le Roux M, Gonzalez TM, Azzaoui R, et al. Techniques to reduce radiation and contrast volume during EVAR. J Cardiovasc Surg. 2014;55:123–31.
Hoshina K, Hosaka A, Takayama T, Kato M, Ohkubo N, Okamoto H, et al. Outcomes after open surgery and endovascular aneurysm repair for abdominal aortic aneurysm in patients with massive neck atheroma. Eur J Vasc Endovasc Surg. 2012;43:257–61.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We have no conflicts of interest to declare.
Rights and permissions
About this article
Cite this article
Haga, M., Hoshina, K., Shigematsu, K. et al. A perioperative strategy for abdominal aortic aneurysm in patients with chronic renal insufficiency. Surg Today 46, 1062–1067 (2016). https://doi.org/10.1007/s00595-015-1286-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-015-1286-0