Abstract
Purpose
We conducted this retrospective cohort study to evaluate which preoperative comorbidities and their combinations are most strongly associated with postoperative complications after gastrectomy.
Methods
We collected data on 214 consecutive patients who underwent gastrectomy for gastric cancer. Preoperative comorbidities were placed into one of ten categories: cardiac, pulmonary, liver, renal, central nervous system, hypertension, diabetes, endocrine/metabolic, vascular, and immune/hematological. The relationship between the number of comorbidities and the incidence of postoperative complications was evaluated.
Results
Among 120 patients (56.1 %) with comorbidities, 48 had a single comorbidity and 72 had multiple (≥2) comorbidities. The incidence of postoperative complications was 45.8 % (33/72) for patients with multiple comorbidities and 23.9 % (34/142) for those with 0 or 1 comorbidity (P = 0.001). Among the ten types of comorbidities, only pulmonary (P = 0.019) and vascular diseases (P = 0.007) were significantly associated with the occurrence of postoperative complications.
Conclusion
Patients with multiple comorbidities had a significantly higher incidence of postoperative complications after gastrectomy. Among the comorbidities studied, pulmonary and vascular diseases had the strongest association with postoperative complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastric cancer is the fourth most common cancer and the second leading cause of cancer-related death in the world [1, 2]. Surgical resection is the only curative treatment for gastric cancer, but postoperative complications are not uncommon, even in the high-volume hospitals, and their occurrence is influenced by various clinicopathological factors. According to previous studies, the risk factors for postoperative complications after gastrectomy include advanced age, male sex, high body mass index, poor nutritional status, total gastrectomy, extended lymph node dissection, and advanced tumor stage [3–10]. With the increasing life expectancy in many countries [11], the proportion of elderly patients diagnosed with gastric cancer is also increasing [12]. Elderly patients are likely to have more comorbidities, such as hypertension, diabetes, cardiovascular diseases, and pulmonary disorders, and the presence of a comorbid condition is considered to be associated with a higher risk of postoperative complications. Although several studies have shown that comorbidity is a risk factor for postoperative complications [13–16], there are few details on the risks associated with preoperative comorbidity. Thus, we conducted a retrospective cohort study to evaluate the relationship between the number of preoperative comorbidities and postoperative complications in patients undergoing gastrectomy for gastric cancer. The secondary aim of this study was to clarify what kinds of preoperative comorbidities are significantly related to postoperative complications after gastrectomy.
Materials and methods
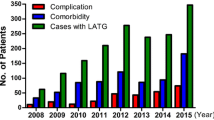
We collected data retrospectively on 214 consecutive patients who underwent curative gastrectomy for histologically confirmed gastric cancer at Osaka University Hospital between January 2010 and December 2011. Patients who underwent concurrent procedures for synchronous malignant tumors were excluded. We used the 14th edition of the Japanese classification of gastric carcinoma to establish pT and pN stage [17]. We collected the data of preoperative comorbidities from the preoperative summary sheet. This sheet included preoperative risk factors based on history, preoperative examinations such as blood tests, electrocardiogram, and spirometry, and preoperative consultation with other specialists, such as a cardiologist. The prognostic nutrition index (PNI) was calculated as follows: 10 × serum albumin level + 0.05 × total lymphocyte count [18].
We divided the comorbid diseases into ten categories: cardiac, pulmonary, liver, renal, central nervous system, hypertension, diabetes, endocrine/metabolic, vascular, and immune/hematological (Table 1). The severity of each disease was not assessed. We counted the number of preoperative comorbidities for each patient. All postoperative events were evaluated according to the Clavien–Dindo classification system [19], and we considered complications of grade II or higher as postoperative complications in this study. We evaluated the relationship between clinicopathological factors, including the number of preoperative comorbidities, and the occurrence of postoperative complications, using the Chi-squared test for categorical variables and the Mann–Whitney U test for continuous variables. We also evaluated which kinds of comorbidities were associated with the highest risk of postoperative complications, using univariate and multivariate logistic regression. P < 0.05 was considered significant. All statistical analyses were performed with the SPSS statistics software package, version 20 (IBM Corp., Armonk, NY, USA).
Results
Of the 214 patients, 120 (56.1 %) had preoperative comorbidities. The most common comorbidity was hypertension (26.6 %), followed by cardiac (14.0 %), pulmonary (13.6 %), and endocrine/metabolic disorders (13.6 %), respectively (Table 2). Among the 120 patients with preoperative comorbidities, 48 (40.0 %) had one comorbidity, 37 (30.8 %) had two comorbidities, 24 (20.0 %) had three comorbidities, and 11 (9.2 %) had four or more comorbidities.
There were 67 patients (31.3 %) who experienced postoperative complications. Major complications included anastomotic leakage (5.1 %), pancreatic fistula (4.7 %), postoperative bleeding (4.2 %), abdominal abscess (3.7 %), food stasis (3.7 %), anastomotic stenosis (1.9 %), cholecystitis (1.9 %), and ascites (1.9 %). We evaluated the relationship between clinicopathological factors and the occurrence of postoperative complications (Table 3). Among the ten clinicopathological factors studied, age (P = 0.034), PNI (P = 0.043), surgical approach (P = 0.011), extent of lymph node dissection (P = 0.002), pT stage (P < 0.001), and the number of comorbidities (P = 0.003) were significantly associated with postoperative complications. When we dichotomized the number of comorbidities, two groupings 0 vs. ≥1 and 0 or 1 vs. ≥2 showed a significant relationship with postoperative complications (P = 0.028 and P = 0.001, respectively), but 0 or 1 vs. ≥2 had a higher odds ratio (2.69; 95 % confidential interval, 1.47–4.91) than 0 vs. ≥1 (1.96; 95 % confidential interval, 1.07–3.59). When the number of comorbidities was grouped as 0–2 vs. ≥3, there was no significant relationship (P = 0.23). The incidence of postoperative complications among patients who had multiple (≥2) comorbidities vs. those who had no or one comorbidity was 45.8 % (33/72) vs. 23.9 % (34/142), respectively. In the multivariate logistic regression model with all ten clinicopathological factors, only pT2–4 (P = 0.006) and multiple comorbidities (P = 0.014) were identified as significant risk factors for postoperative complications.
The incidence of each intra-abdominal complication in patients with multiple comorbidities vs. those with no or one comorbidity was as follows: anastomotic leakage, 4.2 vs. 5.6 %; pancreatic fistula, 4.2 vs. 4.9 %; postoperative bleeding, 5.6 vs. 3.5 %; abdominal abscess, 6.9 vs. 2.1 %; and food stasis, 5.6 vs. 5.6 %. Although there was no significant difference in the incidence of any intra-abdominal complication between the groups, extra-abdominal complications such as pneumonia, delirium, cerebral infarction, and pulmonary embolism occurred more frequently in patients with multiple comorbidities than in patients with no or one comorbidity [11.1 % (8/72) vs. 1.4 % (2/142), P = 0.003].
Next, we evaluated which preoperative comorbidities were significantly related to postoperative complications. Among the ten types of comorbidities evaluated, only pulmonary (P = 0.019) and vascular diseases (P = 0.007) were significantly associated with postoperative complications according to both the univariate and multivariate analyses (Table 4). The risk of postoperative complications among patients with multiple comorbidities that included either pulmonary or vascular disease was 55.9 % (19/34), whereas the risk among those with multiple comorbidities excluding pulmonary and vascular diseases was 36.8 % (14/38).
Discussion
In the present study, we categorized preoperative comorbidities into ten categories and analyzed whether the number of preoperative comorbidities, and which kinds, could effectively predict postoperative complications after gastrectomy. Patients who had multiple (≥2) comorbidities had a significantly higher risk of postoperative complications than those who had no or one comorbidity. Among the comorbidities, pulmonary and vascular diseases were the most strongly associated with postoperative complications. The risk of postoperative complications among patients with multiple comorbidities that included either pulmonary or vascular disease exceeded 50 %; therefore, careful perioperative management is needed for this patient population.
Preoperative comorbidity is generally considered to be associated with a higher risk of postoperative complications for any type of surgery. In the field of gastric cancer surgery, some studies have found that comorbidity and old age are important risk factors for complications [13, 14]. The importance of comorbidity as a risk factor was recently demonstrated in patients who underwent laparoscopic gastrectomy [15, 20]. In these studies, patients were divided into two groups according to whether they had preoperative comorbidities or not. However, considering that elderly patients who require gastrectomy often have at least one comorbid disease, the presence of a single comorbidity may not be as relevant for predicting postoperative complications. Indeed, patients with well-controlled hypertension usually experience relatively few complications after gastrectomy. Jeong et al. [21] reported that multiple comorbidities were associated with postoperative complications in elderly patients. Similarly, our study revealed that the existence of multiple comorbidities was a more reliable indicator of postoperative complications than that of single comorbidity. Furthermore, patients with multiple comorbidities had a higher incidence of extra-abdominal complications but not intra-abdominal complications. Since the number of comorbidities is probably a reflection of a patient’s systemic condition, this may be a reliable predictor, especially of extra-abdominal complications.
Hypertension, cardiopulmonary disease, and liver disease have already been reported as risk factors for postoperative complications after gastrectomy [20, 22, 23]. Jeong et al. [24] reported that gastric cancer patients with abnormal pulmonary function had a significantly higher incidence of local and systemic complications than other patients. They found that anastomotic leakage and wound complications were more common in patients with abnormal pulmonary function. Our study also revealed pulmonary and vascular diseases as significant risk factors for postoperative complications. In patients with abnormal pulmonary function, hypoxia and malnutrition may result in poor wound healing. Regarding vascular disease, as most studies combined vascular disease with cardiac disease into a single category of cardiovascular disease, we could not find any studies that specifically analyzed the relationship between vascular disease and postoperative complications. Although cardiac and vascular disorders have some causes in common, we considered cardiac and vascular diseases as having different impacts on postoperative outcome. For example, cardiac diseases such as decreased pump function may be compensated for with medications, whereas vascular diseases such as arteriosclerosis usually involve irreversible damage to blood vessels that cannot easily be compensated for with medications. The most common vascular disease was arteriosclerosis-related disease, which is associated with poor oxygen supply to peripheral tissues and may cause chronic changes in the functioning of multiple organs. Indeed, all patients with vascular disease in our study had two or more comorbidities.
This study did not evaluate the effect of the severity of each comorbidity on the occurrence of postoperative complications because there is no standard method to evaluate the severity of comorbidities. Instead, we evaluated the number of comorbidities, because this may reflect the overall disease burden for each patient. Patients with severe dysfunction of one organ system tend to have disorders involving multiple organ systems. A good example of this is the patient with chronic renal failure, who usually has secondary hypertension as well. A large-scale prospective study using the same criteria for classifying preoperative comorbidities is needed to confirm our conclusions.
References
Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127:2893–917.
Shinohara S, Korenaga D, Edagawa A, Koushi K, Itoh S, Kawanaka H, et al. Significant prognostic factors in patients with Stage IV gastric cancer with special reference to the curability of surgery. Surg Today. 2013;43:40–7.
Katai H, Sasako M, Sano T, Maruyama K. The outcome of surgical treatment for gastric carcinoma in the elderly. Jpn J Clin Oncol. 1998;28:112–5.
Lee KG, Lee HJ, Yang JY, Oh SY, Bard S, Suh YS, et al. Risk factors associated with complication following gastrectomy for gastric cancer: retrospective analysis of prospectively collected data based on the Clavien-Dindo system. J Gastrointest Surg. 2014;18:1269–77.
Jiang X, Hiki N, Nunobe S, Kumagai K, Nohara K, Sano T, et al. Postoperative pancreatic fistula and the risk factors of laparoscopy-assisted distal gastrectomy for early gastric cancer. Ann Surg Oncol. 2012;19:115–21.
Wu XS, Wu WG, Li ML, Yang JH, Ding QC, Zhang L, et al. Impact of being overweight on the surgical outcomes of patients with gastric cancer: a meta-analysis. World J Gastroenterol. 2013;19:4596–606.
Kim MG, Yook JH, Kim KC, Kim TH, Kim HS, Kim BS. Influence of obesity on early surgical outcomes of laparoscopic-assisted gastrectomy in gastric cancer. Surg Laparosc Endosc Percutan Tech. 2011;21:151–4.
Guo W, Ou G, Li X, Huang J, Liu J, Wei H. Screening of the nutritional risk of patients with gastric carcinoma before operation by NRS 2002 and its relationship with postoperative results. J Gastroenterol Hepatol. 2010;25:800–3.
Memon MA, Subramanya MS, Khan S, Hossain MB, Osland E, Memon B. Meta-analysis of D1 versus D2 gastrectomy for gastric adenocarcinoma. Ann Surg. 2011;253:900–11.
Hiura Y, Takiguchi S, Yamamoto K, Kurokawa Y, Yamasaki M, Nakajima K, et al. Use of fibrin glue sealant with polyglycolic acid sheets to prevent pancreatic fistula formation after laparoscopic-assisted gastrectomy. Surg Today. 2013;43:527–33.
Wang H, Dwyer-Lindgren L, Lofgren KT, Rajaratnam JK, Marcus JR, Levin-Rector A, et al. Age-specific and sex-specific mortality in 187 countries, 1970-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2071–94.
Kitamura K, Yamaguchi T, Taniguchi H, Hagiwara A, Yamane T, Sawai K, et al. Clinicopathological characteristics of gastric cancer in the elderly. Br J Cancer. 1996;73:798–802.
Gong DJ, Miao CF, Bao Q, Jiang M, Zhang LF, Tong XT, et al. Risk factors for operative morbidity and mortality in gastric cancer patients undergoing total gastrectomy. World J Gastroenterol. 2008;14:6560–3.
Seo SH, Hur H, An CW, Yi X, Kim JY, Han SU, et al. Operative risk factors in gastric cancer surgery for elderly patients. J Gastric Cancer. 2011;11:116–21.
Kim MC, Kim W, Kim HH, Ryu SW, Ryu SY, Song KY, et al. Risk factors associated with complication following laparoscopy-assisted gastrectomy for gastric cancer: a large-scale Korean multicenter study. Ann Surg Oncol. 2008;15:2692–700.
Tsou CC, Lo SS, Fang WL, Wu CW, Chen JH, Hsieh MC, et al. Risk factors and management of anastomotic leakage after radical gastrectomy for gastric cancer. Hepatogastroenterology. 2011;58:218–23.
Japanese classification of gastric carcinoma. 3rd English edition. Gastric Cancer. 2011;14:101–12.
Goseki N, Okamoto A, Onodera T. [Postoperative nutritional assessment in gastric and colorectal cancer]. Nihon Geka Gakkai Zasshi. 1986;87:853–8.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Kim W, Song KY, Lee HJ, Han SU, Hyung WJ, Cho GS. The impact of comorbidity on surgical outcomes in laparoscopy-assisted distal gastrectomy: a retrospective analysis of multicenter results. Ann Surg. 2008;248:793–9.
Jeong O, Park YK, Ryu SY, Kim YJ. Effect of age on surgical outcomes of extended gastrectomy with D2 lymph node dissection in gastric carcinoma: prospective cohort study. Ann Surg Oncol. 2010;17:1589–96.
Hwang SH, Park DJ, Jee YS, Kim HH, Lee HJ, Yang HK, et al. Risk factors for operative complications in elderly patients during laparoscopy-assisted gastrectomy. J Am Coll Surg. 2009;208:186–92.
Jeong SH, Ahn HS, Yoo MW, Cho JJ, Lee HJ, Kim HH, et al. Increased morbidity rates in patients with heart disease or chronic liver disease following radical gastric surgery. J Surg Oncol. 2010;101:200–4.
Jeong O, Ryu SY, Park YK. The value of preoperative lung spirometry test for predicting the operative risk in patients undergoing gastric cancer surgery. J Korean Surg Soc. 2013;84:18–26.
Conflict of interest
We have no conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hamakawa, T., Kurokawa, Y., Mikami, J. et al. Risk factors for postoperative complications after gastrectomy in gastric cancer patients with comorbidities. Surg Today 46, 224–228 (2016). https://doi.org/10.1007/s00595-015-1175-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-015-1175-6