Abstract
Purpose
To clarify the feasibility and utility of reduced port surgery (RPS) for achalasia.
Methods
Between September 2005 and June 2013, 359 patients with esophageal achalasia, excluding cases of reoperation, underwent laparoscopic Heller myotomy and Dor fundoplication (LHD) according to our clinical pathway. Three-hundred and twenty-seven patients underwent LHD with five incisions (conventional approach), while the other 32 patients underwent RPS, including eight via SILS. The clinical data were collected in a prospective fashion and retrospectively reviewed. We selected 24 patients matched for gender, age and morphologic type with patients in the RPS group from among the 327 patients (C group). The surgical outcomes were compared between the C and RPS groups.
Results
There were no significant differences between the two groups in the duration of symptoms, dysphagia score, chest pain score, shape of the distal esophagus and esophageal clearance. The operative time was significantly longer in the RPS group than in the C group (p < 0.001). There were no significant differences between the two groups in the length of postoperative hospital stay or rates of bleeding, mucosal injury of the esophagus and/or stomach and postoperative complications. The symptom scores significantly improved after surgery in both groups (p < 0.001). Furthermore, there were no significant differences between the C group and RPS group in terms of the postoperative symptom scores or satisfaction scores after surgery.
Conclusions
The surgical outcomes of RPS for achalasia are comparable to those obtained with the conventional method.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Achalasia is a primary esophageal functional motility disorder characterized by aperistalsis of the esophageal body and a lack of relaxation of the lower esophageal sphincter. Manometry, esophagography and functional magnetic resonance imaging [1] are useful tools for obtaining a diagnosis of achalasia. There are two main types of procedures for treating achalasia: endoscopic and surgical methods. For endoscopic treatments, dilation with an endoscopic balloon or bougie, botulinum toxin injection at the lower esophageal sphincter and per-oral endoscopic myotomy are commonly used. With respect to surgical treatments, Heller myotomy with anti-reflux surgery is generally applied. Currently, laparoscopic Heller myotomy with Dor fundoplication (LHD) is widely considered the gold standard surgical procedure [2–5]. Recently, reduced port surgery (RPS), including single-incision laparoscopic surgery (SILS), was developed to achieve cholecystectomy [6], appendectomy [7], splenectomy [8], partial gastrectomy for submucosal tumors [9], sleeve gastrectomy for obesity [10] and anterior resection of sigmoid colon cancer [11].
In our institution, we introduced LHD for achalasia in 1994 and LHD via SILS in March 2010. Eight patients have since undergone LHD via SILS. The use of SILS with an additional trocar placed under the left costal arch, so-called SILS plus one therapy, was adopted in July 2011 due to the technical difficulty of performing SILS. Because achalasia is a rare disease, with a prevalence of one in 100,000 people, the treatment outcomes of RPS, including SILS, remain unclear. Therefore, we herein report our initial surgical results to help clarify the feasibility and utility of RPS for achalasia.
Patients and methods
Patients
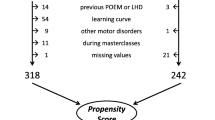
In our institution, we introduced LHD for achalasia in August 1994 and adopted it as a standard treatment in September 2005 because our surgical technique achieved the desired outcomes. Prior to June 2013, 359 patients with achalasia (excluding cases of reoperation) underwent LHD. We began utilizing SILS in young achalasia patients in March 2010 and SILS with an additional trocar placed under the left arcus costalis, the so-called SILS plus one technique, in July 2011 due to the technical difficulties of performing SILS. Consequently, 327 patients underwent LHD with five incisions (conventional approach) and 32 patients underwent RPS, including eight patients treated with SILS (Fig. 1).
Indication and surgery technique for RPS
Females 40 years of age or younger were considered good candidates for RPS due to its cosmetic advantage. In male patients 40 years or younger who wished to receive RPS, we obtained additional informed consent. The detailed surgical technique of LHD for achalasia has previously been reported [12].
Using two 12-mm trocars and three 5-mm trocars (total: five trocars), five surgical incisions were required for LHD. On the other hand, in RPS, the EZ access platform (Hakko company, Tokyo, Japan) was placed at the umbilical incision, through which three 5-mm trocars were inserted. An additional 12-mm trocar was introduced under the left costal arch at the left midclavicular line. In total, two surgical incisions were required to place four trocars according to this procedure (Figs. 2, 3). There were no differences in surgical procedures between the conventional approach and RPS. After completing myotomy comprising approximately 6 cm of the abdominal esophagus and 2 cm on the stomach side at the esophagogastric junction, we added an anti-reflux procedure (Dor fundoplication) in both groups. All short gastric vessels were divided to relieve the tension from the fundic wrap.
Methods
We collected the following data: the patient’s age, gender, symptoms, duration of symptoms, presence or absence of weight loss and history of previous treatment prior to surgery. We selected 24 patients matched for gender, age and morphologic type with the patients in the RPS group from among the 327 patients (C group).
To evaluate the condition of each patient, we conducted upper gastrointestinal Barium swallow tests to judge the shape of the distal esophagus and measure the maximal diameter of the esophagus. The shape of the distal esophagus was classified into two groups: non-sigmoid and sigmoid types. The evaluation of esophageal clearance was carried out using a timed barium esophagogram (TBE) according to a previously reported protocol [13].
The perioperative data were analyzed for the operative time, blood loss, intraoperative and postoperative complications and hospital stay. We judged the degree of symptomatic improvement and satisfaction scores at least 3 months after the surgery. The degree of dysphagia and chest pain was measured by calculating dysphagia and chest pain scores [14]. These factors were evaluated both before and after surgery.
Statistical analysis
To overcome the influence of potential confounders on selection bias, a one-to-one match was applied using a propensity score analysis. Variables involved in the propensity model were sex, age and distal shape of the esophagus. All statistical analyses were performed using the SPSS version 17 software package (SPSS, Inc., Chicago, IL, USA). The Chi-square test was used to analyze categorical variables. Mann–Whitney’s U test was used to compare continuous variables. The data are expressed as medians with the interquartile range. A p value of <0.05 was considered to be statistically significant.
Results
Background and preoperative conditions of the patients
There were no significant differences between the two groups in the duration of symptoms, dysphagia scores, chest pain scores, maximal diameter or esophageal clearance on TBE (Table 1).
Duration, bleeding, hospitalization and intraoperative and postoperative complications
There were no significant differences between the two groups in the length of postoperative hospital stay or rates of bleeding, mucosal injury of the esophagus and/or stomach and postoperative complications (Table 2).
Improvements in symptoms and satisfaction
The median postoperative follow-up period was 32 months (11–62) in the C group and eight months [3–13] in the RPS group. The follow-up period in the C group was longer than that in the RPS group.
There were no significant differences in the dysphagia scores or chest pain scores between the two groups before surgery (p = 0.462, p = 0.601). After surgery, the dysphagia scores and chest pain scores significantly improved in both groups (p < 0.001), with no significant differences between the two groups in the dysphagia scores or chest pain scores postoperatively (Table 2). No patients in the RPS group had gastroesophageal reflux symptoms, such as heartburn, after surgery, whereas three patients in the C group experienced heartburn after surgery and one patient took a proton pump inhibitor to control her symptoms. Furthermore, there were no significant differences between the groups in the satisfaction scores after surgery (p = 0.934); the patients in both groups reported excellent satisfaction. All patients in the RPS group were satisfied with their surgical incisions.
Esophageal clearance after surgery
Postoperative esophageal clearance significantly improved in both the C group and RPS group compared to that observed before surgery (p < 0.001). The 5-min complete clearance rate was 87 % in the C group and 90 % in the RPS group, with no significant differences between the two groups (Table 2).
Discussion
The etiology of achalasia is that of a primary esophageal functional motility disorder for which the cause remains unknown. The main symptoms are dysphagia and chest pain, and the quality of life of patients decreases remarkably. Because the etiology has not been identified, there is currently no curative therapy. Therefore, treatments have focused on improving the passage of food from the esophagus to the stomach to ameliorate the patient’s symptoms. The mainstay of treatment is traditionally surgery, with Heller myotomy first reported in 1914. Simple Heller myotomy is frequently associated with gastroesophageal reflux and reflux esophagitis [15]; hence, anti-reflux procedures utilizing the Dor [2–5], Toupet [5, 16], or Nissen [17] methods are often adopted. Although these procedures were originally performed via conventional laparotomy or thoracotomy, laparoscopic Heller myotomy with Dor fundoplication has been the gold standard procedure since 1991 [18]. The response rate to laparoscopic surgery is approximately 90 %, which is compatible with that of open surgery. Therefore, LHD has become the standard surgical procedure for esophageal achalasia.
On the other hand, multiport laparoscopic surgery has been slowly replaced by RPS, including SILS, for many surgical diseases with the purpose of achieving better cosmesis or minimizing surgical invasion. RPS has been utilized in cases of cholecystectomy [6], appendectomy [7], splenectomy [8], partial gastrectomy for submucosal tumors [9], sleeve gastrectomy for obesity [10] and anterior resection for sigmoid colon cancer [11].
As the lower esophagus is located in the deep intra-abdominal dorsum and the distance from a navel is far, performing LHD via SILS is difficult. Performing LHD requires a good surgical view with elevation of the lateral segment of the liver. In patients undergoing anti-reflux surgery, it is necessary to suture between the muscle of the esophagus and the fundus of the stomach with 10–15 sutures. It is not easy to perform LHD using pure SILS. Eight patients have undergone LHD via pure SILS at our institution. Because the forceps inserted through the trocars in the umbilical port frequently interfere with each other in the abdominal cavity, we adopted the placement of an additional trocar in the left costal arch in July 2011. This modification has significantly reduced the technical challenges of these procedures, as interference between the instruments is almost completely eliminated.
There are few reports of the surgical results of RPS, including SILS, for achalasia treatment. Most such reports are case reports [19–22]. For example, Barry et al. [23] published the only case series in which they performed LHD via SILS in 66 patients since October 2007. Although 11 patients required the use of an additional port or incision, there were no cases of conversion to open surgery. In addition, while the operative time was prolonged in the RPS group compared with that noted with the open conventional method, the effect of treatment was equivalent between the two groups. According to the degree of improvement in symptoms and esophgaeal clearance between before and after surgery, the outcomes of the RPS group achieved the equivalent therapeutic effect in comparison with the conventional method. Notably, there was no variance in our clinical pathway, and all patients were discharged from the hospital within 4 days after surgery. Because our postoperative observation period was short, the long-term results remain unclear. Nevertheless, although a long time follow-up period is required, RPS is superior to the conventional method due to its cosmetic advantage and good surgical outcome. RPS for esophageal achalasia may be a good choice for young people, particularly those with concerns regarding the appearance of their surgical incision. If there are no differences in long-term results between the C and RPS groups in this study, RPS is a potential candidate for the standard approach for surgical treatment in patients with esophageal achalasia.
References
Miyazaki Y, Nakajia K, Sumikawa M, Yamasaki M, Takahashi T, Miyata H, et al. Magnetic resonance imaging for simultaneous morphological and functional evaluation of esophageal motility disorders. Surg Today. 2014;44:668–76.
Tsiaoussis J, Athanasakis E, Pechlivanides G, Tzortzinis A, Gouvas N, Mantides A, et al. Long-term functional results after laparoscopic surgery for esophageal achalasia. Am J Surg. 2007;193:26–31.
Zaninotto G, Costantini M, Rizzetto C, Zanatta L, Guirroli E, Portale G, et al. Four hundred laparoscopic myotomies for esophageal achalasia: a single centre experience. Ann Surg. 2008;248:986–93.
Mattioli S, Ruffato A, Lugaresi M, Pilotti V, Aramini B, D’Ovidio F. Long-term results of the Heller-Dor operation with intraoperative manometry for the treatment of esophageal achalasia. J Thorac Cardiovasc Surg. 2010;140:962–9.
Katada N, Sakuramoto S, Yamashita K, Hosoda K, Shibata T, Moriya H, et al. Comparison of the Heller-Toupet procedure with the Heller-Dor procedure in patients who underwent laparoscopic surgery for achalasia. Surg Today. 2014;44:732–9.
Qiu J, Yuan H, Chen S, He Z, Han P, Wu H. Single-Port versus conventional multiport laparoscopic cholecystectomy: a meta-analysis of randomized controlled trials and nonrandomized studies. J Laparoendosc Adv Surg Tech A. 2013;23:815–31.
Cai YL, Xiong XZ, Wu SJ, Cheng Y, Lu J, Zhang J, et al. Single-incision laparoscopic appendectomy vs conventional laparoscopic appendectomy: systematic review and meta-analysis. World J Gastroenterol. 2013;19:5165–73.
Fan Y, Wu SD, Kong J, Su Y, Tian Y, Yu H. Feasibility and safety of single-incision laparoscopic splenectomy: a systematic review. J Surg Res. 2014;186:354–62.
Takata A, Nakajima K, Kurokawa Y, Takahashi T, Yamasaki M, Miyata H, et al. Single-incision laparoscopic partial gastrectomy for gastric submucosal tumors without compromising transumbilical stapling. Asian J Endosc Surg. 2014;7:25–30.
Mittermair R. Transumbilical single-incision laparoscopic sleeve gastrectomy: short-term results and technical considerations. J Minim Access Surg. 2013;9:104–8.
Kwag SJ, Kim JG, Oh ST, Kang WK. Single incision vs conventional laparoscopic anterior resection for sigmoid colon cancer: a case-matched study. Am J Surg. 2013;206:320–5.
Omura N, Kashiwagi H, Ishibashi Y, Yano F, Tsuboi K, Kawasaki N, et al. Laparoscopic Heller myotomy and Dor fundoplication for the treatment of achalasia: assessment in relation to morphologic type. Surg Endosc. 2006;20:210–3.
Kostic SV, Rice TW, Baker ME, DeCamp MM, Murthy SC, Rybicki LA, et al. Timed barium esophagogram: a simple physiologic assessment for achalasia. J Thorac Cardiovasc Surg. 2000;120:935–46.
Omura N, Kashiwagi H, Yano F, Tsuboi K, Ishibashi Y, Hoshino M, et al. Effect of laparoscopic esophagomyotomy on chest pain associated with achalasia and prediction of therapeutic outcomes. Surg Endosc. 2011;25:1048–53.
Burpee SE, Mamazza J, Schlachta CM, Bendavid Y, Klein L, Moloo H, et al. Objective analysis of gastroesophageal reflux after laparoscopic heller myotomy: an anti-reflux procedure is required. Surg Endosc. 2005;19:9–14.
Khajanchee YS, Kanneganti S, Leatherwood AE, Hansen PD, Swanström LL. Laparoscopic Heller myotomy with Toupet fundoplication: outcomes predictors in 121 consecutive patients. Arch Surg. 2005;140:827–34.
Rossetti G, Brusciano L, Amato G, Maffettone V, Napolitano V, Russo G, et al. A total fundoplication is not an obstacle to esophageal emptying after heller myotomy for achalasia: results of a long-term follow up. Ann Surg. 2005;241:614–21.
Shimi S, Nathanson LK, Cuschieri A. Laparoscopic cardiomyotomy for achalasia. J R Coll Surg Edinb. 1991;36:152–4.
Yamada H, Yano T. Single incision laparoscopic approach for esophageal achalasia: a case report. Int J Surg Case Rep. 2013;4:1–4.
Yano F, Omura N, Tsuboi K, Hoshino M, Yamamoto SR, Kashiwagi H, et al. Single-incision laparoscopic Heller myotomy and Dor fundoplication for achalasia: report of a case. Surg Today. 2012;42:299–302.
Kobayashi M, Mizuno M, Sasaki A, Arisue A, Akiyama S, Wakabayashi G. Single-port laparoscopic Heller myotomy and Dor fundoplication: initial experience with a new approach for the treatment of pediatric achalasia. J Pediatr Surg. 2011;46:2200–3.
Nakajima J, Sasaki A, Obuchi T, Baba S, Umemura A, Wakabayashi G. Single-incision laparoscopic Heller myotomy and Dor fundoplication for achalasia: report of a case. Surg Today. 2011;41:1543–7.
Barry L, Ross S, Dahal S, Morton C, Okpaleke C, Rosas M, et al. Laparoendoscopic single-site Heller myotomy with anterior fundoplication for achalasia. Surg Endosc. 2011;25:1766–74.
Conflict of interest
Nobuo Omura and the other co-authors have no conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Omura, N., Yano, F., Tsuboi, K. et al. Short-term surgical outcomes of reduced port surgery for esophageal achalasia. Surg Today 45, 1139–1143 (2015). https://doi.org/10.1007/s00595-014-1109-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-014-1109-8