Abstract
Purpose
To compare the efficacy and safety of single-incision laparoscopic appendectomy (SILA) and conventional 3-port laparoscopic appendectomy (3-port LA) for appendectomy.
Methods
We searched the PubMed, Embase, Springer link, and the Cochrane library databases up to April, 2014, for relevant randomized controlled trials (RCTs). Data were pooled by weighted mean differences (WMDs) or odds ratios (ORs) with their 95 % confidence intervals (CIs).
Results
We found 11 RCTs, with a collective total of 731 patients treated with SILA and 725 patients treated with 3-point LA. Results indicated no significant differences between SILA and 3-port LA in primary outcomes, including wound infection, intra-abdominal abscess, postoperative ileus, and total postoperative complications, and some secondary outcomes, including postoperative pain scores and length of hospital stay. However, SILA was associated with significantly longer operative times (WMD = 6.78, 95 % CI = 3.78–9.79, P < 0.00001) and higher doses of analgesia (WMD = 0.96, 95 % CI = 0.45–1.47, P = 0.0002) than the 3-port LA.
Conclusion
Although there was no significant difference in the safety of SILA vs. that of 3-port LA, our findings do not support the application of SILA because of its significantly longer operative times and the higher doses of analgesia required compared with those for 3-point LA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute appendicitis is one of the most common causes of acute abdominal pain [1] and appendectomy is one of the most frequently performed operations in the world. The open appendectomy procedure described in 1894 by McBurney remained the gold standard for nearly 100 years [2]. Now, conventional 3-port laparoscopic appendectomy (3-port LA) is widely acknowledged and recommended by most surgeons and the option chosen by most patients [3]. The advantages of 3-port LA over open appendectomy include less surgical trauma, a lower risk of postoperative wound infection, and reduced postoperative pain [3–5]. In addition, single-incision laparoscopic appendectomy (SILA) has been introduced in pursuit of reducing surgical trauma further [2]. SILA was first described in 1998 by Esposito [6] and is gaining popularity as a method with a perceived ‘‘scarless’’ abdomen [7]. According to a recent study, SILA resulted in faster recovery than conventional 3-port LA [8]; however, it has also been reported that SILA is associated with a longer operative time and higher postoperative pain scores, and that patients need more analgesics to feel comfortable [9–12]. Recent meta-analyses [1, 2] of related studies evaluated the clinical efficacy of SILA vs. 3-port LA and failed to find any obvious advantages of SILA over 3-port LA in perioperative and postoperative outcomes. However, the findings of more recent publications from 2013 to 2014, which were not investigated in the previous meta-analyses, remain controversial [9, 13]. The Springer link database was not retrieved in these studies; therefore, it is necessary to perform an updated meta-analysis for a more reliable and stable basis for clinical practice.
Materials and methods
Search strategy
The meta-analysis followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines. We searched PubMed, Embase, Springer link, and the Cochrane library from their inception to April 11, 2014. The main search terms entered were “single-incision”, “laparoscopic” and “appendectomy” or “appendectomies” without any language restrictions. The electronic search was supplemented by a manual search in print documents. We also searched the references of reviews and included studies to ensure that all relevant studies were checked for the meta-analysis.
Study selection
Studies were included in the meta-analysis if they met the following criteria: they were randomized controlled trials (RCTs); they compared SILA (experimental group) and 3-port LA (control group) for patients with appendicitis; and they reported data on operative time, length of hospital stay (LOS), total postoperative complications (TPC), wound infection, intra-abdominal abscess (IAA), postoperative ileus, and postoperative pain scores (PPS) or analgesia use. Studies were excluded if they were animal trials; data were incomplete or unavailable; they were non-original articles such as reviews, or letters and comments; or duplicated publications were excluded apart from the one with the most complete data.
Data extraction
Two reviewers extracted data and evaluated quality independently. The extracted information included the name of the first author, publication year, geographic region of the research, the age and gender of the patients, sample size of the experimental and control groups, and the register number of the research. Extracted tables were exchanged when the work was finished. Differences and disagreements were resolved through discussion.
We selected seven basic criteria for assessing the quality of the included studies, as suggested by the Cochrane Handbook [14]; namely, random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective outcome reporting, and other bias. This tool can help assess and detect varied bias of the studies objectively and completely.
Statistical analysis
Weighted mean differences (WMD) with a 95 % confidence interval (CI) were calculated to assess the effect size for continuous variables. Odds ratios (ORs) with a 95 % CI were used as effect size for dichotomous outcome. Heterogeneity among trials was assessed using the statistic Cochrane Q with significance set at P < 0.05 and an I 2 test with significance set at I 2 > 50 % [15, 16]. If heterogeneity was limited according to forest plotting, we used the Mantel–Haenszel fixed-effect model; if not, we used the Mantel–Haenszel random-effects model. Publication bias was evaluated by a funnel plot. Data analyses were performed using RevMan 5.2.
Results
Literature search
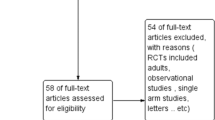
Figure 1 shows a flow diagram of the literature search. A total of 657 articles were identified from PubMed, Embase, Springer link, and the Cochrane library databases. Among them, we identified 528 references after duplicates were removed. On reviewing the titles, 491 obviously irrelevant articles were rejected. After reading the abstracts, a further 21 of the remaining 37 articles (15 retrospective studies, 2 letters, and 4 case reports) were rejected. Five references (three non-RCTs, one protocol study, and one repeated study) were then excluded by reading the full text. Finally, 11 studies [6, 7, 9, 12, 13, 17–22] were included in our meta-analysis. No additional literature was found from our manual search and references lists.
Study characteristics
A total of 11 RCTs with a collective total of 731 patients in the experimental group and 725 patients in the control group were included in this meta-analysis. The publication years of these articles were between 2010 and 2014. Ten RCTs were reported in three studies from America [7, 9, 21], five from Asia [13, 18–20, 22], and two from Europe [6, 17]. One RCT [12] was a multicentric study performed in Spain, Egypt, and Turkey. There were no significant differences in basic data such as F/M, age, body mass index (BMI), or white blood cell percent (WBC) between the experimental and control groups (Table 1).
Figure 2 shows the methodological quality of the included trials. All RCTs were judged as having a low risk of bias for all the criteria, except for the blinding of participants and personnel and blinding of outcome assessment. The total bias of the research studies was low and the quality was moderate.
Primary outcomes
The primary outcomes of this meta-analysis were postoperative complications such as wound infection, IAA, postoperative ileus, and TPC. Eight studies [6, 7, 13, 17, 18, 20–22] included a comparison of wound infection, 5 studies included a comparison of IAA [13, 18, 20–22] and postoperative ileus [9, 13, 18, 20, 22], and 11 studies [6, 7, 9, 12, 13, 17–22] included a comparison of TPC. Figure 3 shows forest plots of the pooled effect of primary outcomes.
For all the four indexes, the results of a heterogeneity test indicated that there was no significant heterogeneity among the included RCTs (I 2 = 0 %, P > 0.05). A fixed-effect model was used to synthesize all data. There were no significant differences in postoperative complications including wound infection (OR = 0.99, 95 % CI = 0.57–1.73, P = 0.97; Fig. 3a), IAA (OR = 1.63, 95 % CI = 0.67–3.97, P = 0.29; Fig. 3b), postoperative ileus (OR = 0.74, 95 % CI = 0.25–2.16, P = 0.58; Fig. 3c), and TPC (OR = 0.99, 95 % CI = 0.67–1.46, P = 0.95; Fig. 3d) between SILA and 3-port LA.
Secondary outcomes
The secondary outcomes of the meta-analysis included operative time, LOS, PPS, and analgesia use. Figure 4 shows forest plots of the pooled effect of secondary outcomes. Eleven studies [6, 7, 9, 12, 13, 17–22] compared operative times and significant heterogeneity among these RCTs was found (I 2 = 78 %, P < 0.00001). A random-effects model was used to synthesize data and the results showed that SILA was associated with significant longer operative times than 3-port LA (WMD = 6.78, 95 % CI = 3.78–9.79, P < 0.00001; Fig. 4a). Nine studies [6, 9, 12, 13, 17–19, 21, 22] compared the LOS between the two groups and no significant heterogeneity among these RCTs was found (I 2 = 0 %, P = 0.5). A fixed-effect model was then used to synthesize all data. The results showed no significant difference in LOS between the experimental and control groups (OR = 0.00, 95 % CI = −0.05–0.04, P = 0.90; Fig. 4b).
For PPS, three papers [6, 13, 17] reported on pain scores in the first 12 h postoperatively and two papers [9, 12] reported on pain scores in the first 24 h postoperatively. There was significant heterogeneity among the studies analyzing the pain scores in the first 12 (I 2 = 82 %, P = 0.004) and 24 h postoperatively (I 2 = 81 %, P = 0.0003). A random-effects model was used to synthesize data. Subgroup analysis indicated that there was no significant difference in pain scores in the first 12 h (WMD = −0.34, 95 % CI = −1.02–0.33, P = 0.32) or the first 24 h (WMD = 0.35, 95 % CI = −0.62–1.33, P = 0.48) between the experimental and control groups (Fig. 4c).
Two papers [6, 13] also studied the frequency of analgesia use and three papers [9, 21, 22] studied the total doses of analgesic agents given. There was no significant heterogeneity among the studies in the analysis of analgesia use (I 2 = 0, P = 0.63) or in the total doses of analgesic agents given (I 2 = 0, P = 0.48). A fixed-effect model was used to synthesize data. Subgroup analysis indicated that there was no significant difference in the frequency of analgesia between the groups (OR = −0.13, 95 % CI = −0.44–0.18, P = 0.41). However, the total doses of analgesics used in experimental group was significantly higher than that in the control group (WMD = 0.96, 95 % CI = 0.45–1.47, P = 0.0002; Fig. 4d).
Publication bias
Funnel plots were used to evaluate the possibility of a publication bias. The scatter-distributed shapes of the funnel plots for operative time did not reveal asymmetry, indicating no evidence of publication bias (Fig. 5; other data not shown).
Discussion
According to our meta-analysis of 11 RCTs, all primary outcomes (namely, wound infection, IAA, postoperative ileus, and TPC) of SILA were similar to those of 3-port LA; consistent with the results of previous meta-analyses [1, 2]. Moreover, the safety of SILA was equivalent to that of 3-Point LA. However, there were significant differences in the secondary outcomes of operative time and analgesia between the two procedures. The operative times were significantly longer and the doses of analgesia were significantly higher for the patients treated with SILA than for those treated with 3-point LA. The characteristic single incision of SILA would increase its technical difficulty because all surgical procedures have to be performed in one working channel [2, 19, 23]. Thus, a longer operative time would be needed for SILA than for 3-point LA. Furthermore, the location of the SILA incision is close to the umbilicus where nerves are more sensitive than in the rest of the abdomen [23, 24]. This may inflict more pain during the operation, resulting in the need for a higher dose of analgesic medication to control pain in SILA patients vs. that needed for 3-point LA patients.
In view of these findings, the operative method selected should be based on the patient preference, the surgeon’s decision, and the availability of laparoscopic instruments. It was also pointed out that the timing of appendectomy for acute appendicitis can influence clinical outcomes, with a delay in performing appendectomy of more than 24 h from the onset of symptoms increasing the rate of complications [25]. Thus, the timing of appendectomy and the surgeon’s experience should also be considered.
Although SILA is more time-consuming, its advantages should not be ignored. SILA is appropriate for patients who desire the optimal cosmetic result because it is “scarless” surgery. Most researchers found that the cosmetic scores given by patients undergoing SILA was higher than that given by patients undergoing the classic procedure [2, 19]. Conversely, others reported that the cosmetic satisfaction score and postoperative pain scores were not significantly different between SILA and 3-port LA [18], which may be attributed to limited experience of the surgeon. Further randomized trials are needed to assess the cosmetic results of SILA. With the development of the SILA technique, the clinical outcomes might be improved, which would be reflected not only in the cosmetic results, but in other outcomes as well. Hence, updated investigations should be continued for further confirmation of the findings of this study.
The results of this updated meta-analysis confirmed the earlier findings on the efficacy and safety of SILA vs. 3-port LA. Compared with previous studies, our meta-analysis included some recent articles such as the research done by Carter et al. [9], Vilallonga et al. [12] and Pan et al. [19]. There were still no significant differences between the experimental and control groups in some basic data such as F/M, age, BMI, and WBC in all the included studies. Thus, the influence of these confounding factors on the results would be reduced and our conclusions may be more reliable than those of the former studies. However, there are also several disadvantages in our meta-analysis which could influence our results. First, significant heterogeneity was found in this study, which may be attributed to the different cultures, ethnicity and region in each study; thus, further studies are required to explore sources of heterogeneity. Second, the lack of data on satisfaction about the operative scar in this study did not allow us to compare SILA and 3-port LA in relation to wound cosmesis and satisfaction. Hence, an investigation of the other outcomes of SILA vs. 3-port LA should be performed by RCTs.
In conclusion, although there was no significant difference in the safety of SILA vs. 3-point LA, our findings do not support the application of SILA because of the significantly longer operative time and higher dose of analgesia required compared with 3-point LA. Further investigations are warranted to verify the findings of this study.
References
Hua J, Gong J, Xu B, Yang T, Song Z. Single-incision versus conventional laparoscopic appendectomy: a meta-analysis of randomized controlled trials. J Gastrointest Surg. 2014;18:426–36.
Gao J, Li P, Li Q, Tang D, Wang DR. Comparison between single-incision and conventional three-port laparoscopic appendectomy: a meta-analysis from eight RCTs. Int J Colorectal Dis. 2013;28:1319–27.
Fahrner R, Schob O. Laparoscopic appendectomy as a teaching procedure: experiences with 1,197 patients in a community hospital. Surg Today. 2012;42:1165–9.
Katsuno G, Nagakari K, Yoshikawa S, Sugiyama K, Fukunaga M. Laparoscopic appendectomy for complicated appendicitis: a comparison with open appendectomy. World J Surg. 2009;33:208–14.
Ohtani H, Tamamori Y, Arimoto Y, Nishiguchi Y, Maeda K, Hirakawa K. Meta-analysis of the results of randomized controlled trials that compared laparoscopic and open surgery for acute appendicitis. J Gastrointest Surg. 2012;16:1929–39.
Sozutek A, Colak T, Dirlik M, Ocal K, Turkmenoglu O, Dag A. A prospective randomized comparison of single-port laparoscopic procedure with open and standard 3-port laparoscopic procedures in the treatment of acute appendicitis. Surg Laparosc Endosc Percutan Tech. 2013;23:74–8.
Perez EA, Piper H, Burkhalter LS, Fischer AC. Single-incision laparoscopic surgery in children: a randomized control trial of acute appendicitis. Surg Endosc. 2013;27:1367–71.
Amos SE, Shuo-Dong W, Fan Y, Tian Y, Chen CC. Single-incision versus conventional three-incision laparoscopic appendectomy: a single centre experience. Surg Today. 2012;42:542–6.
Carter JT, Kaplan JA, Nguyen JN, Lin MY, Rogers SJ, Harris HW. A prospective, randomized controlled trial of single-incision laparoscopic vs conventional 3-port laparoscopic appendectomy for treatment of acute appendicitis. J Am Coll Surg. 2014;218:950–9.
Raman JD, Bagrodia A, Cadeddu JA. Single-incision, umbilical laparoscopic versus conventional laparoscopic nephrectomy: a comparison of perioperative outcomes and short-term measures of convalescence. Eur Urol. 2009;55:1198–206.
Saber AA, El-Ghazaly TH, Elain A, Dewoolkar AV. Single-incision laparoscopic placement of an adjustable gastric band versus conventional multiport laparoscopic gastric banding: a comparative study. Am Surg. 2010;76:1328–32.
Vilallonga R, Barbaros U, Nada A, Sümer A, Demirel T, Fort JM, et al. Single-port transumbilical laparoscopic appendectomy: a preliminary multicentric comparative study in 87 patients with acute appendicitis. Minim Invasive Surg. 2012;2012:492409.
Kye B-H, Lee J, Kim W, Kim D, Lee D. Comparative study between single-incision and three-port laparoscopic appendectomy: a prospective randomized trial. J Laparoendosc Adv Surg Tech A. 2013;23:431–6.
Higgins JP, Green S. Cochrane handbook for systematic reviews of interventions, vol. 5. Wiley Online Library; 2008.
Liu YJ, Zhan J, Liu XL, Wang Y, Ji J, He QQ. Dietary flavonoids intake and risk of type 2 diabetes: a meta-analysis of prospective cohort studies. Clin Nutr. 2014;33:59–63.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. Br Med J. 2003;327:557–60.
Frutos MD, Abrisqueta J, Lujan J, Abellan I, Parrilla P. Randomized prospective study to compare laparoscopic appendectomy versus umbilical single-incision appendectomy. Ann Surg. 2013;257:413–8.
Lee W-S, Choi ST, Lee JN, Kim KK, Park YH, Lee WK, et al. Single-port laparoscopic appendectomy versus conventional laparoscopic appendectomy: a prospective randomized controlled study. Ann Surg. 2013;257:214–8.
Pan Z, Jiang XH, Zhou JH, Ji ZL. Transumbilical single-incision laparoscopic appendectomy using conventional instruments: the single working channel technique. Surg Laparosc Endosc Percutan Tech. 2013;23:208–11.
Park JH, Hyun KH, Park CH, Choi SY, Choi WH, Kim DJ, et al. Laparoscopic vs transumbilical single-port laparoscopic appendectomy; results of prospective randomized trial. J Korean Surg Soc. 2010;78:213–8.
St Peter SD, Adibe OO, Juang D, Sharp SW, Garey CL, Laituri CA, et al. Single incision versus standard 3-port laparoscopic appendectomy: a prospective randomized trial. Ann Surg. 2011;254:586–90.
Teoh AY, Chiu PW, Wong TC, Poon MC, Wong SK, Leong HT, et al. A double-blinded randomized controlled trial of laparoendoscopic single-site access versus conventional 3-port appendectomy. Ann Surg. 2012;256:909–14.
Cuschieri A. Single-incision laparoscopic surgery. J Minim Access Surg. 2011;7:3.
Silen W. In Abdominal Pain. In: Kasper DL, Fauci AS, Longo DL, Braunwald E, Hauser SL, Jameson JL, editors. Harrison’s Principles of Internal Medicine. New York: McGraw Hill; 2005.
Giraudo G, Baracchi F, Pellegrino L, Dal Corso HM, Borghi F. Prompt or delayed appendectomy? Influence of timing of surgery for acute appendicitis. Surg Today. 2013;43:392–6.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Xue, C., Lin, B., Huang, Z. et al. Single-incision laparoscopic appendectomy versus conventional 3-port laparoscopic appendectomy for appendicitis: an updated meta-analysis of randomized controlled trials. Surg Today 45, 1179–1186 (2015). https://doi.org/10.1007/s00595-014-1094-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-014-1094-y