Abstract
Background and purpose
Two types of neuromodulation are currently practised for the treatment of fecal incontinence (FI): sacral nerve stimulation (SNS) and percutaneous tibial nerve stimulation (PTNS). This study compares these therapies, as no data exist to prospectively assess their relative efficacy and costs.
Methods
The subjects of this study were two distinct cohorts undergoing SNS (between 2003 and 2008) or PTNS (2008-onwards) for FI. Clinical outcomes assessed at 3 months included incontinence scores and the number of weekly incontinence episodes. The direct medical costs for each procedure were calculated from the audited expenditure of our unit.
Results
Thirty-seven patients (94.6 % women) underwent permanent SNS and 146 (87.7 % women) underwent PTNS. The mean pre-treatment incontinence score (±SD) was greater in the SNS cohort (14 ± 4 vs. 12 ± 4) and the mean post-treatment incontinence scores were similar for the two therapies (9 ± 5 vs. 10 ± 4), with a greater effect size evident in the SNS patients. In a ‘pseudo case–control’ analysis with 37 “matched” patients, the effect of both treatments was similar. The cost of treating a patient for 1 year was £11 374 ($18 223) for permanent SNS vs. £1740 ($2784) for PTNS.
Conclusion
Given the lesser cost and invasive nature of PTNS, where both techniques are available, a trial of PTNS could be considered for all patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fecal incontinence (FI) is an important condition that compromises quality of life with considerable socioeconomic implications for health services worldwide [1, 2]. It is thought that 10 % of all adults experience some degree of involuntary loss of stool or flatus, although this may be a conservative estimate, given significant under-reporting [3]. Furthermore, considering the much greater prevalence of this condition in older age groups, its impact on health care resources may become more significant as the demographics of western nations shift toward older populations [4–7].
The treatment of FI initially involves conservative measures, including dietary modifications, anti-motility and constipating medications, pelvic floor physiotherapy, and sensory retraining [8]. Unfortunately, these therapies are unsuccessful in about half of the patients, prompting consideration of surgical sphincter repair and, occasionally, augmentation using artificial bowel sphincter or electrically stimulated gracilis neosphincter (ESGN) [5, 9–11]. However, these interventions are complex, have variable outcomes, and carry significant morbidity including the eventual recourse to a permanent stoma.
Pelvic nerve neuromodulation by sacral nerve stimulation (SNS) has been used worldwide since 1995 as treatment for FI, with acceptable success rates and satisfaction, irrespective of anal sphincter morphology [12–14]. SNS is a minimally invasive procedure with success rates between 50 and 70 % and low morbidity, commonly in the form of reversible pains or abnormal sensation, which can usually be rectified by reprogramming. It does, however, require two operations by specialist surgeons, with significant cost implications [15–19]. Despite these caveats, it is recommended by the National Institute of Clinical Excellence in the United Kingdom for the treatment of patients who are not candidates for sphincter repair.
Indirect modulation of the pelvic nerves using percutaneous tibial nerve stimulation (PTNS) has the advantages of avoiding an operation, and being even less invasive, almost complication-free, and potentially more cost-effective. However, data on the efficacy of PTNS are limited mainly to a few small case series with relatively short follow-up [2, 20–26]. Furthermore, little is known about the relative efficacy of the two treatments, whether one therapy should be administered first, or whether patients could be stratified on baseline characteristics to one treatment over the other. While a definitive randomized controlled trial comparing the two therapies will be required to answer these questions, prospective clinical audit data can provide estimates of effect size that may influence future study design.
Methods
Patients
The subjects of this study were patients referred to an academic surgical unit with FI refractory to conservative measures. All patients were assessed clinically and, when indicated, by endoscopic examination to exclude an underlying organic cause of their symptoms. Pre-treatment assessment also included quantification of incontinence using the Cleveland Clinic Florida-Fecal Incontinence (CCF-FI) questionnaire and completion of a bowel diary, prospectively, for 2 weeks. Detailed anorectal physiologic assessment was also performed, including manometric assessment of sphincter pressures and endo-anal ultrasonography of the sphincter complex.
Interventions
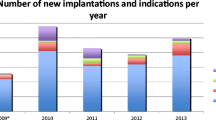
From 2003 to 2008, when PTNS was not available, suitable patients with refractory FI were offered SNS, which was performed according to the standard two-stage procedure protocol [13]. Under general or local anesthetic, patients underwent unilateral peripheral nerve evaluation (PNE) with the percutaneous insertion of a stimulating electrode into the S3 sacral foramen (3065USC, Medtronic, Minneapolis, MN). The test electrode was kept in situ for 2 weeks, following which a permanent implant (3023, Interstim I, Medtronic) was offered to all patients who demonstrated a 50 % reduction in FI episodes and expressed their satisfaction with treatment. From 2008 onwards, the first-line neuromodulation therapy in our institution changed to PTNS, which was performed over 12 nurse-led outpatient sessions, using a hand-held neuromodulation device (Urgent PC, Uroplasty, Manchester, UK). The technique and protocol used in our unit were described in detail previously [2].
Clinical outcomes
The outcomes assessed in all patients were as follows: the CCF-FI score [27]; the ability to defer defecation (deferment time); and the number of weekly incontinence episodes, documented in standard 2-week bowel diaries [28]. Outcomes were assessed prospectively after 2 weeks for patients who underwent temporary SNS (PNE) and after 3 months following the insertion of a permanent implant. Similarly, clinical outcomes were assessed prospectively for all PTNS patients at baseline and following 12 treatment sessions that were completed within a 3-month period. Changes in clinical outcomes between the baseline and the 3-month assessment were calculated. The direct medical costs associated with each procedure for the first year of therapy were calculated from the audited expenditure in our department. The expense associated with each treatment modality over a 10-year period was also estimated from current expenditure costs using conservative estimates about the type of follow-up and clinical input usually required by such patients in our institution. The 10-year time frame was chosen because the need for a replacement battery must be included in the projected costs of SNS when it is offered to patients.
Statistical analyses
Pre- and post-treatment data for both cohorts (each therapy) were analyzed using proprietary software and presented according to data distribution as the mean and standard deviation (normal) or the median and range (non-normal). Differences in baseline characteristics were analyzed using basic categorical and ordinal hypothesis tests. Crude estimates of effect sizes of each index therapy were calculated using the difference between the mean CCF-FI scores pre- and post-treatment divided by the standard deviation pre-treatment.
To compensate for the lack of randomisation and the fact that the two cohorts were treated over two different time periods, a statistical sub-analysis (using a 1–1 ‘pseudo case–control’ model) was performed by matching all patients in the SNS cohort with selected PTNS patients for age, gender, and pre-treatment CCF-FI scores. Normally distributed data were compared using unpaired t tests, whereas the Mann–Whitney U test was used to compare non-normal data. A p value of <0.05 was considered significant.
Results
Patients
Fifty consecutive patients (47F:3M) with FI refractory to conservative measures underwent PNE over a 5-year period (2003–2008). Thirty-seven (74.0 %) patients reported ≥50 % reduction in FI episodes and proceeded to permanent SNS. Patients who underwent permanent SNS were predominantly female (n = 35; 94.6 %) with a median age of 48 years (range 31–84) for the cohort as a whole. A traumatic event (n = 23 obstetric, n = 8 iatrogenic, n = 2 other trauma) was the predominant underlying cause of FI in 33 (89.0 %) patients, while no clear cause was established in 4 patients (idiopathic, 11.0 %; Table 1).
From 2008 to the time of writing, 146 patients underwent a course of PTNS as first-line neuromodulation treatment. They were predominantly female (n = 128; 87.7 %) with a median age of 56 years (range 15–83). The underlying cause was believed to be traumatic (n = 88 obstetric, n = 23 iatrogenic, n = 6 other trauma) in 117 (80.1 %) patients, while the incontinence was classified as idiopathic in 27 (18.5 %), and was attributed to post-radiation damage in 2 (1.4 %).
Table 1 summarizes the pre-treatment anorectal physiology data for the two cohorts. No statistical difference was seen between the demographic and baseline anorectal physiological characteristics of the two groups, with the exception of the median maximum squeeze pressure, which was lower in patients who underwent permanent SNS.
Pre-treatment assessment
The mean pre-treatment CCF-FI score (±standard deviation) for patients who underwent permanent SNS was greater than the mean pre-PTNS incontinence score (14 ± 4 vs. 12 ± 4; Table 2). Patients who underwent permanent SNS also had more weekly incontinence episodes before treatment than patients receiving PTNS [15 (0–53) vs. 4 (0–35)]. No difference was seen in the median pre-treatment deferment time (1 min) between the cohorts.
Functional outcome following neuromodulation
Post-treatment CCF-FI scores were similar for the cohorts [9 ± 5 (SNS) vs. 10 ± 4 (PTNS)] but the mean change in the incontinence score [5 ± 4 (SNS) vs. 3 ± 4 (PTNS)] and calculated effect size [1.2 (SNS) vs. 0.7 (PTNS)] were greater in the patients treated with SNS. Post-treatment incontinence episode frequencies were also similar in the SNS and PTNS cohorts [2 (0–19) vs. 1 (0–27), respectively] but because of the pre-treatment difference, the reduction in frequency was greater in the SNS patients [11 (0–48) vs. 2 (0–29), respectively]. Both therapies resulted in a 4-min improvement in the deferment time (Table 2).
Sub-analysis using a ‘pseudo’ case–control model
In a 1–1 ‘pseudo case–control’ model, matching patients for age, gender and pre-treatment CCF-FI score, the calculated effect size was almost identical between the cohorts, at 1.2 for the SNS group vs. 1.3 for the PTNS group (Table 3). Pre-treatment incontinence episodes remained higher for the SNS patients [15 (0–53) vs. 7 (0–30), respectively; p = 0.02; Table 3], but they did not differ following either treatment [2 (0–19) vs. 1 (0–16), respectively (p = 0.27)]. Furthermore, a median reduction in incontinence episodes was statistically similar between the cohorts, at 11 (0–48) for the SNS group vs. 5 (7–29) for the PTNS group (p = 0.07). Finally, no difference was seen in the pre- and post-treatment deferment times when comparing the two therapies.
Treatment costs
In a center with a pre-existing specialist nursing service, an additional set up cost of £1043 ($1668) for the PTNS programmer is required. This can be used for up to 70 individual sessions in a standard working week, meaning that the cost of the device per patient session can be calculated as £1043/70 = £15 ($24). Additional expenditure includes disposable electrodes [£40 ($64)/electrode], the time spent with the nurse [£46 ($74)/session] and outpatient running costs, such as the keeping of medical records, reception staff, clinical space, and other consumables, at £15 [24] /session; Table 4). In total, the cost of PTNS per patient for the first year of treatment involving 15 sessions was estimated to be £1740 ($2784). Additionally, the theoretical projected cost of PTNS for each subsequent year of treatment involving four maintenance/“top-up” sessions, as two sessions every 6 months, according to the standardized protocol [2] is approximately £464 ($742). Consequently, the total PTNS cost per patient for the first 10 years is estimated to be approximately £5916 ($9466).
The cost of PNE included operating theatre time [£8 ($13)/min or £480 ($780) for a 60-min session], the cost of the PNE electrode (£254/$407), time of the surgeon [£100 ($160)/session], 1 day in hospital (£250/$400), outpatient costs (including time with the surgeon), and running costs [£80 ($128)/session; Table 5]. This equated to £1,164 ($1875), including one outpatient appointment to assess the success of PNE and determine whether the patient could proceed to permanent SNS. For patients who underwent permanent SNS, there was an additional cost for the stimulator [3023, Interstim I, Medtronic, £9300 ($14,880)]. Thus, the total expenditure with operating theatre time at £8 ($13)/min or £480 ($780) for a 60-min session, 1 day in hospital (£250/$400), surgeon time, operating theatre time/outpatient review, and outpatient running costs was £10,210 ($16,348; Table 5) and the total cost of SNS for year 1 was £11,374 ($18,223). Furthermore, the cost of treatment in subsequent years is £160 ($256) to cover the cost of two outpatient sessions 6-monthly [£80 ($128)/session] and £7,670 ($12,272) to cover the costs for replacing the stimulator battery after 7 years [£6,840 ($10,944) for the device, £480 ($780) for operating theatre time, £100 ($160) for time with the surgeon, and £250 ($400) for 1 day in hospital]. In total, the estimated expenditure for PNE and permanent SNS per patient for the first 10 years of treatment is £20,484 ($32,775).
Discussion
In this prospective clinical audit, which, to our knowledge, is the first to assess the outcome of two neuromodulatory therapies for FI, both SNS and PTNS resulted in acceptable improvements in clinical measures at 3 months. In particular, SNS resulted in a 5-unit improvement in the CCF-FI score, with prolongation of the deferment time by 4 min and fewer incontinence episodes by a median of 11 per week. Similarly, PTNS improved the CCF-FI score by 3 units, the deferment time by 4 min and the frequency of incontinence episodes by a median of two per week. These improvements are comparable to the results of previous studies, although direct comparison is difficult due to the assessments being performed at various follow-up intervals. Nevertheless, SNS studies with short follow-up to 6 months demonstrated improved CCF-FI scores by 3–12 units and 2–9 fewer incontinence episodes per week [29–35]. Similarly, previous PTNS studies reported 4–5 unit improvement in the incontinence score and 3–6 fewer weekly incontinence episodes after 3 months [24, 26, 36].
The apparent greater improvement in measurable outcomes following SNS might be attributed to its greater efficiency. Pre-treatment assessment of the SNS and PTNS patients revealed higher CCF-FI scores and frequency of incontinence episodes for the SNS cohort, with greater potential for a more marked effect. When the SNS patients were matched to 37 PTNS patients for age, gender, and pre-treatment incontinence score, in a ‘pseudo case–control’ sub-analysis, the two therapies produced statistically similar changes in the measurable parameters, with almost identical effect size, although the SNS cohort still had statistically more incontinence episodes before treatment.
Calculation of direct medical expenditure associated with the two therapies revealed different costs, with SNS being significantly more expensive after the first year of treatment and when the projected 10-year costs were estimated. Our unit’s expenditure on PNE and permanent SNS for the first year of treatment was similar to that reported by other international investigators [37, 38]. Following the introduction of PTNS, which is less invasive and potentially equally efficacious, the practice of offering SNS to patients without first treating them with PTNS has to be questioned. Furthermore, in the United Kingdom, SNS requires an individual funding application to the appropriate health authority with potential long delays before the procedure can take place. Consequently, this time period can be used to evaluate the efficacy of PTNS prior to proceeding to SNS.
It has been suggested that SNS has a significant advantage over alternative surgical techniques because its efficacy can be evaluated prior to insertion of a permanent implant [16]. This is important as the procedure does not result in significant continence score improvements for every patient with FI [12]. In our study, thirteen patients (26 %) were not eligible for permanent stimulation because of inadequate response, which is comparable with the results of previous studies [12]. The associated expenditure for these patients who failed to progress to permanent SNS was £15,132 ($24,211).The significant cost associated with PNE failure could potentially be reduced using PTNS as an ‘evaluating tool’ to assess the neuromodulatory response in a more cost-effective way. This hypothesis clearly requires a large number of patients and correlation of their baseline physiological characteristics to the outcome of the neuromodulatory process, to stratify or even predict the neuromodulatory response.
Despite the prospective nature of the data, we need to discuss two main limitations. First, this study assesses patient cohorts that were not randomized and were treated during two different time periods. Consequently, a significant degree of selection bias cannot be excluded, with further uncertainty created by the fact that SNS patients for whom PNE failed were excluded from the final analysis. In addition, the cohorts had statistically different pre-treatment squeeze pressures and symptom severity. We attempted to minimize the input of these factors by performing a ‘pseudo case–control’ subgroup analysis, but any conclusions need to be interpreted with caution and require further validation. Nevertheless, the ongoing NIHR randomized mixed methods pilot study (phase II exploratory trial, UKCRN ID 10479) comparing SNS and PTNS will provide definitive data regarding their relative effectiveness, costs, and patient acceptability. A second limitation of this study is the lack of published data on the long-term efficacy of PTNS. Consequently, the projected 10-year costs need to be interpreted with a degree of caution since some patients may require therapy sessions more frequently than the recommended 6-monthly intervals. Furthermore, approximately 20 % of patients do not derive an adequate benefit from PTNS and require subsequent treatment with SNS [39]. Despite these caveats, previously published data from our unit show that 97 % of patients complete the initial course of 12 therapy sessions, with 80 % continuing with the treatment in the long-term, with significant improvements in clinical and quality of life scores [40]. In addition, the cost of PTNS may be reduced further if it is delivered outside a specialist colorectal unit; for example, in a community setting.
In conclusion, based on the findings of this prospective clinical audit, SNS and PTNS both improve fecal incontinence symptoms, at least in the short-term, although whether they have comparable efficacy and longevity remains unconfirmed. Nevertheless, as reported previously by others, SNS has a greater impact on service provision in view of its expense and the need for a specialist colorectal team to deliver this treatment. In the current climate of fiscal uncertainty and limited healthcare resources, the choice of therapy for refractory FI must be justified. Until the results of ongoing prospective randomized trials are available, these data suggest that all patients with persistent FI should be treated, or at least offered, PTNS, and only if this fails, should they proceed to treatment with SNS.
Author contribution
AH: study conception and design acquisition, analysis and interpretation of data, writing manuscript; JM: acquisition, analysis and interpretation of data, writing manuscript; MA: acquisition of data, analysis and interpretation of data, writing manuscript; AC: acquisition of data, analysis and interpretation of data, writing manuscript; NSW: acquisition, analysis and interpretation of data, writing manuscript; CHK: acquisition, analysis and interpretation of data, writing manuscript; CLC: Study conception and design, acquisition, analysis and interpretation of data, writing manuscript.
References
Sung VW, Rogers ML, Myers DL, Akbari HM, Clark MA. National trends and costs of surgical treatment for female fecal incontinence. Am J Obstet Gynecol. 2007;197(652):e1–5.
Hotouras A, Allison M, Currie A, Knowles CH, Chan CL, Thaha MA. Percutaneous tibial nerve stimulation for fecal incontinence: a video demonstration. Dis Colon Rectum. 2012;55:711–3.
Navarro JM, Arroyo Sebastian A, Perez Vicente F, Sanchez Romero AM, Perez Legaz J, et al. Sacral root neuromodulation as treatment for fecal incontinence. Preliminary results. Revista espanola de enfermedades. 2007;99:636–42.
Matzel KE, Kamm MA, Stosser M, Baeten CG, Christiansen J, et al. Sacral spinal nerve stimulation for faecal incontinence: multicentre study. Lancet. 2004;363:1270–6.
Brown SR, Wadhawan H, Nelson RL. Surgery for faecal incontinence in adults. Cochrane Database Syst Rev. 2010;9:CD001757.
Melenhorst J, Koch SM, Uludag O, van Gemert WG, Baeten CG. Is a morphologically intact anal sphincter necessary for success with sacral nerve modulation in patients with faecal incontinence? Colorectal Dis. 2008;10(3):257–62.
Griffin KM, Pickering M, O’Herlihy C, O’Connell PR, Jones JF. Sacral nerve stimulation increases activation of the primary somatosensory cortex by anal canal stimulation in an experimental model. Br J Surg. 2011;98:1160–9.
Allison M. Percutaneous tibial nerve stimulation for patients with faecal incontinence. Nurs Stand. 2011;25:44–8.
Malouf AJ, Vaizey CJ, Norton CS, Kamm MA. Internal anal sphincter augmentation for fecal incontinence using injectable silicone biomaterial. Dis Colon Rectum. 2001;44:595–600.
Wong WD, Congliosi SM, Spencer MP, Corman ML, Tan P, et al. The safety and efficacy of the artificial bowel sphincter for fecal incontinence: results from a multicenter cohort study. Dis Colon Rectum. 2002;45:1139–53.
Tillin T, Gannon K, Feldman RA, Williams NS. Third-party prospective evaluation of patient outcomes after dynamic graciloplasty. Br J Surg. 2006;93:1402–10.
Dudding TC, Pares D, Vaizey CJ, Kamm MA. Predictive factors for successful sacral nerve stimulation in the treatment of faecal incontinence: a 10-year cohort analysis. Colorectal Dis. 2008;10:249–56.
Boyle DJ, Murphy J, Gooneratne ML, Grimmer K, Allison ME, et al. Efficacy of sacral nerve stimulation for the treatment of fecal incontinence. Dis Colon Rectum. 2011;54:1271–8.
Matzel KE, Stadelmaier U, Hohenfellner M, Gall FP. Electrical stimulation of sacral spinal nerves for treatment of faecal incontinence. Lancet. 1995;346:1124–7.
Hetzer FH, Bieler A, Hahnloser D, Lohlein F, Clavien PA, Demartines N. Outcome and cost analysis of sacral nerve stimulation for faecal incontinence. Br J Surg. 2006;93:1411–7.
Dudding TC, Meng Lee E, Faiz O, Pares D, Vaizey CJ, et al. Economic evaluation of sacral nerve stimulation for faecal incontinence. Br J Surg. 2008;95:1155–63.
George AT, Kalmar K, Panarese A, Dudding TC, Nicholls RJ, Vaizey CJ. Long-term outcomes of sacral nerve stimulation for fecal incontinence. Dis Colon Rectum. 2012;55:302–6.
Matzel KE. Sacral nerve stimulation for faecal incontinence: its role in the treatment algorithm. Colorectal Dis. 2011;13(Suppl 2):10–4.
Tjandra JJ, Lim JF, Matzel K. Sacral nerve stimulation: an emerging treatment for faecal incontinence. ANZ J Surg. 2004;74:1098–106.
Shafik A, Ahmed I, El-Sibai O, Mostafa RM. Percutaneous peripheral neuromodulation in the treatment of fecal incontinence. Eur Surg Res. 2003;35:103–7.
Mentes BB, Yuksel O, Aydin A, Tezcaner T, Leventoglu A, Aytac B. Posterior tibial nerve stimulation for faecal incontinence after partial spinal injury: preliminary report. Tech Coloproctol. 2007;11:115–9.
Boyle DJ, Prosser K, Allison ME, Williams NS, Chan CL. Percutaneous tibial nerve stimulation for the treatment of urge fecal incontinence. Dis Colon Rectum. 2010;53:432–7.
Findlay JM, Yeung JM, Robinson R, Greaves H, Maxwell-Armstrong C. Peripheral neuromodulation via posterior tibial nerve stimulation - a potential treatment for faecal incontinence? Ann R Coll Surg Eng. 2010;92:385–90.
Govaert B, Pares D, Delgado-Aros S, La Torre F, Van Gemert WG, Baeten CG. A prospective multicentre study to investigate percutaneous tibial nerve stimulation for the treatment of faecal incontinence. Colorectal Dis. 2010;12:1236–41.
Hotouras A, Thaha MA, Boyle D, Allison ME, Currie A, et al. Short-term outcome following percutaneous tibial nerve stimulation (PTNS) for faecal incontinence: a single-centre prospective study. Colorectal Dis. 2012;14:1101–5.
de la Portilla F, Rada R, Vega J, Gonzalez CA, Cisneros N, Maldonado VH. Evaluation of the use of posterior tibial nerve stimulation for the treatment of fecal incontinence: preliminary results of a prospective study. Dis Colon Rectum. 2009;52:1427–33.
Jorge JM, Wexner SD. Etiology and management of fecal incontinence. Dis Colon Rectum. 1993;36:77–97.
Medtronic. Patient diary, version 1.0. Minneapolis. 2001.
Otto SD, Burmeister S, Buhr HJ, Kroesen A. Sacral nerve stimulation induces changes in the pelvic floor and rectum that improve continence and quality of life. J Gastrointest Surg. 2010;14:636–44.
Hetzer FH, Hahnloser D, Clavien PA, Demartines N. Quality of life and morbidity after permanent sacral nerve stimulation for fecal incontinence. Arch Surg. 2007;142:8–13.
Michelsen HB, Buntzen S, Krogh K, Laurberg S. Rectal volume tolerability and anal pressures in patients with fecal incontinence treated with sacral nerve stimulation. Dis Colon Rectum. 2006;49:1039–44.
Leroi AM, Parc Y, Lehur PA, Mion F, Barth X, Rullier E, et al. Efficacy of sacral nerve stimulation for fecal incontinence: results of a multicenter double-blind crossover study. Ann Surg. 2005;242:662–9.
Rasmussen OO, Buntzen S, Sorensen M, Laurberg S, Christiansen J. Sacral nerve stimulation in fecal incontinence. Dis Colon Rectum. 2004;47:1158–62 (discussion 62–3).
Soria-Aledo V, Mengual-Ballester M, Pellicer-Franco E, Aguayo-Albasini JL. Improvement in the quality of life of faecal incontinent patients after sacral root stimulation treatment]. Cirugia espanola. 2011;89:581–7.
Uludag O, Koch SM, Vliegen RF, Dejong CH, van Gemert WG, Baeten CG. Sacral neuromodulation: does it affect the rectoanal angle in patients with fecal incontinence? World J Surg. 2010;34:1109–14.
Hotouras A, Thaha MA, Allison ME, Currie A, Scott SM, Chan CL. Percutaneous tibial nerve stimulation (PTNS) in females with faecal incontinence: the impact of sphincter morphology and rectal sensation on the clinical outcome. Int J Colorectal Dis. 2012;27:927–30.
Munoz-Duyos A, Navarro-Luna A, Brosa M, Pando JA, Sitges-Serra A, Marco-Molina C. Clinical and cost effectiveness of sacral nerve stimulation for faecal incontinence. Br J Surg. 2008;95:1037–43.
Leroi AM, Lenne X, Dervaux B, Chartier-Kastler E, Mauroy B, Normand LL, et al. Outcome and cost analysis of sacral nerve modulation for treating urinary and/or fecal incontinence. Ann Surg. 2011;253:720–32.
Hotouras A, Murphy J, Thin NN, Allison M, Horrocks E, Williams NS, Knowles CH, Chan CL. Outcome of sacral nerve stimulation (SNS) for fecal incontinence in patients refractory to percutaneous tibial nerve stimulation (PTNS). Dis Colon Rectum. 2013;56(7):915–20.
Hotouras A, Murphy J, Walsh U, Allison M, Curry A, Williams NS, Knowles CH, Chan CL. Outcome of percutaneous tibial nerve stimulation (PTNS) for fecal incontinence: a prospective cohort study. Ann Surg. 2014;259(5):939–43.
Acknowledgments
No funding has been received for this study.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hotouras, A., Murphy, J., Allison, M. et al. Prospective clinical audit of two neuromodulatory treatments for fecal incontinence: sacral nerve stimulation (SNS) and percutaneous tibial nerve stimulation (PTNS). Surg Today 44, 2124–2130 (2014). https://doi.org/10.1007/s00595-014-0898-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-014-0898-0