Abstract
Background
Post-transplantation lymphoproliferative disorder (PTLD) is a group of life-threatening complications of organ transplantation, which occurs most frequently in pediatric patients. This retrospective study evaluates a single-institution experience of five cases of PTLD after living-donor liver transplantation (LDLT).
Patients and method
We reviewed the records of 78 pediatric patients (<18 years old) and 54 adult patients, who underwent LDLT between July 1991 and December 2009.
Result
PTLD was diagnosed in five pediatric patients, yielding an overall incidence of 3.8%. There were no significant differences between the pediatric patients with and those without PTLD in terms of their age, sex, reason for transplantation, calcineurin inhibitor, Epstein–Barr virus (EBV) serostatus, ABO compatibility, lymphocyte cross-matching, or episodes of biopsy proven rejection. Two patients with abdominal lymphadenopathy and one with gastrointestinal PTLD responded to a reduction in immunosuppression. Treatment with rituximab was necessary for another gastrointestinal PTLD patient. Diffuse large-B-cell lymphoma was diagnosed in one patient with mediastinal and lung masses. This patient was treated with chemotherapy and rituximab, followed by surgical resection. All patients survived and no evidence of recurrence has been found since.
Conclusion
Although PTLD is potentially life-threatening, it can be managed by appropriate and prompt treatment, with a good outcome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Post-transplantation lymphoproliferative disorder (PTLD) is a life-threatening complication of solid organ transplantation. The development of lymphoma after transplantation was first described in 1968, by Doak et al. [1], in a renal transplant recipient, but the term “PTLD” was introduced in 1984, by Starzl et al. [2]. The severe impairment of T-cell function as a result of the immunosuppression required to prevent allograft rejection also places transplant patients at risk of the development of PTLD. Epstein–Barr virus (EBV) plays an essential role in the development of these lymphomas, and impaired T-cell function allows the uncontrolled proliferation of B lymphocytes that are infected and transformed by the virus [3]. However, PTLD is not exclusively associated with EBV infection, because EBV-negative PTLD is also being increasingly recognized, usually developing late after transplantation, [4, 5, 6]. This entity appears to be predominantly restricted to adult recipients [7]. The risk factors for PTLD include the degree of immunosuppression and the development of a primary infection after transplantation, so a higher incidence is seen in EBV-seronegative pediatric patients receiving a transplant from an EBV-seropositive donor [8]. The incidence of PTLD ranges from 1 to 20% among solid organ transplant recipients [9, 10]. Among liver transplant recipients, the prevalence of PTLD ranges from 2 to 4% in adults, but is reported to be as high as 20% in pediatric recipients [7, 11, 12]. However, these studies predominantly analyzed deceased-donor liver transplantation recipients. Interestingly, a recent Japanese study found that the incidence of PTLD after adult-to-adult living-donor liver transplantation was relatively low (0.9%) [13]. Another study reported no PLTD patients among 81 children who underwent living-donor liver transplantation (LDLT) [14].
Histologically, PTLD comprises a heterogeneous group of lymphoproliferative disorders, ranging from reactive, polyclonal hyperplasia to aggressive non-Hodgkin’s lymphoma [3]. PTLD characteristically involves extranodal sites, with frequent involvement of the allograft and the gastrointestinal tract [15, 16], but it may occur at virtually any site, including the skin [17] and central nervous system [18]. Although they are not equal to PTLD, primary extranodal non-Hodgkin’s lymphomas arising from the common bile duct have been reported [19].
A reduction in immunosuppression is considered as the first-line therapy for PTLD [20, 21]. Monoclonal antibody therapy (rituximab) is also frequently used and now widely regarded as the first-line therapy [22, 23]. Chemotherapy with the regimens used for lymphoma, such as cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP), is reserved for patients with more extensive high-grade disease or those in whom initial treatments have failed [3]. When PTLD is confined to one site, radiation and/or surgery can effectively control the local disease [5]. Surgery and radiation also play a role in the management of local complications in vital organ structures.
We report our institutional experience of PTLD in LDLT recipients, focusing on the diversity of PTLD manifestations and the different approaches to treatment.
Patients and methods
The records of 78 pediatric patients (<18 years old) and 54 adult patients who underwent LDLT between July 1991 and December 2009 were reviewed retrospectively. This study was approved by the Ethics Committee of Tohoku University Hospital. All patients had given their informed consent for all procedures and treatments. The primary immunosuppression regimen consisted of a calcineurin inhibitor (tacrolimus or cyclosporine) and steroids. In the early 1990s, we had no protocol for discontinuing steroid therapy, but in the late 1990s, steroid therapy was ceased 12 months after transplantation by design, and from 2000 onwards steroid therapy was discontinued around 6 months after transplantation. The majority of patients transplanted before 1998 and a few patients transplanted after 1999 received azathioprine, calcineurin inhibitor, and steroids. Mycophenolate mofetil was given to some patients. Forty-five adult patients and three pediatric patients transplanted after December 2002 received induction therapy with anti-interleukin 2 (IL2) receptor antibody. Rejection episodes were treated with methylprednisolone pulse therapy. Deoxyspergualin [24] or murine monoclonal anti-CD3 antibody (OKT3) was given when steroid treatment failed.
In patients with suspected EBV infection, we performed quantitative real-time PCR to detect EBV DNA in their peripheral-blood mononuclear cells and/or serum (cut-off value >102.5 copies/μg DNA) [25]. When an elevated EBV DNA load was detected, we performed a lymph-node biopsy. If there was no safely accessible lymph node, we made all decisions based on a comprehensive assessment of clinical symptoms, EBV DNA load, and images.
Statistical analysis
Comparative statistical analyses were performed using the Mann–Whitney U test. The χ2 and Fisher’s exact tests were used for categorical variables. p < 0.05 was considered significant.
Results
Incidence and presentation of PTLD
The overall incidence of PTLD in our institutional experience was 3.8% (5/132). All five patients in whom PTLD was diagnosed were children under 6 years old at the time of transplantation. Thus, the incidence of PTLD in the adult and pediatric patients was 0 and 6.4%, respectively. The overall median time to the development of PTLD was 14 months (4–31 months; Table 1).
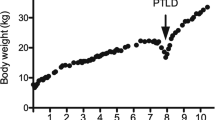
The initial symptom of PTLD in all five patients was fever. Two patients suffered gastrointestinal symptoms, including diarrhea, and one patient with large pulmonary and mediastinal masses suffered respiratory symptoms, including cough, wheezing, and tachypnea (Fig. 1a). The lymph nodes were involved in four patients. The patient characteristics are summarized in Table 1.
Computed tomography (CT) scans of patient 4, showing a large pulmonary and mediastinal masses in a patient with respiratory symptoms, including cough, wheezing, and tachypnea. A CT-guided needle biopsy was performed, confirming the diagnosis of diffuse, large-B-cell lymphoma. b CT after six cycles of rituximab and three cycles of cyclophosphamide and prednisolone chemotherapy showed reduction in the sizes of the pulmonary and mediastinal masses. c CT after another two cycles of rituximab, cyclophosphamide, adriamycin, vincristine, and prednisolone (R-CHOP) chemotherapy revealed residual mediastinal and pulmonary tumors. d After another two cycles of CHOP chemotherapy following surgical resection of the residual mediastinal tumor, CT revealed a residual a lung mass, in which FDG-PET CT showed no abnormal uptake
Patient characteristics
The pediatric PTLD patients were compared with pediatric non-PTLD patients in terms of their age, sex, primary disease, primary immunosuppression, EBV serostatus before transplantation, ABO compatibility, lymphocyte cross-matching, and rejection (Table 2). All five PTLD patients underwent liver transplantation for biliary atresia and four were seronegative for EBV before transplantation. Lymphocyte cross-matching was negative in all the PTLD patients. However, there were no significant differences between the pediatric patients with and those without PTLD in terms of age, sex, reason for transplantation, calcineurin inhibitor, EBV serostatus, ABO compatibility, lymphocyte cross-matching, or episodes of biopsy-proven rejection.
Immunosuppression before PTLD onset
All five patients received tacrolimus, and three were still receiving steroids at the onset of PTLD (Table 1). Patient 2 had suffered from biopsy proven repeated rejection. PTLD developed only 4 months after transplantation in patient 4 and immediately before the scheduled discontinuation of steroid therapy in patient 5. Hence, these patients were still receiving steroids. Although patients 1 and 3 were not receiving steroids at the onset of PTLD, we could not discontinue their steroid therapy within 12 months because they were still suffering episodes suggesting rejection.
The primary immunosuppressive agents given to four patients were tacrolimus and steroids. Only patient 1 received tacrolimus, steroids, and azathioprine as the primary immunosuppression. Patient 2 was started on azathioprine 1 year after transplantation, but it was discontinued after drug-induced liver dysfunction before the onset of PTLD. Tacrolimus was changed to cyclosporine only for patient 2, followed by reconversion to tacrolimus before the onset of PTLD. None of the PTLD patients received OKT3, but one (patient 2) received deoxyspergualin for steroid-resistant rejection. No PTLD patient received induction therapy with anti-IL2 receptor antibody.
Histopathological presentation
The disease of three of the five PTLD patients was not easily accessible for biopsy, but they had persistently high EBV loads and abdominal lymphadenopathy. One of the patients with gastrointestinal symptoms had no lymphadenopathy, but the diagnosis of gastrointestinal PTLD was based on a persistently high EBV load and gastrointestinal edema. A computed tomography (CT)-guided needle biopsy was performed only in one patient with large pulmonary and mediastinal masses. Histology showed EBV-related, CD20-positive, diffuse large-B-cell lymphoma, the recipient origin of which was confirmed by fluorescence in situ hybridization (FISH; Fig. 2).
Histology of a biopsy from patient 4 showed an EBV-related, CD20-positive, diffuse, large-B-cell lymphoma, which was of recipient origin, as confirmed by FISH. a Histology showed large-cell lymphoid proliferation [hematoxylin–eosin (HE) staining; ×400) b In situ hybridization of EBV-encoded small RNA (EBER) was performed. EBER was positive in several lymphoid cells (×400). c Immunostaining for CD20 revealed that these lymphoma cells were CD20 positive (×400). d Lymphoid cell showing an X–Y pattern on fluorescence in situ hybridization (FISH), indicating that post-transplantation lymphoproliferative disorder (PTLD) was of recipient origin because the donor was his mother. The red signal indicates chromosome Xp11.1–q11.1 and the green signal indicates chromosome Yq12
Treatments and outcomes
Our initial three patients (patients 1–3) responded well to reduced immunosuppression and have shown no evidence of recurrence to this point. In patient 1, tacrolimus was discontinued altogether and steroid therapy was resumed; then, after the PTLD improved, cyclosporine was started. In patient 2, cellular rejection occurred after tacrolimus and steroid therapies were discontinued altogether, so low-dose tacrolimus was restarted, maintaining a trough at around 4.0 ng/mL, followed by steroids again. A study undertaken at our institution subsequently demonstrated that EBV infection can be kept asymptomatic with a tacrolimus trough level below 3.0 ng/mL [ 21 ]. Therefore, in patient 3, the tacrolimus dose was reduced, maintaining the trough below 3.0 ng/mL. A reduction in the dose of tacrolimus to maintain the trough below 3.0 ng/mL, together with the withdrawal of steroids, is now the initial therapeutic approach for patients with an increased EBV load or PTLD, at our institution, as was done for patients 4 and 5. When the trough is high, tacrolimus should be discontinued until it drops to about 3.0 ng/mL. However, reduced immunosuppression was insufficient to stabilize the PTLD in our two most recent patients (patients 4 and 5).
One patient (patient 4) with gastrointestinal symptoms, high fever, and abdominal lymphadenopathy, did not respond to a reduction in immunosuppression. Thus, he was commenced on rituximab at a dose of 375 mg/m2 once a week, following which, his gastrointestinal symptoms and high fever improved quickly and his blood EBV load decreased to normal control levels. Although cellular rejection developed after the treatment, he was still in complete remission at his 15-month follow-up.
The patient with large mediastinal and pulmonary masses was intubated and on a mechanical ventilator when he was transferred to our institution. Six cycles of rituximab and three cycles of cyclophosphamide and prednisolone chemotherapy every 3 weeks reduced the size of the tumors (Fig. 1b), and he was successfully extubated. His blood EBV load decreased quickly, but for the remaining mediastinal and pulmonary tumors, he received another two cycles of rituximab, cyclophosphamide, adriamycin, vincristine, and prednisolone (R-CHOP) chemotherapy. A CT scan after these treatments revealed residual mediastinal and pulmonary tumors (Fig. 1c). Fluoro-2-deoxy-d-glucose-positron emission tomography (FDG-PET) CT revealed abnormal uptake only in the mediastinal tumor (Fig. 3). We recognized viable tumor cells only in the mediastinal tumor, which was then removed surgically. Histological examination of the removed tumor revealed residual viable tumor cells (Fig. 4). After another two cycles of CHOP chemotherapy, the patient was in complete remission when last seen at the 12-month follow-up (Fig. 1d). None of the patients had immunosuppression completely withdrawn at their last follow-up.
Discussion
The overall incidence of PTLD in this series at our institution was 3.8% overall, and 6.4% of the pediatric patients. PTLD did not develop in any of the adult patients. These incidences are similar to those reported in other studies that predominantly analyzed deceased-donor liver transplantation recipients [7, 11, [12]. The incidence in this series was slightly higher than that in other recent Japanese studies, in which LDLT patients were predominantly analyzed [13, 14]. This is probably because our series included early cases, treated in the 1990s. Two of our PTLD patients received liver grafts in the mid 1990s and one received their graft in 2001. The other two patients, who received liver grafts after 2005, were only 6 months old when they underwent liver transplantation, which suggests that younger age at transplantation is a risk factor for PTLD among pediatric patients, although we could not show that the age at transplantation was associated with the incidence of PTLD in this study. One Japanese report suggested younger age at transplantation as a risk factor for post-transplantation EBV infection among pediatric recipients [14].
An important risk factor for the development of PTLD is the intensity and amount of immunosuppression administered to the patient [26]. Although we found no significant difference, two patients suffered from biopsy-proven cellular rejection and one suffered from repeated episodes suggesting rejection. Consequently, their steroid therapy could not be discontinued within 12 months. Induction and rejection treatments with anti-T-cell antibody, especially OKT3, and anti-thymocyte globulin increase the risk of PTLD [9, 27, 28, 29]. Although three pediatric patients received OKT3 for allograft rejection in our series, PTLD did not develop in any of them. Interestingly, induction therapy with anti-IL2 receptor antibody does not seem to be associated with an increased risk of PTLD [9, 30, 31]. At our institution, 48 adult and 3 pediatric recipients who underwent transplantation after December 2002 received induction therapy with anti-IL2 receptor antibody, and none of them suffered PTLD, which supports the safety of induction therapy with this antibody. Although some studies have compared the effects of tacrolimus with those of cyclosporine A as risk factors for PTLD [9, 27, 32, 33], there were no differences between the pediatric patients with and those without PTLD in terms of the calcineurin inhibitor in our series.
In general, PTLD is characterized by the transformation of lymphocytes by EBV; therefore, patients who are EBV-seronegative patients receiving allografts from EBV-seropositive donors, resulting in primary EBV infection, are at 10 to 50-fold risk of PTLD development [26, 34, 35, 36],. This also accounts for the high incidence of PTLD in the early post-transplantation period in pediatric patients, who are more often still EBV seronegative at the time of transplantation. In the present study, four of five cases of PTLD occurred during the first 2 years after transplantation. Furthermore, two patients who received liver grafts at 6 months of age suffered PTLD in the first year after transplantation. Four PTLD patients were EBV seronegative and received liver grafts from EBV-seropositive donors, although one gastrointestinal PTLD patient was EBV-seropositive before transplantation. The measurement of peripheral-blood EBV levels is helpful for the diagnosis and monitoring of PTLD, and some studies have also shown promising results of measuring peripheral-blood PCR [37, 38, 39, 40, 41]. In our series, all five patients had high EBV loads when PTLD was diagnosed and their EBV loads decreased to undetectable or normal control levels after treatment.
Because PTLD often presents in a nonspecific way if it is not suspected clinically, it is a major challenge to diagnose at an early stage. PTLD often presents at extranodal sites, including in the allograft and gastrointestinal tract [15, 16]. Because the gastrointestinal tract is frequently involved, gastrointestinal signs and symptoms, such as diarrhea and bleeding, may lead to a diagnosis of gastrointestinal PTLD. In the present study, two patients suffered gastrointestinal PTLD with severe diarrhea, high fever, and high blood EBV loads. In patients with respiratory symptoms, CT of the thoracic cavity may be helpful. Pulmonary masses in patients with high blood EBV loads indicate lung involvement in PTLD, as in our patient with pulmonary and mediastinal masses. FDG-PET scanning is becoming an important tool in the visualization of malignant lymphomas, especially for detection in extranodal locations and in post-treatment evaluations [42, 43]. Some studies have found FDG-PET scanning to be superior to conventional imaging for the staging of PTLD and evaluation of treatments [44, 45, 46]. In our patient treated with R-CHOP therapy, FDG-PET clearly differentiated between the residual masses of the vital tumor and scar tissue. As FDG-PET is also thought to be useful for the early detection of recurrent PTLD, it was performed as part of the post-treatment surveillance of this patient.
Two different sources of the lymphocytes involved in PTLD have been suggested: the recipient and the donor. Lymphocytes of donor origin are those EBV-positive cells that have escaped the immune system of the recipient. Lymphoid cells of donor origin transplanted within the allograft may undergo proliferation in the tolerant environment produced by immunosuppression. PTLD of donor origin is reportedly localized to the transplanted organ, whereas PTLD of recipient origin has an extra-allograft location [47]. It has been suggested that PTLD is usually of recipient origin in solid organ transplantation recipients [3]. Because it is difficult to biopsy abdominal lymphadenopathies and perform digestive endoscopies in young children, we could only perform pathological examination in one patient. This patient was male and received an allograft from his mother. Histology showed an EBV-related, CD20-positive, diffuse, large-B-cell lymphoma and FISH analysis showed an XY pattern; thus confirming that his PTLD of recipient origin.
Because of its inherent association with immunosuppression, a key feature of PTLD treatment includes the restoration of a functional immune system in the recipient. Therefore, initial therapy is aimed at reducing immunosuppression in most of the patients. The response rates vary with some patients achieving complete remission with a reduction in immunosuppression alone or in combination with localized therapy, such as radiation or surgery, whereas others experience progressive disease [20, 48]. Factors that predict failure of reduced immunosuppression as a single treatment modality include elevated lactate dehydrogenase levels, organ dysfunction, and multi-organ involvement [20]. A previous study undertaken at our institution demonstrated that a reduction in the blood level of tacrolimus was associated with a reduction in the EBV load after liver transplantation, and that EBV infection could be kept asymptomatic when the tacrolimus trough level was under 3.0 ng/mL [21]. Rituximab is a chimeric anti-CD20 antibody that has recently been used to treat lymphoma. Rituximab also displays activity against PTLD after solid organ transplantation, and response rates of 44–100% have been reported in several studies [49, 50, 51, 52]. A recent phase 2 clinical trial of rituximab for the treatment of PTLD revealed a response rate of 44% on day 80. This trial included patients whose only previous therapy was the reduction of immunosuppression, but excluded patients with central nervous system PTLD [23]. Chemotherapy with regimens used in lymphoma therapies, such as CHOP, remains a therapeutic option for patients who do not respond to immune manipulation or rituximab. PTLD generally remains chemotherapy-sensitive after progression or failure to respond to rituximab, when used as the first-line therapy, and CHOP salvage therapy can achieve an overall response rate of up to 70% in these patients [53]. To reduce the toxicity of chemotherapy, lower-dose chemotherapy with cyclophosphamide and prednisone was evaluated in 36 pediatric patients who had failed to respond to the first-line therapy, with an excellent overall response rate of 83% [54]. When PTLD is confined to one site, radiation and/or surgery can effectively control the local disease [5]. Surgery and radiation also play roles in managing the local complications of PTLD. Our current treatment algorithm is outlined in Fig. 5. In our series, the reduction of immunosuppression alone sufficiently controlled PTLD in three patients. This might mean that the patients received over immunosuppression at the onset of the disease. Indeed, two of these three patients had suffered from repeated biopsy-proven rejection, and another patient was still undergoing steroid therapy at the onset of PTLD because of repeated episodes suggesting rejection. The method of reducing immunosuppression improved with time. We had no criteria upon which to base the appropriate immunosuppression doses for our initial two patients. Now, reducing the dose of tacrolimus to a level that maintains the trough below 3.0 ng/mL and withdrawing steroids is our treatment approach for PTLD, although rituximab was necessary for one patient with gastrointestinal PTLD. Because there was no safely accessible lymph node for biopsy in this patient, it was possible that his PTLD was a T-cell lymphoma; however, his symptoms improved and his EBV DNA load decreased rapidly after the initiation of rituximab. This outcome suggests that his PTLD was a B-cell lymphoma. Because rituximab is not very dangerous, its use has been suggested when there is no safely accessible site for a pathological diagnosis, especially in pediatric patients. We used chemotherapy with rituximab followed by surgical resection to treat our patient with aggressive lung and mediastinal masses. Complete remission was achieved in all five patients, with no recurrence to this point.
Our therapeutic strategy for post-transplantation lymphoproliferative disorder (PTLD). In patients with early or suspected disease, the initial therapy is reduction of immunosuppression. In patients who fail to respond or whose PTLD progresses, the addition of rituximab may sufficiently control the disease. For extensive high-grade disease or further progression after the initial therapy, chemotherapy, such as R-CHOP (cyclophosphamide, adriamycin, vincristine, prednisolone, and rituximab) therapy, is commenced. Surgery is performed when the disease is localized
In summary, we treated five pediatric cases of PTLD after LDLT. Each case manifested differently and required different therapeutic approaches, including cytotoxic chemotherapy. Although PTLD is a life-threatening complication after liver transplantation, prompt and appropriate treatment with rituximab and chemotherapy, as deemed appropriate, can contribute to a good outcome.
References
Doak PB, Montgomerie JZ, North JD, Smith F. Reticulum cell sarcoma after renal homotransplantation and azathioprine and prednisone therapy. Br Med J. 1968;4:746–8.
Starzl TE, Nalesnik MA, Porter KA, Ho M, Iwatsuki S, Griffith BP, et al. Reversibility of lymphomas and lymphoproliferative lesions developing under cyclosporin-steroid therapy. Lancet. 1984;1:583–7.
Heslop HE. How I treat EBV lymphoproliferation. Blood. 2009;114:4002–8.
Leblond V, Davi F, Charlotte F, Dorent R, Bitker MO, Sutton L, et al. Posttransplant lymphoproliferative disorders not associated with Epstein–Barr virus: a distinct entity? J Clin Oncol. 1998;16:2052–9.
Dotti G, Fiocchi R, Motta T, Mammana C, Gotti E, Riva S, et al. Lymphomas occurring late after solid-organ transplantation: influence of treatment on the clinical outcome. Transplantation. 2002;74:1095–102.
Ghobrial IM, Habermann TM, Macon WR, Ristow KM, Larson TS, Walker RC, et al. Differences between early and late posttransplant lymphoproliferative disorders in solid organ transplant patients: are they two different diseases? Transplantation. 2005;79:244–7.
Jain A, Nalesnik M, Reyes J, Pokharna R, Mazariegos G, Green M, et al. Posttransplant lymphoproliferative disorders in liver transplantation: a 20-year experience. Ann Surg. 2002;236:429–36. (discussion 36–7).
Smith JM, Corey L, Healey PJ, Davis CL, McDonald RA. Adolescents are more likely to develop posttransplant lymphoproliferative disorder after primary Epstein–Barr virus infection than younger renal transplant recipients. Transplantation. 2007;83:1423–8.
Opelz G, Dohler B. Lymphomas after solid organ transplantation: a collaborative transplant study report. Am J Transplant. 2004;4:222–30.
Muti G, Cantoni S, Oreste P, Klersy C, Gini G, Rossi V, et al. Post-transplant lymphoproliferative disorders: improved outcome after clinico-pathologically tailored treatment. Haematologica. 2002;87:67–77.
Smets F, Vajro P, Cornu G, Reding R, Otte JB, Sokal E. Indications and results of chemotherapy in children with posttransplant lymphoproliferative disease after liver transplantation. Transplantation. 2000;69:982–4.
Guthery SL, Heubi JE, Bucuvalas JC, Gross TG, Ryckman FC, Alonso MH, et al. Determination of risk factors for Epstein–Barr virus-associated posttransplant lymphoproliferative disorder in pediatric liver transplant recipients using objective case ascertainment. Transplantation. 2003;75:987–93.
Kataoka K, Seo S, Sugawara Y, Ota S, Imai Y, Takahashi T, et al. Post-transplant lymphoproliferative disorder after adult-to-adult living donor liver transplant: case series and review of literature. Leuk Lymphoma. 2010;51:1494–501.
Shigeta T, Imadome K, Sakamoto S, Fukuda A, Kakiuchi T, Matsuno N, et al. Epstein–Barr virus infection after pediatric living-related liver transplantation—management and risk factors. Transplant Proc. 2010;42:4178–80.
Bakker NA, van Imhoff GW, Verschuuren EA, van Son WJ, Homan van der Heide JJ, Veeger NJ, et al. Early onset post-transplant lymphoproliferative disease is associated with allograft localization. Clin Transplant. 2005;19:327–34.
Ghobrial IM, Habermann TM, Maurer MJ, Geyer SM, Ristow KM, Larson TS, et al. Prognostic analysis for survival in adult solid organ transplant recipients with post-transplantation lymphoproliferative disorders. J Clin Oncol. 2005;23:7574–82.
Beynet DP, Wee SA, Horwitz SS, Kohler S, Horning S, Hoppe R, et al. Clinical and pathological features of posttransplantation lymphoproliferative disorders presenting with skin involvement in 4 patients. Arch Dermatol. 2004;140:1140–6.
Phan TG, O’Neill BP, Kurtin PJ. Posttransplant primary CNS lymphoma. Neuro Oncol. 2000;2:229–38.
Dote H, Ohta K, Nishimura R, Teramoto N, Asagi A, Nadano S, et al. Primary extranodal non-Hodgkin’s lymphoma of the common bile duct manifesting as obstructive jaundice: report of a case. Surg Today. 2009;39:448–51.
Tsai DE, Hardy CL, Tomaszewski JE, Kotloff RM, Oltoff KM, Somer BG, et al. Reduction in immunosuppression as initial therapy for posttransplant lymphoproliferative disorder: analysis of prognostic variables and long-term follow-up of 42 adult patients. Transplantation. 2001;71:1076–88.
Orii T, Ohkohchi N, Satomi S, Hoshino Y, Kimura H. Decreasing the Epstein–Barr virus load by adjusting the FK506 blood level. Transpl Int. 2002;15:529–34.
Svoboda J, Kotloff R, Tsai DE. Management of patients with post-transplant lymphoproliferative disorder: the role of rituximab. Transpl Int. 2006;19:259–69.
Choquet S, Leblond V, Herbrecht R, Socie G, Stoppa AM, Vandenberghe P, et al. Efficacy and safety of rituximab in B-cell post-transplantation lymphoproliferative disorders: results of a prospective multicenter phase 2 study. Blood. 2006;107:3053–7.
Nakanishi C, Kawagishi N, Sekiguchi S, Akamatsu Y, Sato K, Miyagi S, et al. Steroid-resistant late acute rejection after a living donor liver transplantation: case report and review of the literature. Tohoku J Exp Med. 2007;211:195–200.
Orii T, Ohkohchi N, Kikuchi H, Koyamada N, Chubachi S, Satomi S, et al. Usefulness of quantitative real-time polymerase chain reaction in following up patients with Epstein–Barr virus infection after liver transplantation. Clin Transplant. 2000;14:308–17.
Bakker NA, van Imhoff GW, Verschuuren EA, van Son WJ. Presentation and early detection of post-transplant lymphoproliferative disorder after solid organ transplantation. Transpl Int. 2007;20:207–18.
Caillard S, Dharnidharka V, Agodoa L, Bohen E, Abbott K. Posttransplant lymphoproliferative disorders after renal transplantation in the United States in era of modern immunosuppression. Transplantation. 2005;80:1233–43.
Swinnen LJ, Costanzo-Nordin MR, Fisher SG, O’Sullivan EJ, Johnson MR, Heroux AL, et al. Increased incidence of lymphoproliferative disorder after immunosuppression with the monoclonal antibody OKT3 in cardiac-transplant recipients. N Engl J Med. 1990;323:1723–8.
Duvoux C, Pageaux GP, Vanlemmens C, Roudot-Thoraval F, Vincens-Rolland AL, Hezode C, et al. Risk factors for lymphoproliferative disorders after liver transplantation in adults: an analysis of 480 patients. Transplantation. 2002;74:1103–9.
Cherikh WS, Kauffman HM, McBride MA, Maghirang J, Swinnen LJ, Hanto DW. Association of the type of induction immunosuppression with posttransplant lymphoproliferative disorder, graft survival, and patient survival after primary kidney transplantation. Transplantation. 2003;76:1289–93.
Marino IR, Doria C, Scott VL, Foglieni CS, Lauro A, Piazza T, et al. Efficacy and safety of basiliximab with a tacrolimus-based regimen in liver transplant recipients. Transplantation. 2004;78:886–91.
Pirsch JD. Cytomegalovirus infection and posttransplant lymphoproliferative disease in renal transplant recipients: results of the U.S. multicenter FK506 Kidney Transplant Study Group. Transplantation. 1999;68:1203–5.
Wiesner RH. A long-term comparison of tacrolimus (FK506) versus cyclosporine in liver transplantation: a report of the United States FK506 Study Group. Transplantation. 1998;66:493–9.
Armitage JM, Kormos RL, Stuart RS, Fricker FJ, Griffith BP, Nalesnik M, et al. Posttransplant lymphoproliferative disease in thoracic organ transplant patients: ten years of cyclosporine-based immunosuppression. J Heart Lung Transplant. 1991;10:877–86. (discussion 86–7).
Walker RC, Marshall WF, Strickler JG, Wiesner RH, Velosa JA, Habermann TM, et al. Pretransplantation assessment of the risk of lymphoproliferative disorder. Clin Infect Dis. 1995;20:1346–53.
Shahinian VB, Muirhead N, Jevnikar AM, Leckie SH, Khakhar AK, Luke PP, et al. Epstein–Barr virus seronegativity is a risk factor for late-onset posttransplant lymphoroliferative disorder in adult renal allograft recipients. Transplantation. 2003;75:851–6.
Rooney CM, Loftin SK, Holladay MS, Brenner MK, Krance RA, Heslop HE. Early identification of Epstein–Barr virus-associated post-transplantation lymphoproliferative disease. Br J Haematol. 1995;89:98–103.
McDiarmid SV, Jordan S, Kim GS, Toyoda M, Goss JA, Vargas JH, et al. Prevention and preemptive therapy of postransplant lymphoproliferative disease in pediatric liver recipients. Transplantation. 1998;66:1604–11.
Tsai DE, Nearey M, Hardy CL, Tomaszewski JE, Kotloff RM, Grossman RA, et al. Use of EBV PCR for the diagnosis and monitoring of post-transplant lymphoproliferative disorder in adult solid organ transplant patients. Am J Transplant. 2002;2:946–54.
Lee TC, Savoldo B, Barshes NR, Rooney CM, Heslop HE, Gee AP, et al. Use of cytokine polymorphisms and Epstein–Barr virus viral load to predict development of post-transplant lymphoproliferative disorder in paediatric liver transplant recipients. Clin Transplant. 2006;20:389–93.
Tsai DE, Douglas L, Andreadis C, Vogl DT, Arnoldi S, Kotloff R, et al. EBV PCR in the diagnosis and monitoring of posttransplant lymphoproliferative disorder: results of a two-arm prospective trial. Am J Transplant. 2008;8:1016–24.
Moog F, Bangerter M, Diederichs CG, Guhlmann A, Merkle E, Frickhofen N, et al. Extranodal malignant lymphoma: detection with FDG PET versus CT. Radiology. 1998;206:475–81.
Zijlstra JM, Lindauer-van der Werf G, Hoekstra OS, Hooft L, Riphagen II, Huijgens PC. 18F-fluoro-deoxyglucose positron emission tomography for post-treatment evaluation of malignant lymphoma: a systematic review. Haematologica 2006;91:522–9.
Marom EM, McAdams HP, Butnor KJ, Coleman RE. Positron emission tomography with fluoro-2-deoxy-d-glucose (FDG-PET) in the staging of post transplant lymphoproliferative disorder in lung transplant recipients. J Thorac Imaging. 2004;19:74–8.
O’Conner AR, Franc BL. FDG PET imaging in the evaluation of post-transplant lymphoproliferative disorder following renal transplantation. Nucl Med Commun. 2005;26:1107–11.
Bakker NA, Pruim J, de Graaf W, van Son WJ, van der Jagt EJ, van Imhoff GW. PTLD visualization by FDG-PET: improved detection of extranodal localizations. Am J Transplant. 2006;6:1984–5.
Aucejo F, Rofaiel G, Miller C. Who is at risk for post-transplant lymphoproliferative disorders (PTLD) after liver transplantation? J Hepatol. 2006;44:19–23.
Paya CV, Fung JJ, Nalesnik MA, Kieff E, Green M, Gores G, et al. Epstein–Barr virus-induced posttransplant lymphoproliferative disorders. ASTS/ASTP EBV-PTLD Task Force and The Mayo Clinic Organized International Consensus Development Meeting. Transplantation. 1999;68:1517–25.
Savoldo B, Rooney CM, Quiros-Tejeira RE, Caldwell Y, Wagner HJ, Lee T, et al. Cellular immunity to Epstein–Barr virus in liver transplant recipients treated with rituximab for post-transplant lymphoproliferative disease. Am J Transplant. 2005;5:566–72.
Ganne V, Siddiqi N, Kamaplath B, Chang CC, Cohen EP, Bresnahan BA, et al. Humanized anti-CD20 monoclonal antibody (Rituximab) treatment for post-transplant lymphoproliferative disorder. Clin Transplant. 2003;17:417–22.
Blaes AH, Peterson BA, Bartlett N, Dunn DL, Morrison VA. Rituximab therapy is effective for posttransplant lymphoproliferative disorders after solid organ transplantation: results of a phase II trial. Cancer. 2005;104:1661–7.
Oertel SH, Verschuuren E, Reinke P, Zeidler K, Papp-Vary M, Babel N, et al. Effect of anti-CD 20 antibody rituximab in patients with post-transplant lymphoproliferative disorder (PTLD). Am J Transplant. 2005;5:2901–6.
Trappe R, Riess H, Babel N, Hummel M, Lehmkuhl H, Jonas S, et al. Salvage chemotherapy for refractory and relapsed posttransplant lymphoproliferative disorders (PTLD) after treatment with single-agent rituximab. Transplantation. 2007;83:912–8.
Gross TG, Bucuvalas JC, Park JR, Greiner TC, Hinrich SH, Kaufman SS, et al. Low-dose chemotherapy for Epstein–Barr virus-positive post-transplantation lymphoproliferative disease in children after solid organ transplantation. J Clin Oncol. 2005;23:6481–8.
Conflict of interest
None of the authors have any conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nakanishi, C., Kawagishi, N., Sekiguchi, S. et al. Post-transplantation lymphoproliferative disorder in living-donor liver transplantation: a single-center experience. Surg Today 42, 741–751 (2012). https://doi.org/10.1007/s00595-012-0127-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-012-0127-7