Abstract
Direct oral anticoagulants (DOACs) include dabigatran, which inhibits thrombin, and apixaban, edoxaban, and rivaroxaban, which inhibit factor Xa. They have been extensively studied in large trials involving patients affected by the most common cardiovascular diseases. As the presence of diabetes leads to peculiar changes in primary and secondary hemostasis, in this review we highlight the current evidence regarding DOAC use in diabetic patients included in the majority of recently conducted studies. Overall, in trials involving patients with atrial fibrillation, data seem to confirm at least a similar efficacy and safety of DOACs compared to warfarin in patients with or without diabetes. Furthermore, in diabetic patients, treatment with DOACs is associated with a significant relative reduction in vascular death compared to warfarin. In trials enrolling patients undergoing percutaneous coronary intervention, results concerning bleeding events are consistent in patients with or without diabetes. With regards to the COMPASS study, in patients with diabetes (n = 10,241), addition of rivaroxaban 2.5 mg to aspirin resulted in a significantly lower incidence of major adverse cardiovascular events (HR 0.74, 95% CI 0.61–0.90; interaction p = 0.68) with higher rates of major bleeding expected (HR 1.70, 95% CI 1.25–2.31). The 3287 patients with peripheral artery disease and diabetes receiving rivaroxaban plus aspirin had a twofold higher absolute reduction in the composite endpoint (cardiovascular death, myocardial infarction, and stroke) than patients without diabetes. Finally, we report the involvement of cytochromes or P-glycoprotein on the metabolism of the most commonly prescribed glucose-lowering drugs. No clinically relevant interactions are expected during the concomitant use of DOACs and anti-diabetic agents.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite the advances in technology achieved in the past decades and the improvement in diabetes care and complications following both the development of multidisciplinary approaches and a broad attention to advantages of lifestyle changes [1, 2], to date, diabetes mellitus (DM) still represents a major public concern [3, 4]. The prevalence of this worldwide epidemic disease is even expected to increase, according to the most recent estimates. Indeed, by 2060, the number of US adults with diagnosed diabetes is projected to nearly triple, increasing from 22.3 million in 2014 to 60.6 million in 2060 [5, 6].
As DM is a recognized major risk factor for cardiovascular (CV) disease, such as stable coronary artery disease (CAD), acute coronary syndrome (ACS), cerebral ischemic events, peripheral arterial disease (PAD), and atrial fibrillation (AF), an aggressive management is crucial [7, 8]. Indeed, patients with DM present peculiar changes in primary (platelet aggregation and vascular function) and secondary (coagulation and fibrinolysis) hemostasis. The resultant hypercoagulable and prothrombotic status is primarily due to a platelet dysfunction generated by the interaction of multiple factors such as hyperglycemia, insulin deficiency or resistance, associated metabolic pathologies (dyslipidemia, inflammation, and obesity), and cellular abnormalities (e.g., accelerated platelet turnover, increased generation of thrombin, decreased production of nitric oxide, up-regulation of P2Y12 receptor) [9, 10].
In this context, contemporary antithrombotic therapies could be effective for both primary and secondary prevention of atherothrombotic and thromboembolic events, moderating the impact of thrombosis on the global diabetes burden [11].
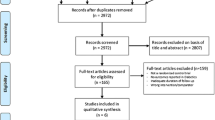
In the last few years, direct oral anticoagulants (DOACs) have been extensively studied in large phase III and phase IV international trials. These involved a great number of patients requiring anticoagulant treatment for common CV diseases like AF, CAD, PAD, venous thromboembolism (VTE), or ACS needing percutaneous coronary intervention (PCI) [12]. The majority of these trials have included a non-negligible proportion of patients with DM. Thus, the aim of this review is to provide an overview on the current evidence regarding DOAC treatment in patients with DM. Furthermore, as DOACs have the potential for pharmacokinetic (PK) interaction with a number of anti-diabetic agents, we examine the potential drug–drug interactions (DDIs) among DOACs and these drugs.
Prevention of stroke and systemic embolism in atrial fibrillation
DM seems associated with a higher risk of development and progression of AF [13]. The impact of diabetes on AF occurrence is actually debated due to conflicting results from different studies [14,15,16]. The results of a meta-analysis showed that DM was associated with a 40% increase in the risk of AF [relative risk (RR) 1.39, p < 0.001 compared with non-DM], which remained borderline significant even after correction for publication bias [RR 1.34, 95% confidence interval (CI) 1.07–1.68, p = 0.003] and multiple risk factors (RR 1.24, 95% CI 1.06–1.44, and 1.70, 1.29–2.22, p = 0.053, most-adjusted versus least-adjusted studies, respectively). Furthermore, the analysis of the impact of cumulative exposure to DM showed that the risk of prevalent AF was approximately 64% in individuals with DM for more than 10 years, compared with non-diabetic patients. In contrast, the risk was only 7% in those with DM for less than 5 years. However, the specific pathophysiological mechanism linking DM with increased risk for developing AF is not completely explained [17]. In 10,082 diabetic patients from the Action to Control Cardiovascular Risk in Diabetes (ACCORD) cohort randomized to an intensive or a standard therapeutic glycemic strategy, the intensive glycemic control did not affect the rate of new onset AF. However, patients with DM and incident AF had an increased risk of morbidity and mortality compared to those without AF [hazard ratio (HR) 2.65 for all-cause mortality; HR of 2.1 for myocardial infarction (MI); HR of 3.80 for heart failure] [18].
In patients with coexisting DM, the risk of cardioembolic stroke resulted increased with an incidence ranging between 3.6 and 8.6% per year in different studies [19]. In the ATRIA (Anticoagulation and Risk Factors in Atrial Fibrillation) study, duration of diabetes ≥ 3 years was a greater predictor of ischemic stroke (adjusted HR 1.74, 95% CI 1.10–2.76) than poor glycemic control (HbA1c > 9.0%: adjusted HR 1.04, 95% CI 0.57–1.92) in AF patients [20]. An analysis from the PREFER in AF (Prevention of thromboembolic events—European Registry in Atrial Fibrillation) indicated that DM patients treated with insulin had a significantly increased risk of stroke/systemic embolism (SSE) at 1 year versus either no diabetes (5.2% versus 1.9% HR 2.89; 95% CI 1.67–5.02; p = 0.0002) or diabetes without insulin treatment (5.2% vs 1.8%; HR 2.96; 95% CI 1.49–5.87; p = 0.0019). Conversely, SSE rates were similar in patients with diabetes not receiving insulin versus patients without diabetes (HR 0.97; 95% CI 0.58–1.61; p = 0.90). Moreover, the selective predictive role of insulin-requiring diabetes was independent of potential confounders, including diabetes duration [21].
DM has been included as one of the items of the CHADS2 score and of the CHA2DS2–VASc stroke risk factor scoring systems in patients with non-valvular AF [22, 23]. The latest European Society of Cardiology [24, 25] and North American [26] guidelines on AF either recommend anticoagulating people with a CHA2DS2–VASc score of ≥ 2 with a consensus for a Class I recommendation. Conversely, guidelines differ on recommendations regarding patients with a CHA2DS2–VASc score of 1. Indeed, the European guidelines approve anticoagulation in all people with non-valvular AF and diabetes (Class IIa, Level of recommendation B) with a preference for DOACs over vitamin K antagonists (VKA) (Class I, Level of recommendation A). Conversely, the American College of Cardiology/American Heart Association/Heart Rhythm Society guidelines state that even antithrombotic therapy with aspirin may be taken into consideration (Class IIb, Level of recommendation C) in patients belonging to this risk class.
However, it has been demonstrated that not all risk factors in the CHA2DS2–VASc score carry the same weight in estimating stroke risk. In a retrospective cohort study involving 186 570 AF patients, in male patients with a CHA2DS2–VASc score of 1, the highest risk for stroke was seen in those 65–74 years of age (HR 3.085; 95% CI 2.790–3.410) or those with DM (HR 2.655; 95% CI 2.230–3161). Similar results were reported in women with a CHA2DS2–VAScscore of 2 [27]. These findings were consistent with those reported by Olesen et al. [28] in the Danish nationwide study. Therefore, it seems reasonable to consider anticoagulation when diabetes is present, even if it is the only risk factor among the CHA2DS2–VASc factors [29].
Participants with diabetes represented a considerable proportion in the phase III randomized controlled trials with DOACs, ranging from 4221 (23%) in the RE-LY and 4547 (25%) in the ARISTOTLE studies to 5695 (40%) in the ROCKET AF and 7624 (36%) in the ENGAGE AF-TIMI [30,31,32,33]. Pre-specified post hoc analyses, examining the characteristics, efficacy, and safety profiles of these subgroups, showed that diabetic patients had more comorbidities and higher risk of SSE than participants without diabetes [34,35,36]. This risk was decreased using DOACs, with no significant interaction to diabetic status or the specific drug used. A lower embolic rate was observed in DM patients both in the ENGAGE and in the ROCKET studies (Table 1). Notably, DM patients were not equally represented in the subgroups of patients with previous stroke in either of the above-mentioned trials [34, 37]. Conversely, in the ARISTOTLE and in the RE-LY trials, the proportion of DM subjects was similar between patients with and without a previous cerebral event [36, 38]. As previous stroke is a recognized major risk factor for subsequent stroke, accounting for 2 points in the CHAD–VASc score, we may speculate that the lower proportion of DM patients among patients with a previous stroke enrolled in the ENGAGE and in the ROCKET could explicate the lower embolic rate observed in those studies.
Overall, compared with warfarin, DOACs reduced the incidence of major bleeding (MB), although there were some differences among those trials with regard to drug safety [39] (Table 1). Specifically, the 5647 patients with DM (≈ 40%) in ROCKET AF were younger, were more obese, and had more persistent AF, but fewer had previous stroke. The relative efficacy of rivaroxaban and warfarin for the prevention of SSE was similar in patients with (1.74 vs 2.14/100 patient-years, HR 0.82) and without (2.12 vs 2.32/100 patient-years, HR 0.92) DM (interaction p = 0.53). Conversely, the efficacy of rivaroxaban versus warfarin (2.83 vs 3.65/100 patient-years, HR 0.80; 95% CI 0.64–0.99) was more evident in DM patients for the secondary outcome of vascular death (interaction p = 0.037).
The safety of rivaroxaban versus warfarin regarding MB (HRs 1.00 and 1.12 for patients with and without DM, respectively; interaction p = 0.43), or non-major clinically relevant bleeding (HRs 0.98 and 1.09; interaction p = 0.17), and intracranial hemorrhage (ICH) (HRs 0.62 and 0.72; interaction p = 0.67) was independent of DM status. As would be expected, adjusted exploratory analyses suggested 1.3-, 1.5-, and 1.9-fold higher 2-year rates of stroke, vascular mortality, and myocardial infarction in DM patients, respectively [34].
In the RE-LY trial, the 4221(23.3%) patients with DM were younger (70.9 vs 71.7 years), more likely to have hypertension (86.6% vs 76.5%), CAD (37.4% vs 24.9%), and PAD (5.6% vs 3.2%) (all p < 0.01). Time in therapeutic range for warfarin-treated patients was 65% for diabetic versus 68% for non-diabetic patients (p < 0.001). Regardless of assigned treatment, SSE was more common among patients with DM (1.9% per year vs 1.3% per year, p < 0.001). DM was also associated with an increased risk of death (5.1% per year vs 3.5% per year, p < 0.001) and MB (4.2% per year vs 3.0% per year, p < 0.001). The absolute reduction in SSE with dabigatran compared to warfarin was greater among patients with DM than in those without DM (dabigatran 110 mg: 0.59% per year vs 0.05% per year; dabigatran 150 mg: 0.89% per year vs 0.51% per year). Therefore, compared to non-DM patients, AF patients with DM derive a greater absolute risk reduction in embolic events when treated with dabigatran [35]. In another pre-specified analysis of RE-LY, a multiple logistic regression model showed that the risk of ischemic events was inversely related to trough dabigatran concentrations (p = 0.045), with age and previous stroke (both p < 0.0001) as significant covariates and that MB risk increased with dabigatran exposure (p < 0.0001), age (p < 0.0001), acetylsalicylic acid use (p < 0.0003), and diabetes (p = 0.018) as significant covariates [40, 41].
The 4547 (24.9%) diabetic patients enrolled in the ARISTOTLE trial were younger (69 vs 70 years), had more CAD (39 vs 31%) and higher mean CHADS2 (2.9 vs 1.9) and HAS-BLED scores (1.9 vs 1.7) (all p < 0.0001) than patients without DM. Patients with diabetes receiving apixaban had lower rates of SSE (HR 0.75, 95% CI 0.53–1.05), all-cause mortality (HR 0.83, 95% CI 0.67–1.02), CV mortality (HR 0.89, 95% CI 0.66–1.20), intracranial hemorrhage (HR 0.49, 95% CI 0.25–0.95), and a similar rate of myocardial infarction (HR 1.02, 95% CI 0.62–1.67) compared with warfarin. For MB, a quantitative interaction was seen (interaction p = 0.003) with a greater reduction in MB in patients without diabetes even after multivariable adjustment. Other measures of bleeding showed a consistent reduction with apixaban compared with warfarin without a significant interaction based on diabetes status [36, 42]. With regard to edoxaban, the primary outcomes were consistent in the 7624 (36%) patients with DM [33]. Patients with diabetes receiving edoxaban had similar rates of SSE (risk ratio 0.91, 95% CI 0.69–1.19) compared with warfarin. Of note, the use of edoxaban 60 mg was associated with significant decrease in MB irrespective of diabetes status (risk ratio 0.78, 95% CI 0.63–0.95 in DM vs 0.81, 95% CI 0.69–0.95 in no-DM) confirming a good safety of edoxaban in this setting [39]. An additional subgroup analysis stratified 21,105 patients in ENGAGE AF-TIMI into pre-specified categories: no-DM (n = 13,481); non-insulin-dependent DM (NIDDM, n = 6354); and IDDM (n = 1270). Patients with IDDM were younger (mean age 68.8 vs 69.5 vs 71.3 yrs) and had higher BMIs (32.9 vs 31.0 vs 28.4 kg/m2) and CHA2DS2–VASc scores (mean 4.8 vs 4.6 vs 4.2) as compared to those with NIDDM or no-DM (each p < 0.001). The annualized rate of the net outcome of stroke/SEE, MB, or CV death was 7.2% in no-DM versus 7.0% in NIDDM (adjusted HR 1.15) versus 11.2% in IDDM (adjusted HR 1.80), both p < 0.001. Secondary outcomes followed similar patterns. The efficacy and safety profiles of edoxaban as compared to warfarin were not modified by DM status (each interaction p > 0.10). [43].
Taken together, these studies seem to confirm at least a similar efficacy and safety trade-off compared to warfarin in patients with or without diabetes. However, single trials may be underpowered to specifically evaluate clinical results of DOACs in definite subgroups of patients, especially for endpoints at low incidence. Moreover, they differ with regard to the inclusion of participants with diabetes, since criteria for the diagnosis of diabetes were mostly based on either documentation of diabetes at baseline or the use of glucose-lowering medications. Furthermore, most trials did not report data on HbA1c or blood glucose levels. Of note, all the phase III trials excluded participants with severe chronic kidney disease, thus possibly also excluding patients with diabetic nephropathy, a subgroup with higher risk of vascular complications and marked bleeding tendency [44]. On the other hand, several studies have shown that patients in treatment with VKAs have increased coronary and renal artery calcification, which, in turn, could be responsible of a higher risk of cardiac events and of an acceleration in the decline of renal function in diabetic individuals [45]. In the RE-LY study, the decline in renal function, after an average of 30 months, was more substantial in patients taking warfarin versus dabigatran, and it was greater in people with diabetes and in previous VKA users [40]. Renal calcinosis VKAs-related may at least partially play a role in inducing an anticoagulant-related nephropathy, caused by glomerular hemorrhage, tubular injury, and obstruction due to red blood cell casts, and observed more frequently with VKA than with DOACs [46, 47]. Furthermore, since warfarin inhibits the vitamin K-dependent gamma-glutamyl carboxylation of proteins, including osteocalcin and matrix Gla protein, it may increase the risk of osteoporotic bone fracture and some authors raise concerns about its use in diabetic patients with AF [45, 48].
A study-level meta-analysis [39], including 18,134 patients with DM and 40,454 without DM, highlighted that the use of DOACs compared with warfarin similarly reduced SSE in diabetic (RR 0.80, 95% CI 0.68–0.93; p = 0.004) and non-diabetic patients (RR 0.83, 95% CI 0.73–0.93; p = 0.001) (interaction p = 0.72). No interaction between diabetes status and benefits of DOACs was found for the occurrence of ischemic stroke, MB, or intracranial bleeding (p for interaction > 0.05 for each comparison). Notably, reduction in vascular death rates with DOACs was significant in diabetic patients (4.97% vs 5.99% with warfarin; RR 0.83, 95% CI 0.72–0.96; p = 0.01), in whom the absolute reduction in this outcome measure was higher than in non-diabetics (1.02% vs 0.27%), although no interaction was present (p = 0.23). The number needed to treat for this outcome measure with DOACs was 98 in diabetic patients and 370 in non-diabetic ones. In light of the current evidence, a recent Consensus Statement from the Working Group on Thrombosis of the Italian Society of Cardiology recommends oral anticoagulant therapy, and preferably a DOAC, for patients affected by AF and diabetes [49].
Antithrombotic strategies for patients with atrial fibrillation undergoing percutaneous coronary intervention
According to the recent 2018 joint European consensus document [50], DOACs as part of triple antithrombotic therapy or dual antithrombotic therapy are safer than VKAs with respect to bleeding risk and are preferable to VKAs in the absence of contraindications to the use of these drugs in anticoagulated AF patients undergoing PCI. Three randomized trials on DOAC versus VKA in combination with antiplatelets for patients with AF undergoing PCI have been recently published [51,52,53], and at least another large trial is ongoing [55]. The design and the principal outcomes of PIONEER AF PCI [51], RE-DUAL PCI [52], AUGUSTUS [53], and ENTRUST-AF-PCI [54] are summarized in Table 2. All these trials are designed to evaluate safety and are not sufficiently powered for ischemic outcomes. With regards to diabetes status, 624 (29, 4%) patients enrolled in the PIONEER trial presented DM among comorbidities at baseline. No specific subgroup analysis is available for these patients [51]. In the RE-DUAL study, a total of 1296 (37%) DM patients were randomized to dual therapy with dabigatran or triple therapy with VKA. The results were consistent in patients with or without diabetes for both primary and secondary endpoints (all interaction p values > 0.05) [52]. The more recent AUGUSTUS trial studied apixaban as part of dual or triple therapy in patients with AF and ACS or PCI, involving 1678 (36.4%) patients with DM. In this two-by-two factorial design trial, the effects of apixaban as compared with VKA and of aspirin as compared with placebo were generally consistent across pre-specified subgroups with regard to bleeding events. Conversely, a significant interaction was found in the DM subgroup for the secondary outcome of death or ischemic events. Indeed, the cumulative incidence of death or ischemic events was higher in DM patients (8.6%) as compared with no diabetic patients (5.9%) with a trend toward advantage of treatment with VKA in the DM group (HR 1.30; 95% CI 0.94–1.81 in favor of VKA; interaction p = 0.007). No significant interaction was observed between the two randomization factors with regard to death or hospitalization (interaction p = 0.053) [53]. Lastly, the ENTRUST trial (NCT02866175) is still ongoing and a pre-specified subgroup analysis for patients with DM is planned [54].
Secondary prevention of CAD and PAD
Patients with established CV disease may suffer further CV events, despite receiving optimal medical treatment. Although platelet inhibition plays a central role in the prevention of new events and improves outcomes in patients with atherothrombotic disease, principally by the thromboxane A2 and the ADP P2Y12 platelet activation pathways, it minimally affects other pathways, while agonists such as thrombin, considered to be the most potent platelet activator, continue to stimulate platelet activation and thrombosis [55]. The recent COMPASS (Rivaroxaban for the Prevention of Major Cardiovascular Events in Coronary or Peripheral Artery Disease) study [56] investigated the effects of the inhibition of thrombin generation, evaluating 27,395 participants with stable atherosclerotic vascular disease randomized to receive rivaroxaban (2.5 mg twice daily) plus aspirin (100 mg once daily), rivaroxaban (5 mg twice daily), or aspirin (100 mg once daily). A total of 90.6% of the participants had a history of CAD, and 27.3% had a history of PAD. The mean age was 68 years, and the majority of participants (78%) were men. This study was prematurely stopped for superiority of the rivaroxaban plus aspirin versus aspirin-alone group after a mean follow-up of 23 months in terms of major adverse cardiovascular events (MACE) such as CV death, MI, or stroke and all-cause death. Indeed, the combination arm resulted in a 24% reduction in the primary endpoint of CV death, stroke, or MI, and an 18% reduction in mortality (3.4 vs 4.1%, HR 0.82, 95% CI 0.71–0.96; p = 0.01). When separately examining components of the primary outcome, the combination treatment produced a larger relative effect on stroke than on CV death and MI: Stroke was reduced by 42% and ischemic stroke by 49%. As reported in a recent detailed analysis on stroke outcomes, age, systolic blood pressure (SBP) at baseline, history of hypertension, diabetes, prior stroke, and Asian ethnicity all resulted as independent predictors of stroke. Prior stroke was the strongest predictor of incident stroke (HR 3.63, 95% CI 2.65–4.97, p < 0.0001) and was associated with a 3.4% per year rate of stroke recurrence on aspirin. Excluding patients with prior stroke, independent risk factors for stroke included age (≥ 75 vs < 65 HR 1.71, 95% CI 1.20–2.44, p < 0.0001), SBP at entry (≥ 140 vs ≤ 120 HR 1.66, 95% CI 1.16–2.37, p = 0.01), history of hypertension (HR 1.36, 95% CI 1.01–1.84, p = 0.05), diabetes (HR 1.46, 95% CI 1.15–1.84, p = 0.002), and Asian ethnicity (HR 1.69, 95% CI 1.27–2.25, p = 0.001). Similar effects of combination treatment were seen across all the subgroups identified, as predictors of stroke occurrence with no significant treatment interactions [57]. Interestingly, hemorrhagic stroke resulted associated with SBP, tobacco use, prior stroke, and Asian ethnicity but not with diabetes (HR 0.82; 95% CI 0.45–1.47, p = 0.50), age > 75 years (HR 2.10; 95% CI 0.82–5.36, p = 0.29) or hypertension (HR 1.20, 95% CI 0.61–2.37, p = 0.60), suggesting, for the latter subgroups, a greatest benefit of the combination therapy in terms of reduction in ischemic events without any significant increase in bleeding. Equally, consistent with the overall study results, in patients with diabetes (n = 10,241; 37, 4%), addition of rivaroxaban to aspirin resulted in significantly lower incidence of MACE (HR 0.74, 95% CI 0.61–0.90; interaction p = 0.68) with expected higher rates of MB (HR 1.70, 95% CI 1.25–2.31) (Table 3). The net clinical benefit of the overall population was significantly in favor of combination therapy (HR 0.80; 95% CI 0.70–0.91; p < 0.001), without increased rates of ICH (HR 1.16; 95% CI 0.67–2.00; p = 0.60) [57]. Results in participants with CAD and in those with PAD were also consistent [58, 59] and occurred regardless of diabetic status. Furthermore, in the high-risk PAD population, the HR for major adverse limb events (MALE, defined as acute limb ischemia or intervention for chronic limb ischemia) was 0.54 (95% CI 0.35–0.84); p = 0.0054, and the HR for major amputation was 0.30 (95% CI 0.11–0.80); p = 0.011, without a concerning increase in ICH. Patients with PAD and diabetes (n = 3287; 44% of PAD subgroup) receiving rivaroxaban plus aspirin had a twofold higher absolute reduction in the composite endpoint (CV death, MI, and stroke) than patients with PAD but without diabetes. Interestingly, the mortality benefit of the COMPASS study was unique in trials of long-term antithrombotics and it is likely to influence future treatment guidelines for patients with stable CV disease. Combination therapy is particularly promising for the PAD population, for which few effective treatments have been proven. In addition, the ongoing VOYAGER PAD trial (NCT02504216) is evaluating the efficacy and safety of the vascular dose of rivaroxaban (2.5 mg twice daily) in patients with symptomatic PAD undergoing peripheral surgical and/or endovascular revascularization [60].
Treatment of venous thromboembolism
The role of diabetes as independent predictor of VTE is uncertain. In a recent analysis of individual participant data from the Emerging Risk Factors Collaboration and the UK Biobank including 1.1 million participants, among a range of established CV risk factors, older age, smoking, and greater adiposity were consistently associated with higher VTE risk. Conversely, there were inconsistent associations of VTE with diabetes and blood pressure [61]. In general, the presence of DM does not influence standard antithrombotic treatment. Accordingly, no specific subgroup analyses have been performed on patients with diabetes in VTE trials comparing DOACs and warfarin and, to our knowledge, no data on specific subgroups are available [62].
Metabolism of direct oral anticoagulants and of non-insulin anti-diabetic drugs: potential drug–drug interactions
One of the advantages of DOACs over VKAs is their predictable pharmacokinetic (PK) and pharmacodynamic profile with fewer interactions with drugs, foods, and herbal medicines and, in turn, fewer clinically significant DDIs [63]. Knowledge regarding interactions, with effect on plasma levels and especially on clinical effects of DOAC drugs, is currently growing, so new information may modify existing recommendations in the near future [64]. Likewise, little information is available, so far, on the potential interactions between DOACs and glucose-lowering agents. However, because DOACs have multiple elimination pathways, they have no clinically relevant interactions with most commonly prescribed medications. All DOACs are substrates of the permeability glycoprotein (P-gp). This cell efflux transporter mediates the export of drugs from cells located in the small intestine, blood–brain barrier, hepatocytes, and kidney proximal tubule. Intestinal absorption, biliary excretion, and urinary excretion of P-gp substrates can be altered by either the inhibition or induction of P-gp [65]. In addition, PK of DOACs may be partially affected by the co-administration of inducers/inhibitors of cytochrome P450 (CYP) 3A4. Indeed, DOACs exposure will likely be increased by the administration of strong P-gp and CYP P450 3A4-inhibitors (e.g., ketoconazole or protease inhibitors of HIV) increasing the risk of bleeds. In general, DOAC use is not recommended in combination with drugs that are strong inhibitors of both CYP3A4 and P-gp. Conversely, strong inducers of P-gp and/or CYP3A4 (such as rifampicin or carbamazepine) will markedly reduce DOAC plasma levels; such combinations should be avoided or used with great caution and surveillance [64].
The clinical importance of any DDI depends on factors that are drug-, patient-, and administration-related. DM patients are generally geriatric and multimorbid subjects receiving polytherapy to reduce their CV risk, especially lipid-lowering agents, antihypertensive drugs, and antiplatelet medications. Thus, many DDIs may potentially contribute to harmful effects of glucose-lowering drugs. Fortunately, although CYP-mediated DDIs are numerous, most of them only moderately influence PK parameters without dramatically affecting efficacy or inducing clinically relevant adverse events. The effects of inducers or inhibitors of CYP have been tested on the metabolism and PK of oral anti-diabetics of each pharmacological class [66, 67]. A vast amount of small-sized in vitro studies and investigations, mostly including healthy volunteers and surrogate parameters of concomitant CV drug use, is available. Although current data suggest that modest PK interferences among some CV drug combinations exist, clinicians can be reassured because they do not seem to have substantial clinical consequences [68]. In Table 4, we report the involvement of CYP or P-gp on the metabolism of the most commonly prescribed glucose-lowering drugs. Because insulins are not described as inhibitors or inducers of human CYP, we do not report any information regarding them. Among non-insulin agents, no strong inducer or inhibitor of P-gp and/or CYP3A4 exists and no clinically relevant interactions are expected during the use of DOACs [69]. In addition, we highlight particular advice if reported in the summary of product characteristics of each drug [70].
Conclusions
DOACs have been extensively studied in large phase III trials. They represent an attractive option in the management of DM patients affected by CV diseases, being at least as effective and safe as in non-DM patients. Current data suggest that they may improve the prognosis of such patients and a vast amount of evidence regarding their net clinical benefit is still growing fast. Specifically, in AF diabetic patients, treatment with DOACs was associated with a significant 17% relative reduction in vascular death compared with warfarin [49]. In addition, results from the COMPASS trial are reassuring in terms of reduction in MI, stroke, vascular death, and all-cause death both in patients with CAD and PAD. Ongoing analyses and studies are promising for the diabetic PAD population [57, 61]. However, clinicians should reserve particular caution to patients with severe chronic kidney disease, as DOACs are contraindicated in this situation. Finally, yet importantly, no clinically relevant interactions are expected during the concomitant use of DOACs with most anti-diabetic drugs.
Abbreviations
- DM:
-
Diabetes mellitus
- CV:
-
Cardiovascular
- CAD:
-
Coronary artery disease
- ACS:
-
Acute coronary syndrome
- PAD:
-
Peripheral arterial disease
- AF:
-
Atrial fibrillation
- DOACs:
-
Direct oral anticoagulants
- VTE:
-
Venous thromboembolism
- PCI:
-
Percutaneous coronary intervention
- PK:
-
Pharmacokinetic
- DDIs:
-
Drug–drug interactions
- RR:
-
Relative risk
- CI:
-
Confidence interval
- HR:
-
Hazard ratio
- MI:
-
Myocardial infarction
- SSE:
-
Stroke/systemic embolism
- VKA:
-
Vitamin K antagonists
- MB:
-
Major bleeding
- NIDDM:
-
Non-insulin-dependent DM
- IDDM:
-
Insulin-dependent DM
- ICH:
-
Intracranial hemorrhage
- MACE:
-
Major adverse cardiovascular events
- SBP:
-
Systolic blood pressure
- MALE:
-
Major adverse limb events
- P-gp:
-
Permeability glycoprotein
- CYP:
-
Cytochrome
References
Standards of Medical Care in Diabetes (2018) Abridged for primary care providers. American Diabetes Association. Clin Diabetes 36(1):14–37
Kodama S, Tanaka S, Heianza Y et al (2013) Association between physical activity and risk of all-cause mortality and cardiovascular disease in patients with diabetes: a meta-analysis. Diabetes Care 36(2):471–479
Vetrone LM, Zaccardi F, Webb DR et al (2019) Cardiovascular and mortality events in type 2 diabetes cardiovascular outcomes trials: a systematic review with trend analysis. Acta Diabetol 56(3):331–339
Rawshani A, Rawshani A, Franzén S et al (2017) Mortality and cardiovascular disease in type 1 and type 2 diabetes. N Engl J Med 376(15):1407–1418
Lin J, Thompson TJ, Cheng YJ et al (2018) Projection of the future diabetes burden in the United States through 2060. Popul Health Metr 16(1):9
http://www.cdc.gov/diabetes/statistics/prevalence_national.htm. Accessed 20 Apr 2019
Marzona I, Avanzini F, Lucisano G et al (2017) Are all people with diabetes and cardiovascular risk factors or microvascular complications at very high risk? Findings from the Risk and Prevention Study. Acta Diabetol 54(2):123–131
Ramezankhani A, Azizi F, Hadaegh F, Momenan AA (2018) Diabetes and number of years of life lost with and without cardiovascular disease: a multi-state homogeneous semi-Markov model. Acta Diabetol 55(3):253–262
Ferreiro JL, Angiolillo DJ (2011) Diabetes and antiplatelet therapy in acute coronary syndrome. Circulation 123(7):798–813
Pomero F, Di Minno MN, Fenoglio L, Gianni M, Ageno W, Dentali F (2015) Is diabetes a hypercoagulable state? A critical appraisal. Acta Diabetol 52(6):1007–1016
Cavender MA, Steg PG, Smith SC Jr, REACH Registry Investigators et al (2015) Impact of diabetes mellitus on hospitalization for heart failure, cardiovascular events, and death: outcomes at 4 years from the reduction of atherothrombosis for continued health (REACH) registry. Circulation 132(10):923–931
De Caterina R, Ageno W, Agnelli G et al (2019) The non-vitamin K antagonist oral anticoagulants in heart disease: section V-special situations. Thromb Haemost 119(1):14–38
Tadic M, Cuspidi C (2015) Type 2 diabetes mellitus and atrial fibrillation: from mechanisms to clinical practice. Arch Cardiovasc Dis 108(4):269–276
Movahed MR, Hashemzadeh M, Jamal MM (2005) Diabetes mellitus is a strong, independent risk for atrial fibrillation and flutter in addition to other cardiovascular disease. Int J Cardiol 105:315–318
Ruigomez A, Johansson S, Wallander MA, Rodriguez LA (2002) Incidence of chronic atrial fibrillation in general practice and its treatment pattern. J Clin Epidemiol 55:358–363
Johansen OE, Brustad E, Enger S, Tveit A (2008) Prevalence of abnormal glucose metabolism in atrial fibrillation: a case control study in 75-year old subjects. Cardiovasc Diabetol 7:28
Huxley RR, Filion KB, Konety S et al (2011) Meta-analysis of cohort and case-control studies of type 2 diabetes mellitus and risk of atrial fibrillation. Am J Cardiol 108:56–62
Fatemi O, Yuriditsky E, Tsioufis C et al (2014) Impact of intensive glycemic control on the incidence of atrial fibrillation and associated cardiovascular outcomes in patients with type 2 diabetes mellitus (from the Action to Control Cardiovascular Risk in Diabetes Study). Am J Cardiol 114:1217–1222
Stroke Risk in Atrial Fibrillation Working Group (2007) Independent predictors of stroke in patients with atrial fibrillation: a systematic review. Neurology 69:546–554
Ashburner JM, Go AS, Chang Y et al (2016) Effect of diabetes and glycemic control on ischemic stroke risk in AF patients: ATRIA study. J Am Coll Cardiol 67:239–247
Patti G, Lucerna M, Cavallari I et al (2017) Insulin-requiring versus noninsulin-requiring diabetes and thromboembolic risk in patients with atrial fibrillation: PREFER in AF. J Am Coll Cardiol 69:409–419
Gage BF, Waterman AD, Shannon W et al (2001) Validation of clinical classification schemes for predicting stroke: results from the National Registry of Atrial Fibrillation. JAMA 285:2864–2870
Lip GY, Nieuwlaat R, Pisters R et al (2010) Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest 137:263–272
KirchhofP BS, Kotecha D et al (2016) 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J 37:2893–2962
Ryden L, Grant PJ, Anker SD, Berne C et al (2014) ESC guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD—summary. Diabetes Vasc Dis Res 11:133–173
January CT, Wann LS, Alpert JS et al (2014) 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol 64:e1–e76
Chao TF, Liu CJ, Wang KL et al (2015) Should atrial fibrillation patients with 1 additional risk factor of the CHA2DS2-VASc score (beyond sex) receive oral anticoagulation? J Am Coll Cardiol 65(7):635–642
Olesen JB, Lip GY, Hansen ML et al (2011) Validation of risk stratification schemes for predicting stroke and thromboembolism in patients with atrial fibrillation: nationwide cohort study. BMJ 342:d124
Plitt A, McGuire DK, Giugliano RP (2017) Atrial fibrillation, type 2 diabetes, and non-vitamin K antagonist oral anticoagulants: a review. JAMA Cardiol 2(4):442–448
Connolly SJ, Ezekowitz MD, Yusuf S et al (2009) Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med 361:1139–1151
Granger CB, Alexander JH, McMurray JJ et al (2011) Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med 365:981–992
Patel MR, Mahaffey KW, Garg J, Pan G et al (2011) Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med 365:883–891
Giugliano RP, Ruff CT, Braunwald E et al (2013) Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med 369:2093–2104
Bansilal S, Bloomgarden Z, Halperin JL et al (2015) Efficacy and safety of rivaroxaban in patients with diabetes and nonvalvular atrial fibrillation: the Rivaroxaban Once-daily, Oral, Direct Factor Xa Inhibition Compared with Vitamin K Antagonism for Prevention of Stroke and Embolism Trial in Atrial Fibrillation (ROCKET AF Trial). Am Heart J 170(4):675.e8–682.e8
Brambatti M, Darius H, Oldgren J et al (2015) Comparison of dabigatran versus warfarin in diabetic patients with atrial fibrillation: results from the RE-LY trial. Int J Cardiol 196:127–131
Ezekowitz JA, Lewis BS, Lopes RD et al (2015) Clinical outcomes of patients with diabetes and atrial fibrillation treated with apixaban: results from the ARISTOTLE trial. Eur Heart J Cardiovasc Pharmacother 1(2):86–94
Rost NS, Giugliano RP, Ruff CT, ENGAGE AF-TIMI 48 Investigators et al (2016) Outcomes with edoxaban versus warfarin in patients with previous cerebrovascular events: findings from ENGAGE AF-TIMI 48 (Effective Anticoagulation With Factor Xa Next Generation in Atrial Fibrillation-Thrombolysis in Myocardial Infarction 48). Stroke 47(8):2075–2082
Diener HC, Connolly SJ, Ezekowitz MD, RE-LY study group et al (2010) Dabigatran compared with warfarin in patients with atrial fibrillation and previous transient ischaemic attack or stroke: a subgroup analysis of the RE-LY trial. Lancet Neurol 9(12):1157–1163
Patti G, Di Gioia G, Cavallari I, Nenna A (2017) Safety and efficacy of non-vitamin K antagonist oral anticoagulants versus warfarin in diabetic patients with atrial fibrillation: a study-level meta-analysis of phase III randomized trials. Diabetes Metab Res Rev 33(3):e2876
Mumoli N, Mastroiacovo D, Tamborini-Permunian E et al (2017) Dabigatran in nonvalvular atrial fibrillation: from clinical trials to real-life experience. J Cardiovasc Med (Hagerstown) 18(7):467–477
Reilly P, Lehr T, Haertter S, RE-LY Investigators et al (2014) The effect of dabigatran plasma concentrations and patient characteristics on the frequency of ischemic stroke and major bleeding in atrial fibrillation patients: the RE-LY Trial (Randomized Evaluation of Long-Term Anticoagulation Therapy). J Am Coll Cardiol 63(4):321–328
Hylek EM, Held C, Alexander JH et al (2014) Major bleeding in patients with atrial fibrillation receiving apixaban or warfarin: the ARISTOTLE Trial (Apixaban for Reduction in Stroke and Other Thromboembolic Events in Atrial Fibrillation): Predictors, Characteristics, and Clinical Outcomes. J Am Coll Cardiol 63(20):2141–2147
Plitt A, Ruff C, Goudev A et al (2016) Abstract 16551: efficacy and safety of oral anticoagulation in 21105 patients with atrial fibrillation stratified by diabetic status in the ENGAGE AF-TIMI 48 Trial. Circulation 134(suppl_1):16551
Penno G, Solini A, Bonora E, Renal Insufficiency and Cardiovascular Events (RIACE) Study Group et al (2018) Defining the contribution of chronic kidney disease to all-cause mortality in patients with type 2 diabetes: the renal insufficiency and cardiovascular events (RIACE) Italian Multicenter Study. Acta Diabetol 55(6):603–612
Yamagishi SI (2019) Concerns about clinical efficacy and safety of warfarin in diabetic patients with atrial fibrillation. Cardiovasc Diabetol 18(1):12
Brodsky SV, Hebert L (2016) Anticoagulant-related nephropathy: an AKI elephant hiding in plain view? J Am Coll Cardiol 68(21):2284–2286
Chan Y-H, Yeh Y-H, Hsieh MY et al (2018) The risk of acute kidney injury in Asians treated with apixaban, rivaroxaban, dabigatran, or warfarin for non-valvular atrial fibrillation: a nationwide cohort study in Taiwan. Int J Cardiol 265:83–89
Gu ZC, Zhou LY, Shen L et al (2018) Non-vitamin K antagonist oral anticoagulants vs. warfarin at risk of fractures: a systematic review and meta-analysis of randomized controlled trials. Front Pharmacol 9:348
Patti G, Cavallari I, Andreotti F, Working Group on Thrombosis of the Italian Society of Cardiology et al (2019) Prevention of atherothrombotic events in patients with diabetes mellitus: from antithrombotic therapies to new-generation glucose-lowering drugs. Nat Rev Cardiol 16(2):113–130
Lip GYH, Collet JP, Haude M, ESC Scientific Document Group et al (2019) Joint European consensus document on the management of antithrombotic therapy in atrial fibrillation patients presenting with acute coronary syndrome and/or undergoing percutaneous cardiovascular interventions: a joint consensus document of the European Heart Rhythm Association (EHRA), European Society of Cardiology Working Group on Thrombosis, European Association of Percutaneous Cardiovascular Interventions (EAPCI), and European Association of Acute Cardiac Care (ACCA) endorsed by the Heart Rhythm Society (HRS), Asia-Pacific Heart Rhythm Society (APHRS), Latin America Heart Rhythm Society (LAHRS), and Cardiac Arrhythmia Society of Southern Africa (CASSA). Europace 21(2):192–193
Gibson CM, Mehran R, Bode C et al (2016) Prevention of bleeding in patients with atrial fibrillation undergoing PCI. N Engl J Med 375:2423–2434
Cannon CP, Bhatt DL, Oldgren J et al (2017) Dual antithrombotic therapy with dabigatran after PCI in atrial fibrillation. N Engl J Med 377:1513–1524
Lopes RD, Heizer G, Aronson R et al (2019) Antithrombotic therapy after acute coronary syndrome or PCI in atrial fibrillation. N Engl J Med 380:1509–1524
Vranckx P, Lewalter T, Valgimigli M et al (2018) Evaluation of the safety and efficacy of an edoxaban-based antithrombotic regimen in patients with atrial fibrillation following successful percutaneous coronary intervention (PCI) with stent placement: rationale and design of the ENTRUST-AF PCI trial. Am Heart J 196:105–112
Angiolillo DJ, Capodanno D, Goto S (2010) Platelet thrombin receptor antagonism and atherothrombosis. Eur Heart J 31(1):17–28
Eikelboom JW, Connolly SJ, Bosch J et al (2017) Rivaroxaban with or without Aspirin in stable cardiovascular disease. N Engl J Med 377(14):1319–1330
Sharma M, Hart RG, Connolly SJ et al (2019) Stroke outcomes in the COMPASS trial. Circulation 139(9):1134–1145
Connolly SJ, Eikelboom JW, Bosch J, COMPASS investigators et al (2018) Rivaroxaban with or without aspirin in patients with stable coronary artery disease: an international, randomised, double-blind, placebo-controlled trial. Lancet 391(10117):205–218
Anand SS, Bosch J, Eikelboom JW, COMPASS Investigators et al (2018) Rivaroxaban with or without aspirin in patients with stable peripheral or carotid artery disease: an international, randomised, double-blind, placebo-controlled trial. Lancet 391(10117):219–229
Capell WH, Bonaca MP, Nehler MR et al (2018) Rationale and design for the Vascular Outcomes study of ASA along with rivaroxaban in endovascular or surgical limb revascularization for peripheral artery disease (VOYAGER PAD). Am Heart J 199:83–91
Gregson J, Kaptoge S, Bolton T et al (2019) Emerging risk factors collaboration. cardiovascular risk factors associated with venous thromboembolism. JAMA Cardiol 4(2):163–173
Blann AD, Lip GY (2016) Non-vitamin K antagonist oral anticoagulants (NOACs) for the management of venous thromboembolism. Heart 102(12):975–983
Prisco D, Ageno W, Becattini C, SIMI (Italian Society of Internal Medicine); FADOI (Federation of Associations of Hospital Doctors on Internal Medicine); SISET (Italian Society for the Study of Haemostasis and Thrombosis) et al (2017) Italian intersociety consensus on DOAC use in internal medicine. Intern Emerg Med 12(3):387–406
Steffel J, Verhamme P, Potpara TS, ESC Scientific Document Group et al (2018) The 2018 European Heart Rhythm Association Practical Guide on the use of non-vitamin K antagonist oral anticoagulants in patients with atrial fibrillation. Eur Heart J 39(16):1330–1393
Wessler JD, Grip LT, Mendell J, Giugliano RP (2013) The P-glycoprotein transport system and cardiovascular drugs. J Am Coll Cardiol 61(25):2495–2502
Abbasi MM, Valizadeh H, Hamishehkar H, Zakeri-Milani P (2016) Inhibition of P-glycoprotein expression and function by anti-diabetic drugs gliclazide, metformin, and pioglitazone in vitro and in situ. Res Pharm Sci 11(3):177–186
Scheen AJ (2011) Cytochrome P450-mediated cardiovascular drug interactions. Expert Opin Drug Metab Toxicol 7(9):1065–1082
Ruscica M, Baldessin L, Boccia D, Racagni G, Mitro N (2017) Non-insulin anti-diabetic drugs: an update on pharmacological interactions. Pharmacol Res 115:14–24
Gelosa P, Castiglioni L, Tenconi M et al (2018) Pharmacokinetic drug interactions of the non-vitamin K antagonist oral anticoagulants (NOACs). Pharmacol Res 135:60–79
www.ema.europa.eu/en/documents/product-information. Accessed 13 May 2019
Acknowledgements
We gratefully acknowledge D’Anna Stefano for the study of potential drug–drug interactions.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to declare.
Ethical standard
This article does not contain any studies with human partecipants or animals performed by any of the authors.
Informed consent
For this type of study formal consent is not required.
Additional information
Managed By Massimo Porta.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pomero, F., Dentali, F., Mumoli, N. et al. The continuous challenge of antithrombotic strategies in diabetes: focus on direct oral anticoagulants. Acta Diabetol 56, 1247–1258 (2019). https://doi.org/10.1007/s00592-019-01426-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-019-01426-2