Abstract
Aims
Frequent glucose testing is required for optimal management of type 1 diabetes (T1D). Limited data are available regarding real-world experience of the novel technology for monitoring by continuous interstitial fluid glucose (IFG), using flash glucose-sensing technology (FSL-CGM). We aimed to assess the effect of FSL-CGM in a real-life clinical setting on glycemic control parameters, compliance, and adverse events among pediatric and young adult T1D patients.
Methods
This observational multi-center study assessed FSL-CGM use (6–12 months) in T1D patients (mean ± SD age 13.4 ± 4.9 years) who purchased the device out-of-pocket. Outcome measures included HbA1c, mean IFG levels, CGM metrics [time in hypoglycemia (< 54 mg/dL; < 3 mmol/L), in target range (70–180 mg/dL; 3.9–10 mmol/L), and in hyperglycemia > 240 mg/dL; > 13.3 mmol/L)], frequency of self-monitoring of blood glucose, acute complications, skin reactions, and reasons for initiation/discontinuation.
Results
Among patients with regular use of the FSL-CGM (n = 59), mean HbA1c decreased from 8.86 ± 0.23 to 8.05 ± 0.2% (73.3–64.5 mmol/mol) in 3 months (p = 0.0001) and plateaued thereafter. A clinically significant reduction in HbA1c (defined as a decrease of ≥ 0.5%) was associated with shorter diabetes duration. Of 71 patients who initiated use of the FSL-CGM, 12 (16.9%) discontinued during the study period. No statistically significant changes were found after FSL-CGM use, in mean and standard deviation IFG levels, and in time of glucose levels in target, hypoglycemia, and hyperglycemia ranges. One patient with hypoglycemia unawareness was found dead-in-bed while using FSL-CGM.
Conclusions
Real-life observational data in a self-selected young T1D population demonstrated a significant and sustained reduction in HbA1c with FSL-CGM in one-third of the participants. Surveillance of glucose monitoring should be individualized, especially for patients with hypoglycemia unawareness.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Glucose monitoring by frequent assessments is mandatory for the optimal management of patients with type 1 diabetes (T1D). Self-monitoring of blood glucose (SMBG) by finger prick tests has been the standard of care for diabetes for the last few decades [1]; its value for better glycemic control has been clearly demonstrated among all insulin-treated patients whether treated by multiple daily insulin injections or by continuous subcutaneous insulin infusion (CSII) [2]. During the last decade, continuous glucose monitoring systems (CGMs) with alarms of hypoglycemia and hyperglycemia have been introduced. The advantages of such technology are the provision of more complete information of the real-time level of interstitial fluid glucose (IFG), including the demonstration of trends and rates of change of IFG. CGMs as a standalone device or in combination with CSII leads to improvements in HbA1c, with reduced risk of hypoglycemic events [3,4,5]. Moreover, new generations of sensor-augmented pump systems are able to reduce time spent in hypoglycemia by suspending insulin infusion when glucose is (or predicted to be) low [6,7,8]. However, limitations of CGM devices have restricted their widespread use, including: discomfort when wearing them, insertion difficulties, the need of SMBG testing for calibration, problems related to the adhesiveness of the sensor, their numerous alarms, concerns about accuracy of data, interference with sports and activities, the need for frequent change, and skin reactions [9, 10]. Decreased usage of CGMs over time was demonstrated in a number of real-life studies in pediatric populations [9,10,11].
A novel technology for continuous IFG monitoring was introduced in the last few years, using Flash glucose-sensing technology: FreeStyle Libre (FSL-CGM Abbott Diabetes Care, Alameda, California, USA). The advantages of this device over other CGMs are that the sensor is replaced every 14 rather than 6–7 days and that calibration is not required. Similar to other CGMs, data are shown real time on a screen, including rate and direction of change in glucose levels. However, the FSL-CGM has no alarms, thus does not alert pending hypoglycemia or hyperglycemia, and glucose-level reading is available only on-demand. The use of FSL-CGM was shown to be reliable, to increase time in target range, easy to wear, and well tolerated by T1D patients [12,13,14,15,16]. A few short-term studies (14 days–3 months) demonstrated the accuracy, safety, and acceptability of this device in pediatric populations [12, 14, 17, 18].
Our aim was to describe real-life data of children and youth using FSL-CGM for 6–12 months, including glycemic control parameters, compliance, and adverse events.
Patients and methods
Study population
The study population included all individuals with T1D ages 1–25 years who were managed by the pediatric diabetes teams from the AWeSoMe Study Group (four pediatric diabetes multidisciplinary clinics in Israel; Assaf Harofeh Medical Center, E. Wolfson Medical Center, Edmond and Lily Safra Children’s Hospital, Dana-Dwek Children’s Hospital) and who chose to purchase FSL-CGM out-of-pocket as part of their diabetes care in addition to the reimbursed finger-stick blood glucose monitoring. The decision to use FSL-CGM was made prior to and independent of their entrance to the study, and was based on preferences of the patients and their parents. Study eligibility criteria included: diagnosis of T1D, routine attendance at clinic visits, and initiation of FSL-CGM usage between April 2016 and March 2017. Patients who discontinued FSL-CGM usage were not excluded from the study, and there were no restrictions on HbA1c value or prior use of CGM. Patients were categorized according to duration of FSL-CGM usage: those who used the FSL-CGM for the entire follow-up period and those who discontinued the use of the device during the follow-up period.
Study design
This is an observational real-life multi-center study, based on data retrieved from charts as part of clinical care at each clinic visit during 6–12 months follow-up, and conducted according to the principles of the Declaration of Helsinki on biomedical research involving human patients and the respective local national regulations. Each center obtained local ethics committee approval. Since data were retrieved from patient medical records, and all personal identification information omitted, informed consent by the patients was waived. Patients arrived for follow-up visits every 3–6 months as is routine in the participating clinics. Management decisions were made per routine practice and were based on FSL-CGM downloaded logbooks, downloaded data of insulin pumps, and HbA1c. All patients received guidance from a diabetes team regarding FGS-CGM use during the first 3 months of system use.
Data collection
Pre-specified clinical data were collected from a period of 6 months before until 12 months after the start of FSL-CGM use. Pre-FSL-CGM was defined as the period prior to FSL-CGM use; the most recent 2-week data were collected from the medical records for the 6- and 3-month visits prior to FSL-CGM initiation and from the first clinical visit with the FSL-CGM, from glucometer and pump data downloading. Variables recorded at the first visit with the FSL-CGM were gender, age, diabetes duration, other medical diseases, weight, height, and Tanner pubertal stage (by routine physical examination during clinical visits in the diabetes clinic). Variables recorded at each visit included: HbA1c levels, as obtained with a DCA point of care device, the number of SMBG per day, the number of device scans, episodes of diabetic ketoacidosis (DKA), and severe hypoglycemia (defined as glucose level < 54 mg/dL; < 3 mmol/L and requiring treatment by another person), height, weight, body mass index (BMI), and skin assessment at the insertion site of the FSL-CGM (itching, redness, and hyper-pigmentation).
Outcome measures
Primary outcome measures were changes in glycemic parameters including HbA1c, mean glucose levels, time in hypoglycemia (< 54 mg/dL; < 3 mmol/L), in target range (70–180 mg/dL; 3.9–10 mmol/L), and in hyperglycemia (> 240 mg/dL; < 13.3 mmol/L), from the pre-FSL-CGM period until the end of follow-up. Secondary outcome measures were the effect of FSL-CGM on SMBG frequency, the number of device scans per day, episodes of acute diabetes complications (severe hypoglycemia and ketoacidosis), skin reactions, and causes for FSL-CGM initiation and discontinuation.
Statistical analysis
Data were analyzed with the IBM SPSS software (IBM SPSS Statistics for Windows, Version 24; IBM Corp., Armonk, NY, USA, 2016). Categorical variables were described as frequency and percent. Continuous variables were assessed for normal distribution using histogram and Q–Q plots. Normally distributed continuous variables were described as means and standard deviations (SD), and non-normally distributed parameters were described as median and interquartile range (IQR). Categorical variables were compared between those who discontinued using FSL-CGM and those who continued, using Chi-square test or Fisher’s exact test. Differences between groups in continuous data were compared using independent-sample t tests (normally distributed data) or Mann–Whitney test (skewed data). The Generalized Estimating Equation (GEE) model was used to evaluate the change in each outcome during the follow-up time. Data analysis was controlled for diabetes duration prior to FSL-CGM. Interaction between each baseline parameter and time was also assessed. The last observation carried forward method was used for imputation of missing data in the 12-month period. A two-tailed p value of ≤ 0.05 was considered significant.
Results
Characteristics of the study population
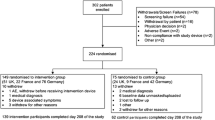
The study population comprised 71 children, adolescents, and young adults with T1D, 56.3% females; the mean age at baseline was 13.4 ± 4.9 years (range 4.1–23.8 years). Five patients were preschoolers (age 1–6 years), 24 children (6–12 years), 29 adolescents (12–18 years), and 18 young adults (18–25 years). The demographic, clinical, and glycemic control parameters are presented in Table 1.
Fifty-nine patients (83.1%) used FSL-CGM for the entire follow-up period, with a median duration of 10.3 months (IQR 6.0, 12.5). Twelve patients (16.9%) discontinued the use of FSL-CGM during the follow-up period, with a median usage time of 5.6 months (IQR 2.8, 7.4). Reasons for discontinuation were switch to a CGM with alarms (n = 4), tired of the device (n = 3), severe skin reactions (n = 2), perception of inaccuracy (n = 2), and too expensive (n = 1). Most characteristics assessed were similar between patients who continued and discontinued use of the device (Table 1). Baseline characteristics demonstrated that those who discontinued use of the device, compared to those who continued, had significantly higher HbA1c [9.3% (IQR 8.9, 11.0) vs. 8.2% (IQR 7.5, 9.4), 78 mmol/mol (IQR 74, 97) vs. 66 mmol/mol (IQR 58, 79), p = 0.02], and a lower proportion of time with glucose in range [37.3% (IQR 25.5, 53.0) vs. 52.6% (IQR 41, 62.7), p = 0.06]. None of those who discontinued had prior experience with CGM (Table 1). Fourteen patients (19.7%) started to use the FSL-CGM less than 6 months after diagnosis of T1D. Three patients discontinued usage due to fear of hypoglycemia and switched to CGM devices with alarms.
Parameters of glycemic control during the follow-up period among the continuous users of the FSL-CGM
HbA1c decreased by 0.8 ± 0.03% (9 mmol/mol) at 3 months (mean ± SE, respectively, p = 0.0001), and plateaued thereafter (Fig. 1a). We defined an improvement in glycemic control as a decrease of ≥ 0.5% in HbA1c. This clinically significant decrease in HbA1c during the follow-up period was observed in 24 patients (40.6% of the continuous users of the FSL-CGM), 9 of them were with diabetes duration less than 6 months, and 15 with more than 6 months disease duration, as presented in Fig. 1. The clinically significant improvement in HbA1c over time was associated with shorter diabetes duration (p value for interaction = 0.001).
A clinically significant decrease in HbA1c was not associated with gender, age at FSL-CGM initiation, modality of insulin delivery, previous use of a CGM, and SMBG/day at baseline (p = 0.643, p = 0.683, p = 0.290, p = 0.054, p = 0.659, respectively), as presented in Table 2. No significant changes were observed following use of the device in mean glucose and SD, and in the proportion of time that blood glucose values were in the target, hypoglycemic, and hyperglycemic ranges (Fig. 2).
Evolution of time in hypoglycemia, in range, and in hyperglycemia before and until 12 months after start of use of FSL-CGM. In the pre-FSL-CGM, data are based on averages of SMBG data. Other data points represent mean (standard error) percentage of FSL-CGM measurements a below 54 mg/dL (3 mmol/L), b 70–180 mg/dL (3.9–10 mmol/L), and c above 240 mg/dL (13.3 mmol/L) at 3, 6, and 12 months after initiation of use of the device
The number of SMBG tests performed per day significantly decreased from a median of 5.2 (IQR 2.5, 7.0) in the Pre-FSL-CGM period to a median of zero tests per day during the follow-up period (IQR 0, 2.6, p = 0.001). The median number of sensor scans per day during the follow-up was 12 (IQR 8, 16.5) and was stable during the entire study period. No association was found between a decrease in HbA1c and the number of scans performed daily (Table 2).
Reasons for initiating FSL-CGM use
The most common reason for using FSL-CGM, as expressed by 37 (54%) patients and their parents, was to improve their quality of life; this reason was more often stated than the other reason (p = 0.04). Additional reasons were to improve diabetes control (n = 9, 12.7%), to improve compliance of glucose assessment (n = 3, 4.2%), to reduce the frequency of hypoglycemia (n = 2, 2.8%), and to avoid hypoglycemia unawareness (n = 1, 1.4%). Nineteen patients expressed various combinations of reasons (26.8%).
Adverse events during FGS-CGM use
Considering the entire cohort, contact dermatitis presented in 9 (12.7%) patients. Of them, dermatitis appeared within 3 months of FSL-CGM use in 5, and after 6 months in 4. Two patients with severe dermatitis stopped using the device because of skin reactions (16.7% of the patients who discontinued use of the device), which presented shortly after initiation of use of the FSL-CGM. Of note, these patients had experienced similar skin reactions to other adhesives used in diabetes-related devices. Seven patients continued using the FSL-CGM despite the skin reactions, and used various protective barrier dressings.
No episode of DKA was reported during the follow-up period, while four episodes were documented in the pre- FGS-CGM period.
Two severe hypoglycemia episodes were documented during the FSL-CGM period, in a 23-year-old female patient with well-controlled Hashimoto thyroiditis. She had a similar incidence of hypoglycemic events during the pre-FSL-CGM period and a history of hypoglycemia unawareness. She refused to use a CGM with alert devices and used the FSL-CGM intermittently. During the two severe episodes, the device was not in use. She was found dead-in-bed after a total of 8 months of intermittent use of FSL-CGM while using the system. Her mean HbA1c during the 6 months prior to FSL-CGM was 7.8%, and on her last visit 8.6%.
Discussion
This is the first long-term real-life report of FSL-CGM use in the pediatric and young adult T1D population. In this cohort of 71 self-selected participants, we were able to demonstrate various aspects of routine use of this new device: reasons for initiation and discontinuation, adverse events, and changes in glycemic control parameters.
In a subgroup of patients with shorter disease duration (< 6 months) and higher initial HbA1c, we demonstrated a clinically and statistically significant decrease in HbA1c (≥ 0.5%), shortly after initiation of using the device. Still, one-third of the patients with diabetes longer than 6 months showed a similar decrease. Several studies of adult patients with T1D demonstrated a decrease in HbA1c following use of the FSL-CGM [19,20,21].
Dunn et al. analyzed real-life data of 50,000 users (with type 1 and type 2 diabetes) of the FSL-CGM worldwide [16]. That study showed that estimated HbA1c gradually decreased from 8.0 to 6.7% (64–50 mmol/mol). Moreover, a strong correlation was shown between the number of glucose scans and improvement in glycemic parameters. Previously, a greater number of SMBG were shown to be associated with better HbA1c [1, 2]. However, in our pediatric and young adult population with T1D, the number of self-tests per day was higher following FSL-CGM use (median 12 scans vs. 5.2 finger pricks). However, no correlation was found between the number of scans per day and HbA1c reduction, possibly due to the smaller study population, which was not powered to show such a correlation. The frequency of SMBG dramatically decreased among FSL-CGM users. This phenomenon has been described in other studies as well, and reflects the confidence of the users in the device [15, 22].
We presume that the “honeymoon period” may explain, at least in part, the more frequent clinically significant decreases in HbA1c in patients who were diagnosed with T1D within 6 months of initiating use of the device compared to patients with longer disease duration. A marked reduction in HbA1c is a well-documented phenomenon that occurs shortly after diagnosis of T1D [23] and that is related to the initiation of insulin treatment and some recovery of beta cell function. Nonetheless, one-third of patients with prolonged disease also achieved a clinically significant reduction in HbA1c. We were not able to characterize the patients with improved glycemic control, since the decrease in HbA1c was not associated with gender, age at FSL-CGM initiation, modality of insulin delivery, and previous use of a CGM and SMBG/day at baseline.
As in every new technology that seems flawless in controlled research, introduction to the relevant patient population highlights troublesome areas. Nearly, 17% of the study population, all of them naïve to CGM devices, stopped using the FLS-CGM during the follow-up period. The various reasons for discontinuation resemble those that have been described for the discontinuation of other CGMs [9, 10]. An additional reason for discontinuation was fear of hypoglycemia, which the FSL-CGM does not warn against. Interestingly, the majority of those who discontinued use due to fear of hypoglycemia were with relatively new onset T1D (less than 6 months from diagnosis). As reported recently, patients with hypoglycemia unawareness benefit more from other CGM devices than from the FSL-CGM system [24]. The young adult found dead-in-bed was a patient with hypoglycemia unawareness, and her death may have been associated with hypoglycemia. An additional reason for discontinuing FSL-CGM use is contact dermatitis, which is typical of adhesive use, and which occurred in 13% of our study population. Similarly, adverse skin events were described by Bolinder and al. in a cohort of adults with type 1 diabetes who were using the FSL-CGM [25]. Herman et al. described 15 patients from a dermatology clinic with contact dermatitis attributed to isobornyl acrylate (a component in the adhesive part of the device) [26]. Local skin reaction is an occasional adverse event of medical devices attached to the body, and local preventive measures have been reported [27]. We note that none of the patients with a previous history of CGM discontinued use of the FLS-CGM during the study period. About 30% of the cohort switched to the FSL-CGM, because they found the alarms of other CGMs annoying and the presence of continuously visible glucose levels overwhelming and interfering with daily life.
Limitations of the current study include the absence of blinded FSL-CGM data prior to FSL-CGM use; this is a limitation inherent to an observational real-life study design and the absence of a prospective control group. Other limitations are the relatively small number of patients and the selected population of patients who could self-fund the device. Strengths of the study are the real-life population, which included patients with a wide range of HbA1c (6.1–16.1%), the relatively long use experience, the multi-center design and the analysis of the largest pediatric, and youth population using the FSL-CGM reported thus far.
In a real-life context, FSL-CGM use resulted in a significant and sustained reduction in HbA1c among one-third of patients with prolonged duration of diabetes. Although underpowered, this report raises questions regarding the clinical relevance of adult population reports for the pediatric population, and highlights the need for large scale real-life assessments of FGS-CGM in the pediatric population, and of defining the patients who will benefit the most from the device. The data have several clinical implications for FSL-CGM use in pediatric and young adult patients with T1D, including its consideration among patients with hypoglycemia unawareness. Tailoring glucose monitoring to patients of different characteristics is important to improve glycemic control and prevent complications.
Change history
12 September 2018
Unfortunately, the co-author name was misspelled as “Avivit Brenner” instead of “Avivit Brener” in the original publication and the correct author name is updated here
References
Ziegler R, Heidtmann B, Hilgard D et al (2011) Frequency of SMBG correlates with HbA1c and acute complications in children and adolescents with type 1 diabetes. Pediatr Diabetes 12:11–17. https://doi.org/10.1111/j.1399-5448.2010.00650.x
Miller KM, Beck RW, Bergenstal RM et al (2013) Evidence of a strong association between frequency of self-monitoring of blood glucose and hemoglobin A1c levels in T1D exchange clinic registry participants. Diabetes Care 36:2009–2014. https://doi.org/10.2337/dc12-1770
Bergenstal RM, Tamborlane WV, Ahmann A et al (2010) Effectiveness of sensor-augmented insulin-pump therapy in type 1 diabetes. N Engl J Med 363:311–320. https://doi.org/10.1056/NEJMoa1002853
Juvenile Diabetes Research Foundation Continuous Glucose Monitoring Study Group, Tamborlane WV, Beck RW et al (2008) Continuous glucose monitoring and intensive treatment of type 1 diabetes. N Engl J Med 359:1464–1476. https://doi.org/10.1056/NEJMoa0805017
Charleer S, Mathieu C, Nobels F et al (2018) Effect of continuous glucose monitoring on glycemic control, acute admissions and quality of life: a real-world study. J Clin Endocrinol Metab. https://doi.org/10.1210/jc.2017-02498
Hermanides J, Nørgaard K, Bruttomesso D et al (2011) Sensor-augmented pump therapy lowers HbA1c in suboptimally controlled Type 1 diabetes; a randomized controlled trial. Diabet Med 28:1158–1167. https://doi.org/10.1111/j.1464-5491.2011.03256.x
Weiss R, Garg SK, Bode BW et al (2015) Hypoglycemia reduction and changes in hemoglobin A1c in the ASPIRE in-home study. Diabetes Technol Ther 17:542–547. https://doi.org/10.1089/dia.2014.0306
Battelino T, Nimri R, Dovc K et al (2017) Prevention of hypoglycemia with predictive low glucose insulin suspension in children with type 1 diabetes: a randomized controlled trial. Diabetes Care 40:764–770. https://doi.org/10.2337/dc16-2584
Wong JC, Foster NC, Maahs DM et al (2014) Real-time continuous glucose monitoring among participants in the T1D Exchange clinic registry. Diabetes Care 37:2702–2709. https://doi.org/10.2337/dc14-0303
Rachmiel M, Landau Z, Boaz M et al (2015) The use of continuous glucose monitoring systems in a pediatric population with type 1 diabetes mellitus in real-life settings: the AWeSoMe Study Group experience. Acta Diabetol 52:323–329. https://doi.org/10.1007/s00592-014-0643-6
Juvenile Diabetes Research Foundation Continuous Glucose Monitoring Study Group (2010) Effectiveness of continuous glucose monitoring in a clinical care environment: evidence from the Juvenile Diabetes Research Foundation continuous glucose monitoring (JDRF-CGM) trial. Diabetes Care 33:17–22. https://doi.org/10.2337/dc09-1502
Edge J, Acerini C, Campbell F et al (2017) An alternative sensor-based method for glucose monitoring in children and young people with diabetes. Arch Dis Child 102:543–549. https://doi.org/10.1136/archdischild-2016-311530
Bonora B, Maran A, Ciciliot S et al (2016) Head-to-head comparison between flash and continuous glucose monitoring systems in outpatients with type 1 diabetes. J Endocrinol Investig 39:1391–1399. https://doi.org/10.1007/s40618-016-0495-8
Al Hayek AA, Robert AA, Al Dawish MA (2017) Evaluation of FreeStyle libre flash glucose monitoring system on glycemic control, health-related quality of life, and fear of hypoglycemia in patients with type 1 diabetes. Clin Med Insights Endocrinol Diabetes 10:1179551417746957. https://doi.org/10.1177/1179551417746957
Bolinder J, Antuna R, Geelhoed-Duijvestijn P et al (2016) Novel glucose-sensing technology and hypoglycaemia in type 1 diabetes: a multicentre, non-masked, randomised controlled trial. Lancet 388:2254–2263. https://doi.org/10.1016/S0140-6736(16)31535-5
Dunn TC, Xu Y, Hayter G, Ajjan RA (2018) Real-world flash glucose monitoring patterns and associations between self-monitoring frequency and glycaemic measures: a European analysis of over 60 million glucose tests. Diabetes Res Clin Pract 137:37–46. https://doi.org/10.1016/j.diabres.2017.12.015
Szadkowska A, Gawrecki A, Michalak A et al (2017) Flash glucose measurements in children with type 1 diabetes in real-life settings: to trust or not to trust? Diabetes Technol Ther. https://doi.org/10.1089/dia.2017.0287
Massa GG, Gys I, Op ‘t Eyndt A et al (2018) Evaluation of the FreeStyle® libre flash glucose monitoring system in children and adolescents with type 1 diabetes. Horm Res Paediatr 89:189–199. https://doi.org/10.1159/000487361
Dover AR, Stimson RH, Zammitt NN, Gibb FW (2017) Flash glucose monitoring improves outcomes in a type 1 diabetes clinic. J Diabetes Sci Technol 11:442–443. https://doi.org/10.1177/1932296816661560
McKnight JA, Gibb FW (2017) Flash glucose monitoring is associated with improved glycaemic control but use is largely limited to more affluent people in a UK diabetes centre. Diabet Med 34:732–732. https://doi.org/10.1111/dme.13315
Ish-Shalom M, Wainstein J, Raz I, Mosenzon O (2016) Improvement in glucose control in difficult-to-control patients with diabetes using a novel flash glucose monitoring device. J Diabetes Sci Technol 10:1412–1413. https://doi.org/10.1177/1932296816653412
Haak T, Hanaire H, Ajjan R et al (2017) Use of flash glucose-sensing technology for 12 months as a replacement for blood glucose monitoring in insulin-treated type 2 diabetes. Diab Ther 8:573–586. https://doi.org/10.1007/s13300-017-0255-6
Duca LM, Wang B, Rewers M, Rewers A (2017) Diabetic ketoacidosis at diagnosis of type 1 diabetes predicts poor long-term glycemic control. Diabetes Care 40:1249–1255. https://doi.org/10.2337/dc17-0558
Reddy M, Jugnee N, El Laboudi A et al (2018) A randomized controlled pilot study of continuous glucose monitoring and flash glucose monitoring in people with type 1 diabetes and impaired awareness of hypoglycaemia. Diabet Med 35:483–490. https://doi.org/10.1111/dme.13561
Bolinder J, Antuna R, Geelhoed-Duijvestijn P et al (2017) Cutaneous adverse events related to FreeStyle libre device—authors’ reply. Lancet 389:1396–1397. https://doi.org/10.1016/S0140-6736(17)30893-0
Herman A, Aerts O, Baeck M et al (2017) Allergic contact dermatitis caused by isobornyl acrylate in Freestyle® Libre, a newly introduced glucose sensor. Contact Dermat 77:367–373. https://doi.org/10.1111/cod.12866
Englert K, Ruedy K, Coffey J et al (2014) Skin and adhesive issues with continuous glucose monitors: a sticky situation. J Diabetes Sci Technol 8:745–751. https://doi.org/10.1177/1932296814529893
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflicts of interest.
Human and animal rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the 1975 Declaration of Helsinki, as revised in 2008.
Informed consent
Each center obtained local ethics committee approval before enrollment. Because there was no identification of the patients for whom data were retrieved, informed consent by the patients was waived.
Additional information
Managed by Massimo Federici.
The original version of this article was revised: The co-author name was misspelled as “Avivit Brenner” instead of “Avivit Brener” in the original publication.
Rights and permissions
About this article
Cite this article
Landau, Z., Abiri, S., Gruber, N. et al. Use of flash glucose-sensing technology (FreeStyle Libre) in youth with type 1 diabetes: AWeSoMe study group real-life observational experience. Acta Diabetol 55, 1303–1310 (2018). https://doi.org/10.1007/s00592-018-1218-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-018-1218-8