Abstract
Aims
Insulin autoantibodies (IAA) are often the first marker of autoimmunity detected in children in the preclinical phase of type 1 diabetes (T1D). Currently, the vast majority of laboratories adopt the radiobinding micro-assay (RBA) for measuring IAA. Our aim was to replace RBA with a novel non-radioactive IAA Luciferase Immuno Precipitation System (LIPS) assay with improved performance.
Methods
We developed (pro)insulin antigens with alternative placements of a NanoLuc™ luciferase reporter (NLuc). Performance in LIPS was evaluated by testing sera from new onset T1D (n = 80), blood donors (n = 123), schoolchildren (n = 186), first-degree relatives (FDRs) from the Bart’s Oxford family study (n = 53) and from the Belgian Diabetes Registry (n = 136), coded sera from the Islet Autoantibody Standardization Program (IASP) (T1D n = 50, blood donors n = 90).
Results
IAA LIPS based on B chain-NLuc proinsulin or B chain-NLuc insulin, in which NLuc was fused at the C-terminus of the insulin B chain, required only 2 μL of serum and a short incubation time, showed high concordance with RBA (Spearman r = 0.866 and 0.833, respectively), high assay performance (B chain-NLuc proinsulin ROC-AUC = 0.894 and B chain-NLuc insulin ROC-AUC = 0.916), and an adjusted sensitivity at 95% specificity ranking on par with the best assays submitted to the two most recent IASP workshops. In FDRs, the IAA LIPS showed improved discrimination of progressors to T1D compared to RBA.
Conclusions
We established a novel high-performance non-radioactive IAA LIPS that might replace the current gold standard RBA and find wide application in the study of the IAA response in T1D.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Insulin autoantibodies (IAA) [1] are frequently the first autoantibodies detected in children in the preclinical phase of type 1 diabetes (T1D) [2]. Therefore, IAA measurement is a cornerstone of the study of the T1D natural history [3,4,5] and of all screening strategies aimed at identifying and enrolling children at increased T1D risk in prevention trials [6]. Currently, the vast majority of laboratories measuring IAA adopt the radiobinding micro-assay (RBA), based on the immunoprecipitation of radiolabeled 125I-insulin with patient serum [7, 8]. While years of effort, including several international standardization workshops, have led to assay improvements [9,10,11,12,13], compared with assays measuring other T1D autoantibodies, the IAA RBA shows lower concordance and reproducibility across laboratories, requires more serum and a lengthy incubation, and is critically dependent on a limited number of suppliers for the provision of radiolabeled tracer. Furthermore, a significant fraction of subjects identified as single IAA positive by RBA during screening do not progress to T1D, suggesting an imperfect discrimination of IAA responses truly correlated with disease progression [14].
Currently, novel IAA assays that aim to replace RBA are under active development, of which the most mature example is an ECL method [15,16,17]. In particular, most efforts are aimed at substituting radiolabeled tracers with non-radioactive and more stable antigens, reducing serum consumption and assay duration, while at the same time improving assay sensitivity, specificity, and prediction of future disease development [16, 18]. In this study, we report the development of a novel IAA assay based on the Luciferase Immuno Precipitation System (LIPS) [19,20,21,22,23,24], a format in which luciferase-tagged antigens are immunoprecipitated with test sera, aimed at retaining most features of the classical IAA RBA while avoiding its shortcomings.
Materials and methods
Study subjects
All procedures performed in the study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments. Informed consent was obtained from all individual participants included in the study. Samples (ESM Table 1) included 80 new onset T1D patients and 123 blood donors from the San Raffaele Scientific Institute; 186 non-diabetic schoolchildren and 53 non-diabetic first-degree relatives (FDRs) of patients with T1D, from the Bart’s Oxford (BOX) study [25]; 136 non-diabetic FDRs from the Belgian Diabetes Registry (BDR) family study [26]; 50 new onset T1D patients and 90 blood donor controls coded samples from the 2015 and 2016 Islet Autoantibody Standardization Program (IASP) workshops.
Recombinant luciferase-tagged antigens production
Custom synthetic genes (Eurofins Genomics GmbH, Munich, Germany) of recombinant proinsulin or insulin antigens tagged with a NanoLuc™ (NLuc) luciferase reporter (Promega, Madison WI, USA) were sub-cloned into a modified pCMVTNT™ vector (Promega). To express luciferase-tagged insulins, PC1/PC2 convertase recognition sites were replaced with those of furin convertases [27,28,29], allowing for cleavage of the C-peptide. Antigens were expressed by transfection into Expi293F™ cells (Expi293™ Expression System, Thermo Fisher Scientific Life Technologies, Carlsbad, CA, USA). After 48 h, cells were removed by centrifugation and the culture medium harvested stored frozen at − 80 °C as single-use aliquots. The recovered luciferase activity was quantified by seeding the wells of an OptiPlate™ 96-well plate (PerkinElmer, Waltham, MA, USA) with 25-μL aliquots of serial tenfold dilutions of the antigen in 50 mM tris buffer, 1% Tween-20, pH 8 (TBT) followed by the addition of 40 μL of Nano-Glo® substrate (Promega), mixing and measurement of light units (LU) bioluminescence for 2 s/well in a Berthold Centro XS3 luminometer (Berthold Technologies GmbH & Co. KG, Bad Wildbad, Germany).
IAA LIPS assay
Antigens were diluted with TBT to adjust the luciferase activity to a final concentration of 107 LU/25 μL, and then filtered with a Durapore™ PVDF 0.45-μm Millex-HV syringe filter (Millipore, Billerica, MA, USA). Immunoprecipitation was performed with and without competition of IAA binding using ACTRAPID® insulin (Novo Nordisk, Bagsværd, Denmark) added at a final concentration of 4.5 × 10−5 mol/L.
Four 2-μL replicates of each serum were pipetted into 96-deep-well plates (Beckman Coulter Inc., Brea, CA, USA), 25 μL of antigen w/o competitor was added to half of the replicates, while the rest received antigen plus competitor. Plates were then mixed briefly on a rotary shaker, centrifuged for 2′ at 500g at 4 °C, and incubated for 24 h at 4 °C. Immunocomplexes were captured by incubation with 5 μL of blocked [12] rProtein A and 2.5 μL of G Sepharose 4Fast Flow in 50 μL TBT (GE Healthcare Europe GmbH, Freiburg, Germany), for 1 h at 4 °C, with shaking. Plates were washed 5 times by sequential dispensing of 750 μL of TBT per well, centrifugation at 500g for 2′ at 4 °C, and removal of supernatant using a micro-plate plate washer (BioTek Instruments Inc., Winooski, VT, USA). Resin pellets were then transferred to an OptiPlate™, and the luciferase activity was measured after addition of each well with 40 μL of Nano-Glo® substrate, followed by a 2′′ readout in the luminometer.
Acquired LU were converted to arbitrary units (AU) using a standard curve constructed from nine doubling dilutions in normal human serum of either a IAA positive serum or the monoclonal antibody HUI018 (Dako, Glostrup, Denmark), whose epitope is centered against the A chain loop of human insulin [30]. AU were calculated based on the delta of measured LU between competed and non-competed wells, using a logarithmic curve fitting algorithm in Excel (Microsoft Corporation, Redmond, WA, USA). All samples in which LU of non-competed replicates was below those of competed replicates were given a fixed value of 0.01 AU. The anti C-peptide monoclonal antibody C-PEP-01 (Santa Cruz Biotechnology, Inc. Dallas, TX, USA), directed against an epitope within the central part of the C-peptide [31], was used to check presence or absence of the C-peptide in the labeled antigen.
Statistical analysis
Statistical analysis was performed using the Prism v6 software (GraphPad Software, Inc., La Jolla CA, USA) and the pROC package for the R software [32, 33]. The area under the receiver operating characteristic (ROC) curve was used to verify the ability of the IAA LIPS test to discriminate cases from controls. Concordance of quantitative results of assays was assessed by calculating the Spearman’s r correlation coefficient. Survival curves following Kaplan–Meier analysis were compared using the Mantel–Haenszel Log-rank test.
Results
Expression and immunoprecipitation of (pro)insulin luciferases
We generated and expressed in eukaryotic cells as secreted recombinant proteins eight different (pro)insulin luciferase constructs in which the NLuc reporter was placed either at the NH2 or COOH termini of the insulin A or B chains (Fig. 1). We evaluated, by immunoprecipitation, antibody binding to each of the expressed (pro)insulin luciferases using serial dilutions of the HUI018 mAb (against a conformational epitope in the insulin A chain), the C-PEP01 mAb (against an epitope in the C-peptide), and two human sera, IAA positive and negative, respectively. All immunoprecipitations were performed with and without competition of binding using unlabeled insulin, as per the classical IAA RBA protocol. Our results show that the HUI018 mAb specifically bounds to all constructs and that the C-peptide was correctly removed from the insulin antigens (ESM Fig. 1a, b). Prolonged storage of the antigens at − 80 °C did not affect significantly luciferase activity or antibody binding up to 10 months post-freezing (ESM Fig. 2). Five constructs were selected for further analysis in LIPS using human sera: sNLuc proinsulin, B chain-NLuc proinsulin, B chain-NLuc insulin, NLuc-A chain proinsulin, and NLuc-A chain insulin.
Schematic representation of recombinant luciferase-tagged (pro)insulin antigens showing the placement of the NLuc reporter (black arrows) relative to the insulin B chain (white arrows) A chain (gray arrows) and C-peptide (black line). Dashed lines indicate the mutagenesis of recognition sites for native PC1/PC2 convertase to those of furin proteases
Performance in LIPS of alternative (pro)insulin luciferases
We conducted a preliminary evaluation of performance in LIPS of the selected (pro)insulin luciferases using 5 μL of serum per replicate, competition with unlabeled insulin, and 48 h incubation. All the antigens discriminated in LIPS newly diagnosed T1D (n = 76) from control (n = 81) sera, albeit with variable efficiency as measured by the analysis of the area under the ROC curve (ROC-AUC) (ESM Fig. 3a, b). Two constructs, in which the NLuc reporter was joined at the COOH terminus of the B chain and preceding the C-peptide (B chain-NLuc proinsulin and B chain-NLuc insulin), were selected for further study.
The B chain-NLuc proinsulin LIPS was then used to test FDRs from the BOX family study [25] that included high-risk subjects (n = 15), who either developed T1D or tested positive for multiple T1D autoantibodies, and low-risk subjects, who tested negative for other T1D autoantibodies and were either positive (n = 18) or negative (n = 20) for IAA in RBA (Fig. 2). The threshold for positivity was placed at the 97.5th percentile of AU measured by LIPS in serum samples from 186 healthy schoolchildren for both LIPS and RBA. The B chain-NLuc proinsulin LIPS showed a ROC-AUC of 0.877 (95% CI 0.762–0.993, p < 0.0001) compared to 0.774 for RBA (95% CI 0.648–0.899, p = 0.002). While the two ROC-AUCs were not statistically different (p = 0.214), a comparison of ROC-AUCs at a specificity greater than 90% showed a trend toward significance in this limited sample set (p = 0.088) (ESM Fig. 4).
B chain-NLuc proinsulin LIPS results (clear symbols) compared to RBA (gray symbols) in progressors/high-risk (diamonds n = 15) and non-progressors/low-risk (pointed circles n = 38) FDRs from the BOX study (dotted and dashed lines indicate the thresholds for positivity of RBA and LIPS placed at the 97.5th percentile of titers 186 non-diabetic schoolchild shown as clear circles)
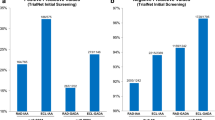
In blind evaluation of IAA LIPS assays in IASP workshops
The B chain-NLuc proinsulin and insulin LIPS assay performance was verified by testing independently in two laboratories sets of coded human sera obtained from the IASP2015 and IASP2016 workshops. Both laboratories achieved for the B chain-NLuc proinsulin LIPS an adjusted sensitivity at 95% specificity (AS95) of 64%, ranking first of the 23 IAA assays that reported results for the 2015 workshop, and an AS95 of 50 and 47.9%, ranking third and fourth of the 25 assays reporting results in the IASP2016. The B chain-NLuc insulin LIPS showed an AS95 of 64% in IASP2015, again at the first rank of all assays in that workshop, and of 50 and 43.7% in IASP2016, at the third and sixth rank of all assays in the 2016 workshop.
The concordance of the B chain-NLuc proinsulin LIPS between the two laboratories was high, both as raw data in LU (Spearman r = 0.967, p < 0.0001 in T1D samples; Spearman r = 0.618, p < 0.0001 in control samples) and in AU (Spearman r = 0.974, p < 0.0001 in T1D samples; r = 0.541, p < 0.0001 in controls) (ESM Fig. 5). In addition, a variety of experimental conditions including reduced serum volume and assay incubation lengths were evaluated, showing that a comparable assay performance could be achieved by using only 2 μL of serum and shortening the assay incubation to 18 h (ESM Fig. 6).
Optimized B chain-NLuc (pro)insulin LIPS performance
Optimized LIPS assays using 2 μL of serum per replicate and 24-h incubation were evaluated in new onset T1D (n = 80) and control (n = 123) samples. The proinsulin LIPS showed a ROC-AUC of 0.894 (95% CI 0.841–0.946, p < 0.0001), while the insulin LIPS showed a ROC-AUC of 0.916 (95% CI 0.872–0.960, p < 0.0001) (Fig. 3). The results in T1D sera were highly correlated between LIPS assays (Spearman r = 0.978, 95% CI 0.965–0.986, p < 0.0001) and between LIPS assays and RBA (B chain-NLuc proinsulin: Spearman r = 0.866, 95% CI 0.779–0.921, p < 0.0001; B chain-NLuc insulin: r = 0.833, 95% CI 0.726–0.901, p < 0.0001) (ESM Fig. 7).
B chain-NLuc proinsulin LIPS performance in FDRs
The optimized B chain-NLuc proinsulin LIPS assay was used to test in blind 136 FDRs from the BDR family study [26], and its results were compared to those of RBA. For both tests, the threshold for positivity was placed at the 99th percentile of control titers. A Kaplan–Meier analysis highlighted a different rate of progression to T1D in FDRs IAA positive in LIPS (n = 43) with a diabetes-free survival fraction at 225 months of follow-up of 47%, compared to 79% in the IAA negatives (n = 93) (Mantel–Haenszel Log-rank test p < 0.0001) (Fig. 4a). Diabetes-free survival at 240 months was 59.6% in the IAA positives in RBA (n = 44), compared to 74% in IAA negatives (n = 92) (Mantel–Haenszel Log-rank test p = 0.0804) (Fig. 4b). After grouping according to the concordance of LIPS and RBA results, the diabetes-free survival fraction in FDRs at 181 months was 40% in subjects positive both in LIPS and in RBA, 48% in subjects positive only in LIPS, 90% in the subjects that tested IAA positive only in RBA, and 78% in subjects negative for both assays (Fig. 4c).
Diabetes-free survival in 136 FDRs from the BDR study tested in the B chain-NLuc proinsulin LIPS (a) or RBA (b) or stratified according to presence or absence of IAA in both assays, (c) on the graphs are shown the number of progressors and the total number of subjects in each group and the p value of the Mantel–Haenszel Log-rank test
All FDRs who tested IAA positive exclusively in LIPS (n = 9) also had additional T1D associated autoantibodies (5 subjects with single additional GADA and 4 with multiple auto-Abs). During follow-up, progression to T1D was observed in 5 subjects of the 9 IAA positive only in LIPS (1 with a single GADA and in all 4 with multiple auto-Abs). Conversely, among the 10 FDRs who tested IAA positive exclusively in RBA, additional antibodies were found in only 4 subjects (2 single GADA, 1 single IA-2A, and 1 single ZnT8A positive) of which only one progressed to T1D at a later stage. After stratification of the FDRs according to the presence of other T1D autoantibodies (0–3 additional auto-Abs), the impact on T1D-free survival of IAA positivity in either LIPS or RBA did not reach statistical significance in any of the four grouping categories (ESM Fig. 8).
Discussion
In this study, we developed novel recombinant (pro)insulins tagged with a luciferase reporter and evaluated their performance as antigens for measuring IAA in LIPS, an immunoassay already successfully applied to the measurement of other T1D-associated autoantibodies [19,20,21,22,23,24].
Past studies led to the production of numerous variants of recombinant (pro)insulin proteins; however, we are aware of only two instances in which large GFP or firefly luciferase reporters were fused either within the C-peptide or at the carboxyl terminus of the proinsulin sequence [34, 35]. In both cases, the secretion of mature insulin from cells transfected with these tagged proinsulins could be confirmed, but was nevertheless associated with substantial misfolding and retention in the endoplasmic reticulum.
Initially, our work focused on the generation of (pro)insulins joined to NLuc [36], the smallest commercially available luciferase, and on the systematic analysis of parameters that could potentially affect IAA binding to NLuc-(pro)insulins, including the placement of the reporter relative to the antigen sequence. Our results indicate that, despite the NLuc relatively large size compared to proinsulin, NLuc-(pro)insulins are constitutively secreted by transfected eukaryotic cells and undergo post-translational modifications, including the removal of the C-peptide. More importantly, the engineered (pro)insulins appear to be at least partly correctly folded, an essential requirement for their use in assays measuring IAA [9], as implicitly demonstrated by their recognition, albeit with variable efficiency and background levels, by both monoclonal and human serum antibodies directed against conformational epitopes.
We selected two recombinant proteins in which NLuc was joined at the carboxyl terminus of the insulin B chain (B chain-NLuc proinsulin and B chain-NLuc insulin, respectively) as the most promising antigens for IAA measurement in LIPS. We further confirmed the ability of our IAA LIPS to discriminate cases from controls by testing in blind new onset T1D and blood donor sera distributed in IASP2015 and IASP2016, the most recent NIDDK sponsored workshops for the standardization of islet autoantibodies [13], and achieve a performance on a par with the best IAA assays that participated in the two workshops.
Overall, the comparison of LIPS and RBA results showed a high degree of correlation between the two tests, suggesting that the IAA responses measured by LIPS in new onset T1D patients are mostly consistent with those in obtained by RBA. Furthermore, our preliminary results in a selection of FDRs from the BOX study [25] and from the BDR [26] suggested that LIPS might be more sensitive and specific when used to discriminate future progressors to T1D from subjects with lower risk. However, while in isolation the IAA LIPS showed an advantage over RBA, our study was not sufficiently powered to clarify whether there might be an added benefit of IAA measurement by LIPS in discriminating progressors from non-progressors in the context of strategies based on multiple autoantibody testing. Similar to previous validation studies [18], only the testing of very large cohorts of subjects at risk of T1D will allow the superiority of the IAA LIPS assay over RBA for prediction of T1D, particularly in young children, to be confirmed.
Compared to RBA, LIPS offers several practical advantages, primarily in the avoidance of radiolabeled tracers, a major source of RBA variability and complexity, because of the short life of 125I-insulin and the cumbersome and expensive requirements linked to the use of radioactive substances. In addition to using a non-radioactive tracer with a potentially very long half-life, LIPS offers a greatly shortened assay duration and requires less than half the amount of serum (2 vs 5–30 μL per replicate), a noteworthy advantage when IAA testing is performed on precious and essentially irreplaceable archival samples collected for T1D natural history studies [37,38,39,40], or from capillary blood samples increasingly used for general population screening [6, 41].
Compared to ECL, another novel non-radioactive immunoassay and currently the only other successfully validated IAA assay format [15, 18], the IAA LIPS offers the benefit of reduced serum consumption, relies on relatively inexpensive and widely available equipment and commercial reagents, and is amenable to future implementation on more advanced micro-fluidic platforms [42, 43].
In conclusion, we have established a novel non-radioactive IAA test that offers high performance while preserving an assay procedure overall similar to the gold standard IAA RBA. This suggests that the IAA LIPS might become an easily transferable replacement for tests based on radiolabeled antigen that might find wide application in the study of the IAA response in T1D.
Abbreviations
- IAA:
-
Insulin autoantibodies
- T1D:
-
Type 1 diabetes
- FDR:
-
First-degree relative
- RBA:
-
Radiobinding micro-assay
- LIPS:
-
Luciferase Immuno Precipitation System
- BOX study:
-
Bart’s-Oxford study
- BDR:
-
Belgian Diabetes Registry
- IASP:
-
Islet Autoantibodies Standardization Program
- ROC-AUC:
-
Area under the receiver operator curve
- AS95:
-
Adjusted sensitivity at 95% specificity
- NLuc:
-
NanoLuc™ luciferase
- sNLuc:
-
Secretory NanoLuc™ luciferase
- LU:
-
Light units
- AU:
-
Arbitrary units
References
Palmer J, Asplin C, Clemons P et al (1983) Insulin antibodies in insulin-dependent diabetics before insulin treatment. Science 222:1337–1339. https://doi.org/10.1126/science.6362005
Krischer JP, Lynch KF, Schatz DA et al (2015) The 6 year incidence of diabetes-associated autoantibodies in genetically at-risk children: the TEDDY study. Diabetologia 58:980–987. https://doi.org/10.1007/s00125-015-3514-y
Ziegler AG, Hillebrand B, Rabl W et al (1993) On the appearance of islet associated autoimmunity in offspring of diabetic mothers: a prospective study from birth. Diabetologia 36:402–408
TEDDY Study Group (2007) The environmental determinants of diabetes in the young (TEDDY) study: study design. Pediatr Diabetes 8:286–298. https://doi.org/10.1111/j.1399-5448.2007.00269.x
Kupila A, Muona P, Simell T et al (2001) Feasibility of genetic and immunological prediction of type I diabetes in a population-based birth cohort. Diabetologia 44:290–297
Mahon JL, Sosenko JM, Rafkin-Mervis L et al (2009) The TrialNet natural history study of the development of type 1 diabetes: objectives, design, and initial results. Pediatr Diabetes 10:97–104. https://doi.org/10.1111/j.1399-5448.2008.00464.x
Williams AJ, Bingley PJ, Bonifacio E, Palmer JP, Gale EA (1997) A novel micro-assay for insulin autoantibodies. J Autoimmun 10:473–478. https://doi.org/10.1006/jaut.1997.0154
Naserke HE, Dozio N, Ziegler AG, Bonifacio E (1998) Comparison of a novel micro-assay for insulin autoantibodies with the conventional radiobinding assay. Diabetologia 41:681–683. https://doi.org/10.1007/s001250050968
Greenbaum CJ, Palmer JP, Kuglin B, Kolb H (1992) Insulin autoantibodies measured by radioimmunoassay methodology are more related to insulin-dependent diabetes mellitus than those measured by enzyme-linked immunosorbent assay: results of the fourth international workshop on the standardization of insulin autoantibody measurement. J Clin Endocrinol Metab 74:1040–1044. https://doi.org/10.1210/jcem.74.5.1569152
Achenbach P, Schlosser M, Williams AJK et al (2007) Combined testing of antibody titer and affinity improves insulin autoantibody measurement: Diabetes Antibody Standardization Program. Clin Immunol 122:85–90. https://doi.org/10.1016/j.clim.2006.09.004
Curnock RM, Reed CR, Rokni S, Broadhurst JW, Bingley PJ, Williams AJK (2012) Insulin autoantibody affinity measurement using a single concentration of unlabelled insulin competitor discriminates risk in relatives of patients with type 1 diabetes. Clin Exp Immunol 167:67–72. https://doi.org/10.1111/j.1365-2249.2011.04495.x
Williams AJK, Norcross AJ, Chandler KA, Bingley PJ (2006) Non-specific binding to protein A Sepharose and protein G Sepharose in insulin autoantibody assays may be reduced by pre-treatment with glycine or ethanolamine. J Immunol Methods 314:170–173. https://doi.org/10.1016/j.jim.2006.06.003
Schlosser M, Mueller PW, Törn C, Bonifacio E, Bingley PJ (2010) Diabetes Antibody Standardization Program: evaluation of assays for insulin autoantibodies. Diabetologia 53:2611–2620. https://doi.org/10.1007/s00125-010-1915-5
Steck AK, Vehik K, Bonifacio E et al (2015) Predictors of progression from the appearance of islet autoantibodies to early childhood diabetes: The Environmental Determinants of Diabetes in the Young (TEDDY). Diabetes Care 38:808–813. https://doi.org/10.2337/dc14-2426
Yu L, Miao D, Scrimgeour L, Johnson K, Rewers M, Eisenbarth GS (2012) Distinguishing persistent insulin autoantibodies with differential risk: nonradioactive bivalent proinsulin/insulin autoantibody assay. Diabetes 61:179–186. https://doi.org/10.2337/db11-0670
Miao D, Steck AK, Zhang L et al (2015) Electrochemiluminescence assays for insulin and glutamic acid decarboxylase autoantibodies improve prediction of type 1 diabetes risk. Diabetes Technol Ther 17:119–127. https://doi.org/10.1089/dia.2014.0186
Kikkas I, Mallone R, Tubiana-Rufi N et al (2013) A simple and fast non-radioactive bridging immunoassay for insulin autoantibodies. PLoS ONE 8:e69021. https://doi.org/10.1371/journal.pone.0069021
Fouts A, Pyle L, Yu L et al (2016) Do electrochemiluminescence assays improve prediction of time to type 1 diabetes in autoantibody-positive TrialNet subjects? Diabetes Care 39:1738–1744. https://doi.org/10.2337/dc16-0302
Burbelo PD, Kisailus AE, Peck JW (2002) Detecting protein-protein interactions using Renilla luciferase fusion proteins. Biotechniques 33:1044–1048, 1050
Burbelo PD, Goldman R, Mattson TL (2005) A simplified immunoprecipitation method for quantitatively measuring antibody responses in clinical sera samples by using mammalian-produced Renilla luciferase-antigen fusion proteins. BMC Biotechnol 5:22. https://doi.org/10.1186/1472-6750-5-22
Burbelo PD, Groot S, Dalakas MC, Iadarola MJ (2008) High definition profiling of autoantibodies to glutamic acid decarboxylases GAD65/GAD67 in stiff-person syndrome. Biochem Biophys Res Commun 366:1–7. https://doi.org/10.1016/j.bbrc.2007.11.077
Burbelo PD, Hirai H, Leahy H et al (2008) A new luminescence assay for autoantibodies to mammalian cell-prepared insulinoma-associated protein 2. Diabetes Care 31:1824–1826. https://doi.org/10.2337/dc08-0286
Lampasona V, Passerini L, Barzaghi F et al (2013) Autoantibodies to harmonin and villin are diagnostic markers in children with IPEX syndrome. PLoS ONE 8:e78664. https://doi.org/10.1371/journal.pone.0078664
McLaughlin KA, Richardson CC, Ravishankar A et al (2016) Identification of tetraspanin-7 as a target of autoantibodies in type 1 diabetes. Diabetes 65:1690–1698. https://doi.org/10.2337/db15-1058
Bingley PJ, Gale EA (1989) Incidence of insulin dependent diabetes in England: a study in the Oxford region, 1985–1986. BMJ 298:558–560
Gorus FK, Balti EV, Messaaoui A et al (2017) Twenty-year progression rate to clinical onset according to autoantibody profile, age, and HLA-DQ genotype in a registry-based group of children and adults with a first-degree relative with type 1 diabetes. Diabetes Care 40:1065–1072. https://doi.org/10.2337/dc16-2228
Groskreutz DJ, Sliwkowski MX, Gorman CM (1994) Genetically engineered proinsulin constitutively processed and secreted as mature, active insulin. J Biol Chem 269:6241–6245
Shaw JAM, Delday MI, Hart AW, Docherty HM, Maltin CA, Docherty K (2002) Secretion of bioactive human insulin following plasmid-mediated gene transfer to non-neuroendocrine cell lines, primary cultures and rat skeletal muscle in vivo. J Endocrinol 172:653–672. https://doi.org/10.1677/joe.0.1720653
Auricchio A, Gao G-P, Yu QC et al (2002) Constitutive and regulated expression of processed insulin following in vivo hepatic gene transfer. Gene Ther 9:963–971. https://doi.org/10.1038/sj.gt.3301746
Andersen L, Dinesen B, Jørgensen PN, Poulsen F, Røder ME (1993) Enzyme immunoassay for intact human insulin in serum or plasma. Clin Chem 39:578–582
Hilgert I, Stolba P, Kristofová H et al (1991) A monoclonal antibody applicable for determination of C-peptide of human proinsulin by RIA. Hybridoma 10:379–386
Robin X, Turck N, Hainard A et al (2011) pROC: an open-source package for R and S+ to analyze and compare ROC curves. BMC Bioinformatics 12:77. https://doi.org/10.1186/1471-2105-12-77
R Development Core Team (2005) R: a language and environment for statistical computing. R Development Core Team, Vienna
Pouli AE, Kennedy HJ, Schofield JG, Rutter GA (1998) Insulin targeting to the regulated secretory pathway after fusion with green fluorescent protein and firefly luciferase. Biochem J 331(Pt 2):669–675
Liu M, Hodish I, Rhodes CJ, Arvan P (2007) Proinsulin maturation, misfolding, and proteotoxicity. Proc Natl Acad Sci USA 104:15841–15846. https://doi.org/10.1073/pnas.0702697104
Hall MP, Unch J, Binkowski BF et al (2012) Engineered luciferase reporter from a deep sea shrimp utilizing a novel imidazopyrazinone substrate. ACS Chem Biol 7:1848–1857. https://doi.org/10.1021/cb3002478
Barker JM, Barriga KJ, Yu L et al (2004) Prediction of autoantibody positivity and progression to type 1 diabetes: Diabetes Autoimmunity Study in the Young (DAISY). J Clin Endocrinol Metab 89:3896–3902. https://doi.org/10.1210/jc.2003-031887
Ziegler AG, Rewers M, Simell O et al (2013) Seroconversion to multiple islet autoantibodies and risk of progression to diabetes in children. JAMA 309:2473–2479. https://doi.org/10.1001/jama.2013.6285
Parikka V, Näntö-Salonen K, Saarinen M et al (2012) Early seroconversion and rapidly increasing autoantibody concentrations predict prepubertal manifestation of type 1 diabetes in children at genetic risk. Diabetologia 55:1926–1936. https://doi.org/10.1007/s00125-012-2523-3
TEDDY Study Group (2008) The Environmental Determinants of Diabetes in the Young (TEDDY) study. Ann N Y Acad Sci 1150:1–13. https://doi.org/10.1196/annals.1447.062
Raab J, Haupt F, Scholz M et al (2016) Capillary blood islet autoantibody screening for identifying pre-type 1 diabetes in the general population: design and initial results of the Fr1da study. BMJ Open 6:e011144. https://doi.org/10.1136/bmjopen-2016-011144
Zubair A, Burbelo PD, Vincent LG, Iadarola MJ, Smith PD, Morgan NY (2011) Microfluidic LIPS for serum antibody detection: demonstration of a rapid test for HSV-2 infection. Biomed Microdevices. https://doi.org/10.1007/s10544-011-9575-x
Burbelo PD, Gunti S, Keller JM et al (2017) Ultrarapid measurement of diagnostic antibodies by magnetic capture of immune complexes. Sci Rep 7:3818. https://doi.org/10.1038/s41598-017-03786-7
Acknowledgements
This study was supported by the JDRF—The Leona M. and Harry B. Helmsley Charitable Trust Grant 2-SRA-2015-50-Q-R. The study was conducted within the framework of the Italian Ministry of Research’s project “Ivascomar Project, Cluster Tecnologico Nazionale Scienze della Vita ALISEI.” The Belgian Diabetes Registry is supported by the Research Foundation-Flanders (Fonds Wetenschappelijk Onderzoek-Vlaanderen) Project No. G.0868.11, the Research Council of the Vrije Universiteit Brussel Project SRP-42, the Willy Gepts Fund of Universitair Ziekenhuis Brussel Project G177/2013, and the Flemish Government Project IWT 130138.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Statement of Human and Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5).
Informed consent
Informed consent was obtained from all patients for being included in the study.
Additional information
Managed by Massimo Federici.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Liberati, D., Wyatt, R.C., Brigatti, C. et al. A novel LIPS assay for insulin autoantibodies. Acta Diabetol 55, 263–270 (2018). https://doi.org/10.1007/s00592-017-1082-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-017-1082-y