Abstract
Aims
Circulating lipopolysaccharides (LPSs), associated with both infection and inflammation, may arise from the gastrointestinal tract microbiota, and the levels may be affected by daily nutrition. We investigated whether nutrient intake affects the association of serum LPS activity with prevalent obesity, metabolic syndrome (MetS), diabetes, and coronary heart disease (CHD) and with the risk of incident CHD events.
Methods
The nutrition cohort (n = 2,452, mean age ± SD, 52.2 ± 10.1 years) of the FINRISK 1997 Study was followed up for 10 years. Information on macronutrient intake at baseline was collected from 24-h dietary recall. Serum endotoxin activities were determined by the Limulus amebocyte lysate assay.
Results
LPS activity was associated directly with the total energy intake and indirectly with carbohydrate intake in lean, healthy subjects. High LPS was significantly associated with prevalent obesity, MetS, diabetes, and CHD events, independently of established risk factors, CRP, and total energy or nutrient intake. The ORs (95 % CI) were 1.49 (1.21–1.85, p < 0.001, Q2–4 vs. Q1) for obesity, 2.56 (1.97–3.32, p < 0.001, Q2–4 vs. Q1) for MetS, 1.94 (1.06–3.52, p = 0.031, Q2–4 vs. Q1) for CHD, and 1.01 (1.00–1.01, p = 0.032, LPS unit) for diabetes. In the follow-up, high LPS was significantly associated with the risk of CHD events with a hazard ratio of 1.88 (1.13–3.12, p = 0.013, Q2–4 vs. Q1). This association was independent of baseline established risk factors, diet, obesity, MetS, and diabetes.
Conclusion
A high serum LPS activity is strongly associated with cardiometabolic disorders, which supports the role of bacterial infections and immune response in their etiology.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lipopolysaccharide (LPS), often referred to as endotoxin, is a large glycolipid that consists of lipid and polysaccharide moieties joined by a covalent bond. This important virulence factor of Gram-negative bacteria is found in the outer bacterial membrane. In humans, increased systemic levels of endotoxins promote the pro-inflammatory response of the innate immune system.
“Metabolic endotoxemia” is a twofold to threefold increase in serum LPS level, which is detectable also in apparently healthy subjects and may result in low-grade inflammation [1–3]. The long-term effects of subclinical endotoxemia are deleterious, since endotoxemia associates with the risk of incident cardiovascular disease (CVD) events [4, 5] and diabetes [6]. Endotoxemia also associates with components and presence of metabolic syndrome (MetS) [6, 7], insulin resistance, dyslipidemia, obesity, and chronic inflammation [4, 7]. LPS may arise from various sources: bacterial infections, diet, and commensal microbiota. Lifestyle, dietary habits, and the use of antimicrobial agents may affect the variety of bacterial species and the microbial load. These modulations in the composition of commensal microbiota may be important contributors to the host metabolism affecting energy homeostasis.
Human gastrointestinal tracts, including the oral cavity and the gut, are colonized by Gram-negative bacteria. For example, the adult human intestine is inhabited by 1013–1014 microorganisms [8]. In healthy conditions, intestinal alkaline phosphatase may maintain normal gut homeostasis by neutralizing LPS toxicity [9] and the intestinal epithelium defends itself from LPS translocation. Of note, fat-containing diet may promote intestinal transport of fat-soluble LPS molecules via chylomicrons [10]. In addition, it has been suggested that LPS may be absorbed by intestinal cells [11] and expression of genes involved in the barrier function in host epithelial cells may be modulated by bacteria [12].
The previous studies on humans suggest that endotoxemia may be associated with energy, fat, and carbohydrate intake, and furthermore, that postprandial endotoxin absorption is affected by the metabolic disease state. These studies are interventions with relatively small study populations, while large population-based studies with information on nutrient intake collected from dietary recalls do not exist. High energy intake composed of saturated fat or carbohydrate-rich meal may lead to acute low-grade endotoxemia [2, 13–15]. A high-fat meal has been shown to elevate circulating endotoxin levels both in healthy, lean subjects [2, 14] and in subjects with metabolic disorders, i.e., obesity, type 2 diabetes, or impaired glucose tolerance [15, 16]. Indeed, LPS appears to be a molecular link between high-fat diet, microbiota, and inflammation, which has been shown in a mouse model for the time being [3]. We investigated in a population-based nutrition cohort the association of serum LPS activity with prevalent obesity, MetS, diabetes, and coronary heart disease (CHD) and with the risk of incident CHD events, taking into account data on the individual energy and macronutrient intake registered in a dietary 24-h recall.
Materials and methods
Study population
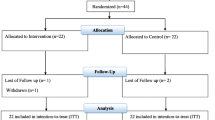
The National FINRISK 1997 Study is a population-based risk factor survey with 8,444 participants. It was conducted in five geographical areas in Finland, and the age range was 25 to 74 years [17]. The survey methods follow the WHO MONICA protocol [18]. The National FINDIET 1997 Survey (n = 2,452) is a nutrition subsample of the FINRISK 1997. The study included a self-administered questionnaire and a clinical examination with weight, height, and blood pressure measurements, and blood samples. The study was approved by the ethics committee of the National Public Health Institute, and it was conducted according to the Declaration of Helsinki. All subjects gave an informed consent.
Laboratory analysis
Subjects were asked to fast 4 h and to avoid heavier meals prior to blood sampling. The median fasting time was 5 (interquartile range 3–7) h. Lipids and γ-glutamyltransferase (GGT) measurements were taken from fresh serum samples. The rest of the serum and plasma biomarkers were determined from samples stored at −70 °C. Ultrasensitive C-reactive protein (CRP) was determined with Architect c8000 analyzer (Abbott Laboratories, Abbott Park, IL). Serum endotoxin activities were determined by a Limulus amebocyte lysate assay coupled with a chromogenic substrate (HyCult Biotechnology B.V., Uden, the Netherlands), and the interassay coefficient of variation was 9.2 % (n = 75). The laboratory analyses have been described earlier in detail [6].
Determination of risk factors and diseases
Obesity was defined as a body mass index (BMI)-based classification of adult overweight (≥25 kg/m2) and obesity (≥30 kg/m2) according to the World Health Organization [19].
The subjects were classified into those with and without MetS according to the International Diabetes Federation definition for Europids [20].
Prevalent diabetes and CVD events were defined as a doctor-diagnosed disease using the questionnaire, and the register data either as an intake of related drugs or as hospitalizations with the disease. CHD events included subjects with the history of myocardial infarction, revascularizations, or percutaneous transluminal coronary angioplasty. Additionally, history of stroke (excluding subarachnoid hemorrhage) was included in the prevalent CVD. Follow-up for incident CHD events was performed for 10 years with the use of record linkage of the FINRISK data with three data sources: (1) National Hospital Discharge Register; (2) National Causes of Death Register; and (3) National Drug Reimbursement Register. The high validity of the data on CHD events has been shown previously [21].
Blood pressure measurements have been described in detail earlier [17]. Hypertension was determined according to the criteria of the American Heart Association [22] as blood pressure ≥140 mmHg systolic or ≥90 mmHg diastolic or the use of any antihypertensive drug.
Smoking was assessed by a self-administered questionnaire. Classification was performed into three categories: (1) current smokers (who had smoked regularly for ≥1 year and still smoked or had quit smoking <6 months ago); (2) former smokers (who used to smoke regularly but had quit ≥6 months before the survey); and (3) non-smokers (who had never smoked regularly).
Information on diet was collected from the interviewed 24-h dietary recall. A picture booklet of food portions was used to estimate portion sizes [23]. The average daily intakes of energy, energy-yielding nutrients, and fiber were calculated by the national food composition database Fineli®, using an in-house software [24]. We used standard energy densities in the analysis: 37 kJ/g for fat, 17 kJ/g for protein and carbohydrates, and 8 kJ/g for fiber (http://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=OJ:L:2011:304:0018:0063:EN:PDF).
Statistical analysis
The statistical significance of differences between the subjects with and without cardiometabolic disorders was tested with t test or chi-square test. The values with skewed distribution (serum triglyceride, GGT, and CRP) were logarithmically transformed before comparisons. Smoking habit was used in the categories never, former, and current smokers. Subjects were excluded from the study if the reported total energy intakes were less (n = 17) or greater (n = 0) than 3xSD from the mean energy intake of the population [25]. Association between LPS and total energy and nutrient intake was analyzed by linear regression model, first unadjusted, followed by a multivariate model including age, sex, education years, BMI, current smoking, and serum GGT, CRP, and cholesterol concentrations, and the use of hypertension medication. The differences in LPS concentrations between lean (BMI < 25 kg/m2), overweight (BMI ≥ 25 kg/m2), and obese (≥30 kg/m2) subjects were determined by the one-way analysis of variance (ANOVA). The association of prevalent cardiometabolic disorders with the LPS activity was analyzed using a logistic regression model. In the models where the dependent variables were obesity, MetS, diabetes, or CHD, the covariates included age, sex, education years, current smoking, hypertension (except the MetS model), cholesterol and CRP concentrations, and energy intake. The logistic regression models were repeated adjusting for protein, fat, and fiber intake instead of total energy. Those with prevalent CVD (n = 151) were excluded from the prospective analyses. The possible effect of hypertension medication to the relation between LPS and total energy and nutrient intake was tested by interaction terms in all regression models; the associations were not statistically significant.
The association of incident CHD events with the LPS activity was analyzed using seven different Cox regression models. All models were adjusted for age, sex, years of education, current smoking, hypertension (except the MetS models), cholesterol, and CRP concentrations. Model 2 was further adjusted for MetS, model 3 for MetS and energy (418.7 kJ or 100 kcal), model 4 for obesity, model 5 for obesity and energy, and finally Model 6 for diabetes and model 7 for diabetes and energy.
The statistical analyses were executed with the IBM SPSS Statistics 21 Statistical Package for Social Sciences.
Results
Characteristics of the subjects with or without cardiometabolic disorders are summarized in Table 1. In the FINRISK 1997 nutrition cohort at baseline, 65.8 % were overweight or obese, 30.1 % had MetS, 7.1 % diabetes, and 6.2 % CHD. Most of the cardiometabolic risk factors differed significantly between the counterparts. Males were more frequently obese, while females had more MetS, diabetes, or CHD. In total, 481 of the study subjects were using antihypertensive medication. Online Resource 1 summarizes the information on macronutrient intake from the 24-h dietary recall.
LPS activity did not correlate significantly with total energy, carbohydrate, or fat intake in univariate linear regression models. However, in a multivariate model, LPS activity was associated directly with the total energy intake with unstandardized regression coefficients/418 kJ (100 kcal) (SE) 0.90 (0.43, p = 0.037) and indirectly with the carbohydrates available, −0.055 (0.02, p = 0.018) (Table 2). The association of LPS and energy or carbohydrate intake arose only from lean, healthy subjects; no significant associations were observed in subjects with CHD, obesity, MetS, or DM (Table 2). Corresponding results were also obtained when cardiometabolically healthy subjects (n = 763) were compared to those with at least one of the listed disorders.
The mean (SD) endotoxin activity was higher in the subjects with prevalent cardiometabolic disorder compared to subjects without: 68.5 (39.8) versus 54.2 (29.4) pg/ml, (p < 0.001) for obesity, 79.6 (44.8) versus 56.6 (31.0) pg/ml (p < 0.001) for MetS, and 68.9 (39.7) versus 63.2 (37.0) pg/ml (p = 0.05) for diabetes (Fig. 1). The difference between those with and without prevalent CHD, 68.0 (37.2) versus 63.4 (37.3) pg/ml, was not significant (p = 0.243). In addition, LPS increased with increasing BMI. The mean activities were 54.2 (29.4), 65.8 (37.5), and 73.7 (37.3) pg/ml, (p < 0.001) in lean, overweight, and obese subjects, respectively.
Serum endotoxin activities in the cardiometabolic disorders. LPS activity (pg/ml) was determined by Limulus amebocyte lysate assay. Mean endotoxin activities with 95 % CI are shown. Subjects without and with a cardiometabolic disorder are indicated by white and gray bars, respectively. The statistical significance of differences in endotoxin activities was tested with t test; *p ≤ 0.05, **p ≤ 0.01, ***p ≤ 0.001
In logistic regression models, high LPS was significantly associated with prevalent obesity, MetS, diabetes, and CHD. These associations were independent of cardiometabolic risk factors, CRP, and energy-yielding nutrients and fiber, or total energy intake. In the second–fourth quartiles (Q2–4) compared to the first quartile (Q1) of the LPS activity when adjusted for total energy, the ORs (95 % CI) were 1.49 (1.21–1.85, p < 0.001) for obesity, 2.56 (1.97–3.32, p < 0.001) for MetS, and 1.94 (1.06–3.52, p = 0.031) for CHD. The OR for diabetes was 1.01 (1.00–1.01, p = 0.032) per pg/ml increase in the LPS activity. The regression models are presented in Table 3. The ORs did not change notably when, instead of total energy intake, the models were adjusted for intake of macronutrients, protein, fat, and fiber (data not shown).
During the follow-up of 10 years, among subjects with no history of CVD at baseline (n = 2,301) altogether 137 incident CHD events appeared. In the multivariate analysis, high LPS was significantly associated with CHD events with a hazard ratio 1.90 (1.15–3.16, p = 0.013) (Table 4). The hazard ratio was not substantially changed when the model was adjusted for total energy intake (Fig. 2) or macronutrients (data not shown), or further, for prevalent obesity, MetS, or diabetes (Table 4).
Cumulative hazard for incident CHD events. The cumulative hazard in LPS quartiles (Q1 in gray vs. Q2–4 in black) was analyzed by Cox regression model adjusted for age, sex, education years, current smoking, cholesterol and CRP concentrations, hypertension, and energy intake in the follow-up of 10 years. The CHD events included subjects with myocardial infarction, coronary death, coronary bypass surgery, or percutaneous transluminal coronary angioplasty
Discussion
This large population-based study shows that endotoxemia is associated with prevalent cardiometabolic disorders, i.e., obesity, MetS, diabetes, and CHD independently of established cardiometabolic risk factors and factors known to affect serum endotoxin activity (age, sex, cholesterol, BMI, CRP). Interestingly, we showed that the association is also independent of energy or macronutrients. In addition, high LPS activity is associated with an increased risk of incident CHD events independently of baseline cardiometabolic disorders, risk factors, or macronutrients. Previously, we have reported in the population-based FINRISK 1997 Study that endotoxemia is associated with increased risk for incident diabetes [6]. In concordance, the present nutrition subsample of the FINRISK 1997 Study showed also a direct association between high LPS levels and incident diabetes independently of nutrient intake.
In mice, feeding studies have shown an influence of the diet on circulating endotoxin levels [3]. In mice grown in germ-free environment, endotoxemia has been associated with the onset of insulin resistance, weight gain, and low-grade inflammation following high-fat diet. In humans, similar observations have been reported with relatively small intervention studies carried out in controlled environment. A Western-style high-fat diet seems to result in gut dysbiosis, an altered composition of the microbiota, which may disrupt the intestinal barrier leading to translocation of LPS into circulation via increased gut permeability or secretion with chylomicrons [3, 26]. Present lifestyle including a high-fat and energy-rich diet induces endotoxemia and furthermore low-grade inflammation compared with no meal or a meal rich in fruit and fiber [2, 14]. Both glucose intake and cream intake have been shown to induce inflammation and insulin resistance, while only intake of cream elevated plasma LPS concentrations [27]. In contrast, the intake of an equivalent amount of carbohydrate as orange juice caused neither inflammation nor endotoxemia in the same study. Indeed, the orange juice seems to neutralize the pro-inflammatory effect of a high-fat, high-carbohydrate meal and prevent endotoxemia and insulin resistance [28]. These observations suggest the concept of nutrition as a potential modulator of postprandial endotoxemia and inflammation. Large studies with data on nutrition, metabolic state, and endotoxemia are scarce. Therefore, in the present study, we focused to investigate the association of LPS with cardiometabolic disorders, taking into account data on the energy and macronutrient intake.
In the present study, we found that endotoxemia associated directly with daily energy but indirectly with carbohydrate intake. This is in agreement with previous studies [13], but deviating from the feeding trials [2, 14, 29], since no association was found between endotoxemia and fat intake either in univariate or in multivariate analyses. These associations were clearly dependent on the metabolic conditions, since in any of the cardiometabolic disorders studied separately no association between endotoxemia and energy or carbohydrate intake was observed. Harte et al. [15] showed that subjects with compromised metabolic state had a stronger acute endotoxemia response to high-fat diet than metabolically healthy subjects. A very recent study showed no significant impact of acute fat intake to endotoxin activity in healthy subjects or patients with type 1 diabetes, suggesting that metabolic endotoxemia may be more substantive in patients with chronic metabolic disorders [30]. However, the design in the feeding trials compared to the present one is totally different, because we have merely measured the fasting period endotoxemia and tried to avoid the effect of postprandial status. Despite of the results, the intake of energy or macronutrients did not affect the association of high LPS activity with the cardiometabolic disorders. The reported energy and macronutrients intake values between the cardiometabolic groups had relatively minor variation, although there were some statistically significant differences. The significant disparity might be due to the dietary counseling for patients diagnosed, e.g., for diabetes.
The FINRISK 1997 is an extensive study with a prospective design, well-determined risk factor data for multivariate adjustments, and long follow-up time. Yet, as a limitation, the information on macronutrient intake was collected from the 24-h dietary recall, which cannot provide information on long-term diet and may be affected by causal diet variations during the registration period. To reduce misclassification, we excluded subjects if the reported total energy intakes were less or greater than 3xSD from the mean energy intake of the population [25].
The mean LPS activity of the study population (63.6 EU/ml) was on the same level as found in Finnish healthy blood donors (35.9 EU/ml) [31] and the middle-aged subjects (122.8 EU/ml) [4]. Again, mean LPS concentration of 6.7 pg/ml has been reported in the healthy elderly [32] and 850 pg/ml in patients with Gram-negative sepsis [33]. It is problematic to compare results of the endotoxin measurements between different studies due to the variety of units reported, assay kits, standardizations, and even among the assay lots available. The origin of serum endotoxin activity remains unknown, since the limulus assay is not specific to any bacterial species, and endotoxin activity diverges even between different bacterial clones. Generally, endotoxins from anaerobic bacteria, commonly found in the gut and oral cavity, are more reactive in the limulus assay than, for example, E. coli [34], which in most assay kits is used as a standard. Therefore, measuring endotoxemia with the limulus assay mirrors the exposure only to certain, but unknown, mixture of LPS.
Although metabolic endotoxemia probably plays a significant role in circulating LPS levels, the most likely sources of endotoxins are chronic infections by Gram-negative microbes, such as periodontal pathogens. Periodontitis is a common chronic oral infection of multiple, mostly Gram-negative anaerobic bacterial species, such as Tannerella forsythia, Aggregatibacter actinomycetemcomitans, and Porphyromonas gingivalis. It affects, especially the middle-aged and elderly, and gives rise to bacteremia and endotoxemia, which are more frequent than previously thought. LPS may travel to the bloodstream through inflamed periodontal tissue during daily routines, e.g., tooth brushing, or via saliva to gastrointestinal tract [35, 36]. Through binding to pathogen-sensing system, LPS induces release of a large number of inflammatory cytokines, which play an important role in metabolic processes. Clinical periodontitis itself has been associated with incident cardiovascular disease events and type 2 diabetes [37, 38]. Similarly as in the most studies exploring the relation between endotoxemia and diet, in the present study, the periodontal status of the subjects was not examined.
Altogether, our earlier studies [4, 6, 7] and the present data show that high serum LPS activity is strongly associated with cardiometabolic disorders and the risk of future CHD events. In addition to metabolic endotoxemia, the results support the role of bacterial infections and immune response in the etiology of cardiometabolic diseases. Although energy intake was correlated with endotoxemia in healthy subjects, the overall associations were independent of macronutrient intake.
References
Neves AL, Coelho J, Couto L, Leite-Moreira A, Roncon-Albuquerque R Jr (2013) Metabolic endotoxemia: a molecular link between obesity and cardiovascular risk. J Mol Endocrinol 51:R51–R64
Erridge C, Attina T, Spickett CM, Webb DJ (2007) A high-fat meal induces low-grade endotoxemia: evidence of a novel mechanism of postprandial inflammation. Am J Clin Nutr 86:1286–1292
Cani PD, Amar J, Iglesias MA, Poggi M, Knauf C, Bastelica D, Neyrinck AM, Fava F, Tuohy KM, Chabo C, Waget A, Delmee E, Cousin B, Sulpice T, Chamontin B, Ferrieres J, Tanti JF, Gibson GR, Casteilla L, Delzenne NM, Alessi MC, Burcelin R (2007) Metabolic endotoxemia initiates obesity and insulin resistance. Diabetes 56:1761–1772
Pussinen PJ, Tuomisto K, Jousilahti P, Havulinna AS, Sundvall J, Salomaa V (2007) Endotoxemia, immune response to periodontal pathogens, and systemic inflammation associate with incident cardiovascular disease events. Arterioscler Thromb Vasc Biol 27:1433–1439
Wiedermann CJ, Kiechl S, Dunzendorfer S, Schratzberger P, Egger G, Oberhollenzer F, Willeit J (1999) Association of endotoxemia with carotid atherosclerosis and cardiovascular disease: prospective results from the Bruneck Study. J Am Coll Cardiol 34:1975–1981
Pussinen PJ, Havulinna AS, Lehto M, Sundvall J, Salomaa V (2011) Endotoxemia is associated with an increased risk of incident diabetes. Diabetes Care 34:392–397
Lassenius MI, Pietilainen KH, Kaartinen K, Pussinen PJ, Syrjanen J, Forsblom C, Porsti I, Rissanen A, Kaprio J, Mustonen J, Groop PH, Lehto M, FinnDiane Study Group (2011) Bacterial endotoxin activity in human serum is associated with dyslipidemia, insulin resistance, obesity, and chronic inflammation. Diabetes Care 34:1809–1815
Backhed F, Ley RE, Sonnenburg JL, Peterson DA, Gordon JI (2005) Host-bacterial mutualism in the human intestine. Science 307:1915–1920
Kelly CJ, Colgan SP, Frank DN (2012) Of microbes and meals: the health consequences of dietary endotoxemia. Nutr Clin Pract 27:215–225
Ghoshal S, Witta J, Zhong J, de Villiers W, Eckhardt E (2009) Chylomicrons promote intestinal absorption of lipopolysaccharides. J Lipid Res 50:90–97
Hathaway LJ, Kraehenbuhl JP (2000) The role of M cells in mucosal immunity. Cell Mol Life Sci 57:323–332
Hooper LV, Gordon JI (2001) Commensal host-bacterial relationships in the gut. Science 292:1115–1118
Amar J, Burcelin R, Ruidavets JB, Cani PD, Fauvel J, Alessi MC, Chamontin B, Ferrieres J (2008) Energy intake is associated with endotoxemia in apparently healthy men. Am J Clin Nutr 87:1219–1223
Ghanim H, Abuaysheh S, Sia CL, Korzeniewski K, Chaudhuri A, Fernandez-Real JM, Dandona P (2009) Increase in plasma endotoxin concentrations and the expression of Toll-like receptors and suppressor of cytokine signaling-3 in mononuclear cells after a high-fat, high-carbohydrate meal: implications for insulin resistance. Diabetes Care 32:2281–2287
Harte AL, Varma MC, Tripathi G, McGee KC, Al-Daghri NM, Al-Attas OS, Sabico S, O’Hare JP, Ceriello A, Saravanan P, Kumar S, McTernan PG (2012) High fat intake leads to acute postprandial exposure to circulating endotoxin in type 2 diabetic subjects. Diabetes Care 35:375–382
Clemente-Postigo M, Queipo-Ortuno MI, Murri M, Boto-Ordonez M, Perez-Martinez P, Andres-Lacueva C, Cardona F, Tinahones FJ (2012) Endotoxin increase after fat overload is related to postprandial hypertriglyceridemia in morbidly obese patients. J Lipid Res 53:973–978
Vartiainen E, Laatikainen T, Peltonen M, Juolevi A, Mannisto S, Sundvall J, Jousilahti P, Salomaa V, Valsta L, Puska P (2010) Thirty-five-year trends in cardiovascular risk factors in Finland. Int J Epidemiol 39:504–518
WHO (1988) The World Health Organization MONICA Project (monitoring trends and determinants in cardiovascular disease): a major international collaboration. WHO MONICA Project Principal Investigators. J Clin Epidemiol 41:105–114
World Health Organization 2 (2004) Obesity: prevention and managing the global epidemic. Report of a WHO Consultation. WHO Technical Report Series no. 894. WHO, Geneva
Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, Fruchart JC, James WP, Loria CM, Smith SC Jr, International Diabetes Federation Task Force on Epidemiology and Prevention, National Heart, Lung, and Blood Institute, American Heart Association, World Heart Federation, International Atherosclerosis Society, International Association for the Study of Obesity (2009) Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 120:1640–1645
Pajunen P, Koukkunen H, Ketonen M, Jerkkola T, Immonen-Raiha P, Karja-Koskenkari P, Mahonen M, Niemela M, Kuulasmaa K, Palomaki P, Mustonen J, Lehtonen A, Arstila M, Vuorenmaa T, Lehto S, Miettinen H, Torppa J, Tuomilehto J, Kesaniemi YA, Pyorala K, Salomaa V (2005) The validity of the finnish hospital discharge register and causes of death register data on coronary heart disease. Eur J Cardiovasc Prev Rehabil 12:132–137
Perloff D, Grim C, Flack J, Frohlich ED, Hill M, McDonald M, Morgenstern BZ (1993) Human blood pressure determination by sphygmomanometry. Circulation 88:2460–2470
Pietinen P, Hartman AM, Haapa E, Rasanen L, Haapakoski J, Palmgren J, Albanes D, Virtamo J, Huttunen JK (1988) Reproducibility and validity of dietary assessment instruments. I. A self-administered food use questionnaire with a portion size picture booklet. Am J Epidemiol 128:655–666
Reinivuo H, Hirvonen T, Ovaskainen ML, Korhonen T, Valsta LM (2010) Dietary survey methodology of FINDIET 2007 with a risk assessment perspective. Public Health Nutr 13:915–919
Missmer SA, Smith-Warner SA, Spiegelman D, Yaun SS, Adami HO, Beeson WL, van den Brandt PA, Fraser GE, Freudenheim JL, Goldbohm RA, Graham S, Kushi LH, Miller AB, Potter JD, Rohan TE, Speizer FE, Toniolo P, Willett WC, Wolk A, Zeleniuch-Jacquotte A, Hunter DJ (2002) Meat and dairy food consumption and breast cancer: a pooled analysis of cohort studies. Int J Epidemiol 31:78–85
Musso G, Gambino R, Cassader M (2011) Interactions between gut microbiota and host metabolism predisposing to obesity and diabetes. Annu Rev Med 62:361–380
Deopurkar R, Ghanim H, Friedman J, Abuaysheh S, Sia CL, Mohanty P, Viswanathan P, Chaudhuri A, Dandona P (2010) Differential effects of cream, glucose, and orange juice on inflammation, endotoxin, and the expression of Toll-like receptor-4 and suppressor of cytokine signaling-3. Diabetes Care 33:991–997
Ghanim H, Sia CL, Upadhyay M, Korzeniewski K, Viswanathan P, Abuaysheh S, Mohanty P, Dandona P (2010) Orange juice neutralizes the proinflammatory effect of a high-fat, high-carbohydrate meal and prevents endotoxin increase and toll-like receptor expression. Am J Clin Nutr 91:940–949
Pendyala S, Walker JM, Holt PR (2012) A high-fat diet is associated with endotoxemia that originates from the gut. Gastroenterology 142(1100–1101):e2
Lassenius MI, Makinen VP, Fogarty CL, Peraneva L, Jauhiainen M, Pussinen PJ, Taskinen MR, Kirveskari J, Vaarala O, Nieminen JK, Horkko S, Kangas AJ, Soininen P, Ala-Korpela M, Gordin D, Ahola AJ, Forsblom C, Groop PH, Lehto M (2014) Patients with type 1 diabetes show signs of vascular dysfunction in response to multiple high-fat meals. Nutr Metab (Lond) 11:28-7075-11-28. eCollection 2014
Pradhan-Palikhe P, Vikatmaa P, Lajunen T, Palikhe A, Lepantalo M, Tervahartiala T, Salo T, Saikku P, Leinonen M, Pussinen PJ, Sorsa T (2010) Elevated MMP-8 and decreased myeloperoxidase concentrations associate significantly with the risk for peripheral atherosclerosis disease and abdominal aortic aneurysm. Scand J Immunol 72:150–157
Goto T, Eden S, Nordenstam G, Sundh V, Svanborg-Eden C, Mattsby-Baltzer I (1994) Endotoxin levels in sera of elderly individuals. Clin Diagn Lab Immunol 1:684–688
Pearson FC, Dubczak J, Weary M, Bruszer G, Donohue G (1985) Detection of endotoxin in the plasma of patients with gram-negative bacterial sepsis by the Limulus amoebocyte lysate assay. J Clin Microbiol 21:865–868
Wachtel RE, Tsuji K (1977) Comparison of limulus amebocyte lysates and correlation with the United States Pharmacopeial pyrogen test. Appl Environ Microbiol 33:1265–1269
Kinane DF, Riggio MP, Walker KF, MacKenzie D, Shearer B (2005) Bacteraemia following periodontal procedures. J Clin Periodontol 32:708–713
Lappin DF, Sherrabeh S, Erridge C (2011) Stimulants of Toll-like receptors 2 and 4 are elevated in saliva of periodontitis patients compared with healthy subjects. J Clin Periodontol 38:318–325
DeStefano F, Anda RF, Kahn HS, Williamson DF, Russell CM (1993) Dental disease and risk of coronary heart disease and mortality. BMJ 306:688–691
Demmer RT, Jacobs DR Jr, Desvarieux M (2008) Periodontal disease and incident type 2 diabetes: results from the First National Health and Nutrition Examination Survey and its epidemiologic follow-up study. Diabetes Care 31:1373–1379
Acknowledgments
This work was supported by the grants from the Academy of Finland (1266053 to P.J.P., 136895 and 263836 to S.M.), the Sigrid Juselius Foundation (P.J.P), the Aarne Koskelo Foundation (K.A.E.K), Folkhälsan Institute of Genetics (M.L.), the Finnish Dental Society Apollonia (K.A.E.K), and the Finnish Foundation for Cardiovascular Research (V.S.).
Conflict of interest
Elisa Kallio, Katja Hätönen, Markku Lehto, Veikko Salomaa, Satu Männistö, and Pirkko Pussinen declare that they have no conflict of interest.
Human and animal rights disclosure
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975.
Informed consent disclosure
Informed consent was obtained from all patients for being included in the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Managed by Massimo Federici.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kallio, K.A.E., Hätönen, K.A., Lehto, M. et al. Endotoxemia, nutrition, and cardiometabolic disorders. Acta Diabetol 52, 395–404 (2015). https://doi.org/10.1007/s00592-014-0662-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-014-0662-3