Abstract
Vitamin D (Vit D) deficiency may be linked to the development of obesity-associated complications such as insulin resistance and type 2 diabetes. We therefore evaluated the relationship of Vit D serum concentrations with metabolic parameters and type 2 diabetes in middle-aged Caucasian men and women. One thousand six hundred and thirty-one Caucasians (832 males, 58.8 ± 9.7 years; 799 females, 59.7 ± 10.7 years) were evaluated in a cross-sectional study. Vit D status was assessed by measuring the serum concentration of 25-hydroxyvitamin D3 [25(OH)D3]. Type 2 diabetes prevalence was ascertained by medical history, fasting plasma glucose concentrations, oral glucose tolerance testing and/or glycosylated hemoglobin. Men displayed higher crude or seasonally adjusted 25(OH)D3 serum concentrations than women (24.64 ± 10.98 vs. 22.88 ± 11.6 ng/ml; P < 0.001). Strong associations between body mass index (BMI) and 25(OH)D3 were observed in both genders (P < 0.001). Seasonally adjusted levels of 25(OH)D3 revealed stronger associations with type 2 diabetes in women than men (P < 0.001). However, adjustment for BMI and other confounding variables revealed an independent inverse association of 25(OH)D3 with diabetes only in women (P < 0.001), whereas the association was abrogated in men. Using a 15 ng/ml 25(OH)D3 cutoff for binary comparison, adjusted odds ratios for having newly diagnosed or known type 2 diabetes more than doubled (2.95 [95 % CI 1.37–4.89] and 3.26 [1.59–6.68], respectively), in women below the cutoff. We conclude that in women, but not in men, low 25(OH)D3 serum levels are independently associated with type 2 diabetes. These findings suggest sex-specific effects of Vit D in the pathogenesis of type 2 diabetes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Serum vitamin D (Vit D) concentrations depend on biosynthesis in response to UVB exposure and Vit D dietary intake. Recently, a potentially prominent role of Vit D has emerged in the development of common diseases such as cancer, cardiovascular disease and insulin resistance (IR) [1] besides its long-recognized involvement in calcium and bone metabolism. In the general population, low levels of Vit D (defined as a serum 25(OH)D3 level <20 ng/ml) [2] were associated with the metabolic syndrome (MetS), prediabetes, impaired fasting glucose and impaired glucose tolerance [3–6]. These associations were not only found in cross-sectional studies, but also in prospective settings [7, 8]. Similarly, a decreased risk of type 2 diabetes, cardiovascular disease and MetS was reported in subjects with high serum concentrations of Vit D [9].
However, not all studies confirmed the relationship of Vit D status with fasting glucose, IR or type 2 diabetes [10, 11]. Thus, evidence so far available on the role of Vit D in the pathogenesis of type 2 diabetes is inconclusive. In addition, the MetS and type 2 diabetes share common risk factors with low Vit D including physical inactivity with decreased sunlight exposure and obesity making it difficult to determine causality. Nonetheless, Vit D supplementation suggested a beneficial effect on adipose tissue distribution with a reduction in visceral adipose tissue [12], and a meta-analysis demonstrated a strong link between Vit D status and incident type 2 diabetes [13], arguing for a role of Vit D in the pathophysiology of obesity-related complications rather than obesity itself.
The roles of Vit D may differ between men and women [14], but sex-specific influences have been incompletely assessed in the setting of newly diagnosed or known type 2 diabetes. We therefore performed a detailed analysis of serum 25(OH)D3 concentrations and glucometabolic parameters in a well-characterized population of middle-aged Caucasian men and women.
Materials and methods
Study population
The study was conducted in participants of a health-screening program [15]. From a total of 838 initially screened male subjects, four males were excluded because of systemic autoimmune diseases taking systemic steroids (rheumatoid arthritis, systemic lupus erythematodes and autoimmune hepatitis). Two men were diagnosed with pancreatic or hematological neoplasm, and these were also excluded. Six of 805 screened females were excluded because of systemic autoimmune disease. Thus, data from 832 Caucasian males (aged between 33 and 87 years) and 799 females (31–88 years) were included in the analysis. The study was approved by the local ethics committee, and informed consent was obtained from all participants.
Following an overnight fast, venous blood was drawn. A detailed medical history, including life style questionnaires, was obtained. Physical activity was assessed by the international physical activities questionnaire (IPAQ) [16] and was available in 1,403 study subjects. A standard physical examination was performed that included blood pressure readings and body mass index (BMI) and waist/hip ratio measurements. Hypertension was defined as blood pressure ≥135/85 mmHg or current antihypertensive treatment. A full blood count was obtained in all subjects by standard laboratory methods. Blood was centrifuged, and plasma was analyzed for triglycerides, cholesterol, high density and low density lipoprotein cholesterol and C-reactive protein (CRP).
Assessment of type 2 diabetes and glucose metabolism
Plasma glucose and insulin were determined as described [17]. HbA1c was measured by HPLC using Adamts H-8160 (Menarini, Florence, Italy). An oral glucose tolerance test (OGTT) was performed with 75 g of glucose in 300 ml of water according to international guidelines. The homeostasis model assessment [HOMA-IR; fasting insulin (µU/l) × fasting glucose (mmol/l)/22.5] was used to assess IR. HOMA-B [20 × fasting insulin (µU/l)/[fasting glucose (mmol/l) − 3.5]] was used for estimating beta-cell function. Type 2 diabetes was classified as use of glucose-lowering medication, HbA1C ≥6.5 % (48 mmol/mol) [18], 120 min OGTT glucose levels ≥11.1 mmol/l or fasting glucose ≥7.0 mmol/l.
Assessment of vitamin D status
We determined 25(OH)D3 by the electrochemiluminescence-based Cobase 411 analyserTM using the respective ElecsysTM reagents (Roche Diagnostics GmbH, Mannheim, Germany). The laboratory performed regular quality control measurements, including a pooled serum sample analyses to monitor precision and identify possible laboratory shifts over time, as well as testing duplicates in different batches. The coefficient of variation was <6 % for 25(OH)D3 for between-batches analyses. All analyses were conducted in a blinded fashion.
Statistical analysis
For all analyses, Statistica 7.0 or STATA 8.0 software packages were used. Data are presented as mean ± SD, unless otherwise indicated. ANOVA was used for comparison of continuous variables. Logarithmic transformations were used, if the equal variance and normality assumptions of ANOVA were rejected. We adjusted measurements, by multiple regressions, for concomitant effects of age, BMI, seasonal variation or other variables as indicated. Seasonal variation was coded by 1, 2, 3 and 4 for the first, second, fourth and third quarters. The proportion of inter-individual variability of 25(OH)D3 levels explained by seasonal variation was ascertained using the R 2 value of the regression analysis. Smoking habits were coded as 0 and 1 for never smoking and past or current smoking, respectively. In addition, current smoking habits were coded as 0, 1 or 2 for nonsmoking, <20 cigarettes/day or ≥20 cigarettes/day, respectively. Physical activity was coded as 0, 1 or 2 for minimal, intermediate or extensive physical activity according to the IPAQ guidelines as described [19]. The χ 2 test was used to calculate rates and proportions as appropriate. Regression analysis adjusted for seasonal variation was used to determine sex-specific associations of 25(OH)D3 with variables. Logistic regression analysis was used to ascertain the variables predicting the presence of known or newly diagnosed type 2 diabetes. As this is a cross-sectional study, the dependent variable in the logistic regression equation is the log odds of having known or newly diagnosed type 2 diabetes at the time of examination. To identify the serum 25(OH)D3 level for binary classification, we used nonparametric receiver operating characteristic (ROC) analysis. Thus, the true positive and false positive rates were plotted for 25(OH)D3 levels, and the point showing the largest vertical distance to the diagonal was selected as binary classifier. Throughout, a two-tailed P value <0.05 was considered statistically significant.
Results
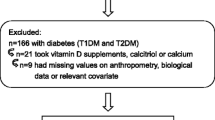
A total of 1,631 subjects with a mean age of 59.3 ± 6.3 years were enrolled. Ninety-three patients (13 males and 80 females) with current Vit D supplementation showing significantly higher 25(OH)D3 levels than subjects without Vit D supplementation were excluded (data not shown). Thus, data from 1,538 subjects, 819 males and 719 females, were included in the final analysis.
As seasonal variation in sun exposure throughout the year may result in changes of 25(OH)D3 concentrations, we assessed serum concentrations in men and women according to the time of examination. Seasonal distribution showed a similar pattern in men and women (Fig. 1); in that, the highest or lowest values were observed in the third or first quarter, respectively (P < 0.001). However, the proportion of the inter-individual variability explained by seasonal variation was higher in men than in women (8 vs. 3 %, P = 0.016).
Previously diagnosed type 2 diabetes was present in 50 (6.9 %) women and 75 (9.1 %) men, while type 2 diabetes was newly diagnosed in 53 (7.3 %) women and 67 (8.1 %) men (Table 1). Average levels of BMI, waist, waist/hip ratio, fasting glucose and triglycerides (crude or adjusted for age, BMI and seasonal quarters) were lower in women, while average adjusted levels of cholesterol and HDL cholesterol were higher. Serum levels of 25(OH)D3, crude or adjusted for seasonal quarters, age and BMI, were higher in men than in women (P < 0.001).
Strong inverse associations of seasonally adjusted 25(OH)D3 with BMI, waist/hip ratio, triglycerides and direct associations with the extent of physical activity and HDL cholesterol were observed in both genders. Strong inverse associations were also noted with systolic blood pressure, hypertension, type 2 diabetes, plasma insulin, HOMA-IR and HOMA-B in females, while no or only modest associations were observed in men (Table 2).
Type 2 diabetes was associated with older age, greater BMI and waist/hip ratio, a higher prevalence of hypertension and lower levels of HDL cholesterol in both sexes (all P < 0.001), while an association with higher triglycerides was noted only in women. Physical activity scores were moderately associated in men (P = 0.042), but strongly in women (P < 0.001). Furthermore, type 2 diabetes was associated with increased proportions of current nonsmokers in men (P = 0.037) and women (P = 0.004).
In the entire study population, logistic regression adjusted for seasonal variability revealed that 25(OH)D3 status predicted type 2 diabetes (OR 0.96 [95 % CI 0.93–0.98]). After adjustment for sex, BMI, hypertension, current smoking and HDL cholesterol, 25(OH)D3 status remained a predictor (P = 0.027, OR 0.98 [95 % CI 0.95–0.98]).
Sex-specific analysis indicated that the significant effect was only carried by the female population. In men, seasonally adjusted 25(OH)D3 status marginally predicted type 2 diabetes (P = 0.045, OR 0.98 [95 % CI 0.96–1.00]. After additional adjustment for age and BMI and further adjustment for hypertension, current smoking and HDL cholesterol, the P values increased to 0.302 and 0.516 (OR 0.99 [95 % CI 0.97–1.01]), respectively. In contrast, in women, the predictive value of 25(OH)D3 was highly significant in the seasonally adjusted model (P < 0.001) and significance was maintained in the fully adjusted model (P = 0.003, OR 0.96 [95 % CI 0.93–0.98], or 0.59 [95 % CI 0.43–0.82]) per ng/ml or SD increase in 25(OH)D3.
ROC analysis suggested that a 25(OH)D3 concentration of 15 ng/ml provided the optimal compromise between sensitivity and specificity for type 2 diabetes in the entire and the female population. Using this value, rates for sensitivity, specificity and correct classification were 34, 79 and 72 %, respectively, in the whole population. In females, the respective values were 53, 78 and 74 %. However, using 25(OH)D3 values between 12.5 and 22.5 ng/ml, the ROC area was 0.505 [95 % CI 0.023] in men. Hence, a binary classifier could not be identified. When used in unadjusted logistic regression, comparisons of the odds of overall, newly diagnosed or known type 2 diabetes in all subjects with 25(OH)D3 <15 ng/ml and the odds in all subjects with 25(OH)D3 ≥15 ng/ml were significant (all P < 0.002). However, these comparisons remained significant only for overall type 2 diabetes in models adjusted for seasonal variation, age, BMI, smoking habits, hypertension and HDL cholesterol (Table 3). In contrast, fully adjusted models for overall, newly diagnosed or known type 2 diabetes revealed significant odds ratios in women (Table 4). Furthermore, after additional adjustment for physical activity (available in 652 women), the odds ratios (95 % CIs) of binary comparisons for newly diagnosed and known type 2 diabetes were 2.34 (1.16–4.69) and 3.57 (1.66–7.68), respectively.
As 80 women and 13 men were on Vit D supplementation and these had significantly higher 25(OH)D3 serum concentrations, we evaluated the rate of type 2 diabetes in these subjects and found that among 80 women, six (7.5 %) had newly diagnosed and seven (8.8 %) known type 2 diabetes. The rates in the 719 women not using Vit D supplementation were similar [53 (7.4 %) and 50 (7 %), respectively]. Likewise, seventeen women were on hormone replacement therapy, and the results of calculations were not different when these were excluded.
To gain some insight into the potential mechanism underlying the association between Vit D and type 2 diabetes, we studied associations of 25(OH)D3 serum levels with indices of IR and/or beta-cell function in women without type 2 diabetes. Analyses adjusted for seasonal variation, age and BMI showed borderline significant associations with both HOMA-IR (P = 0.085) and HOMA-B (P = 0.075).
Conclusions
In this cross-sectional study, we performed a detailed analysis of the association of serum 25(OH)D3 concentrations with features of the IR syndrome and, in particular, with markers of impaired glucose metabolism including fasting glucose, OGTT and HbA1c. We found that low Vit D, defined as a serum 25(OH)D3 concentration <15 ng/ml, was independently linked to newly diagnosed and known type 2 diabetes in women.
Traditionally, Vit D has been almost exclusively appreciated for its prominent role in bone health. Recently, nonclassical roles of Vit D have received attention among which its involvement in the development of cancer and IR are the most important. The assumption that Vit D action impacts on multiple diseases is further supported by the fact that the key Vit D metabolizing enzymes CYP27B1 and CYP24A1 and also Vit D receptors (VDR) are nearly ubiquitously expressed, thereby providing indirect evidence of an autocrine Vit D system in many tissues including adipose tissue, endothelium, colonocytes and also beta-cells [20–23]. Gender-specific expressions of VDR, CYP27B1 and CYP24A1 have been shown previously in human colonocytes of cancer lesions [24]; however, to our knowledge, no data are available on gender-specific expression in these key tissues of IR.
The association of Vit D with obesity and its sequelae such as type 2 diabetes has been extensively investigated during the last decade with conflicting results. These data provide strong evidence that low Vit D does not increase BMI but rather that it follows the rise in BMI. At the same time, evidence that low Vit D is linked to type 2 diabetes has been further strengthened making it likely that Vit D may have a role in the pathogenesis of obesity-associated complications rather than obesity itself. Our data showing that 25(OH)D3 serum concentrations <15 ng/ml are associated with type 2 diabetes after adjusting for BMI and other potential confounders support this concept.
Importantly, the independent association between low Vit D and type 2 diabetes was observed in women, but not in men. Even more, we also demonstrated that the effect of Vit D on type 2 diabetes observed in the analysis of the whole cohort is entirely carried by the association in women. Recently, Gagnon et al. [25] have prospectively evaluated the risk of incident MetS with regard to Vit D in 11,247 Australian adults showing the highest risk in 25(OH)D3 concentrations <24 ng/ml. Similarly, Heaney et al. [26] found a Vit D dependent transition to IR in 25(OH)D3 ranges of 40–90 ng/ml evaluating 4,116 adults. Unfortunately, these studies have not reported separate results for men and women, and it remains therefore unclear whether the link of Vit D with type 2 diabetes is distinct in men and women. A meta-analysis confirmed the inverse relationship of 25(OH)D3 concentrations with type 2 diabetes in both men and women [13]. Similarly, Hurskainen et al. and Dalgard et al. [27, 28] reported an inverse association of Vit D and type 2 diabetes after adjustment for gender. Thus, available data do not permit firm conclusions on gender differences of the association between Vit D and type 2 diabetes. Additionally, a Korean analysis suggested that the sex specificity of the association of Vit D with type 2 diabetes may change over time [14].
There is, however, circumstantial evidence that interactions between steroid hormones and Vit D homeostasis may be physiologically relevant. A link between sex hormones, specifically 17β-estradiol and local tissue Vit D homeostasis, has been demonstrated. In an elegant intervention, estrogen substitution for one month in postmenopausal women showed a significant increase in VDR and the Vit D metabolizing enzymes CYP24A1 and CYP27B1 in the rectal mucosa [29]. These findings suggest that estrogens can increase both the cellular 125(OH)D3 concentrations together with its nuclear receptor in epithelial cells of the colon, thereby augmenting the biological effectiveness of Vit D. It has been suggested that these mechanisms may account for the decreased rate of colon cancers in women on hormone replacement therapy [30].
Additionally, estradiol up-regulates VDR and CYP27B1, thereby increasing the intracellular active Vit D metabolite and its receptor in colonocytes and endothelial cell lines [31], but data of a potential interaction between estrogen and Vit D in adipose tissue or in beta-cells are lacking, and therefore, additional studies are required. Administration of Vit D together with the phytoestrogen genistein has been shown to significantly improve glycemic control and cardiovascular risk factors above Vit D alone in a two-year, randomized-double-blind study [32] demonstrating that this estrogenic compound augments Vit D effects on glucose metabolism and cardiovascular risk indicators. A similar interaction was reported in cell culture of vascular smooth muscle cells with an increased expression of CYP27B1 in response to 17β-estradiol and other estrogenic compounds [33].
Absence of estrogen receptors in breast cancer may render cells vulnerable to the absence of Vit D action [34], and introduction of VDR was necessary for re-establishing the chemopreventive action of Vit D in triple-negative cell lines [35]. Thus, data from other tissues and also malignancies demonstrate important molecular links between sex hormones and Vit D effects. Our results demonstrating an independent association of low Vit D with type 2 diabetes only in women suggest the physiological relevance of these interactions should probably be extended to the field of IR and type 2 diabetes. Hence, further studies on potential interactions between Vit D and steroid hormones in adipose tissue and likely also its stromal fraction, liver, pancreatic beta-cells and muscle may be particularly relevant.
Previous studies on the role of Vit D in type 2 diabetes implicated effects on both IR and insulin secretion [36, 37]. Our results showing that low 25(OH)D3 serum concentrations tend to be linked to both measurements of β-cell function and IR in women would be consistent with the concept that several pathways relevant to development of type 2 diabetes may be affected by inappropriately low 25(OH)D3 concentrations.
Unfortunately, only a small number of study subjects were on Vit D supplementation, and type 2 diabetes rates in these were not different from those who did not use Vit D supplements. However, the figures were not high enough to draw reliable conclusions. Inherent to the design of a cross-sectional study, our results are limited by single determinations of 25(OH)D3, whereas the development of IR and type 2 diabetes is a process even of decades. However, a recent investigation demonstrated that 25(OH)D3 concentrations were relatively stable over 14 years, suggesting that subjects deficient in Vit D remain so for long periods of time [38].
In summary, we provide clinical evidence that inadequate 25(OH)D3 serum concentrations are associated with both incident and known type 2 diabetes particularly in women. Our data suggest that interactions between sex hormones and Vit D homeostasis in adipose tissue and in beta-cells may be physiologically relevant to the development of type 2 diabetes. Although there is evidence of sex-specific associations between Vit D and fat distribution [39, 40], which may be potentially relevant to the pathogenesis of our clinical observations, further studies on gender-specific actions of Vit D in beta-cells, adipose tissue, muscle and liver are required in order to elucidate the role of Vit D in type 2 diabetes.
References
Holick MF (2007) Vitamin D deficiency. N Engl J Med 357(3):266–281. doi:10.1056/NEJMra070553
Holick MF, Chen TC (2008) Vitamin D deficiency: a worldwide problem with health consequences. Am J Clin Nutr 87(4):1080S–1086S
Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) (2001) Expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III). JAMA 285(19):2486–2497
Martini LA, Wood RJ (2006) Vitamin D status and the metabolic syndrome. Nutr Rev 64(11):479–486
Hypponen E, Power C (2006) Vitamin D status and glucose homeostasis in the 1958 British birth cohort: the role of obesity. Diabetes Care 29(10):2244–2246. doi:10.2337/dc06-0946
Kositsawat J, Freeman VL, Gerber BS, Geraci S (2010) Association of A1C levels with vitamin D status in U.S. adults: data from the national health and nutrition examination survey. Diabetes Care 33(6):1236–1238. doi:10.2337/dc09-2150
Knekt P, Laaksonen M, Mattila C, Harkanen T, Marniemi J, Heliovaara M, Rissanen H, Montonen J, Reunanen A (2008) Serum vitamin D and subsequent occurrence of type 2 diabetes. Epidemiology 19(5):666–671. doi:10.1097/EDE.0b013e318176b8ad
Grimnes G, Emaus N, Joakimsen RM, Figenschau Y, Jenssen T, Njolstad I, Schirmer H, Jorde R (2010) Baseline serum 25-hydroxyvitamin D concentrations in the Tromso Study 1994–95 and risk of developing type 2 diabetes mellitus during 11 years of follow-up. Diabetic Med J Br Diabetic Assoc 27(10):1107–1115. doi:10.1111/j.1464-5491.2010.03092.x
Parker J, Hashmi O, Dutton D, Mavrodaris A, Stranges S, Kandala NB, Clarke A, Franco OH (2010) Levels of vitamin D and cardiometabolic disorders: systematic review and meta-analysis. Maturitas 65(3):225–236. doi:10.1016/j.maturitas.2009.12.013
Robinson JG, Manson JE, Larson J, Liu S, Song Y, Howard BV, Phillips L, Shikany JM, Allison M, Curb JD, Johnson KC, Watts N (2011) Lack of association between 25(OH)D levels and incident type 2 diabetes in older women. Diabetes Care 34(3):628–634. doi:10.2337/dc10-1632
Pilz S, van den Hurk K, Nijpels G, Stehouwer CD, Van’t Riet E, Kienreich K, Tomaschitz A, Dekker JM (2012) Vitamin D status, incident diabetes and prospective changes in glucose metabolism in older subjects: the Hoorn study. Nutr Metab Cardiovasc Dis 22(10):883–889. doi:10.1016/j.numecd.2012.03.008
Rosenblum JL, Castro VM, Moore CE, Kaplan LM (2012) Calcium and vitamin D supplementation is associated with decreased abdominal visceral adipose tissue in overweight and obese adults. Am J Clin Nutr 95(1):101–108. doi:10.3945/ajcn.111.019489
Song Y, Wang L, Pittas AG, Del Gobbo LC, Zhang C, Manson JE, Hu FB (2013) Blood 25-hydroxy vitamin D levels and incident type 2 diabetes: a meta-analysis of prospective studies. Diabetes Care 36(5):1422–1428. doi:10.2337/dc12-0962
Lee BK, Park S, Kim Y (2012) Age- and gender-specific associations between low serum 25-hydroxyvitamin D level and type 2 diabetes in the Korean general population: analysis of 2008–2009 korean national health and nutrition examination survey data. Asia Pac J Clin Nutr 21(4):536–546
Stadlmayr A, Aigner E, Steger B, Scharinger L, Lederer D, Mayr A, Strasser M, Brunner E, Heuberger A, Hohla F, Steinwendner J, Patsch W, Datz C (2011) Nonalcoholic fatty liver disease: an independent risk factor for colorectal neoplasia. J Intern Med 270(1):41–49. doi:10.1111/j.1365-2796.2011.02377.x
Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE, Pratt M, Ekelund U, Yngve A, Sallis JF, Oja P (2003) International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 35(8):1381–1395. doi:10.1249/01.MSS.0000078924.61453.FB
Hahne P, Krempler F, Schaap FG, Soyal SM, Hoffinger H, Miller K, Oberkofler H, Strobl W, Patsch W (2008) Determinants of plasma apolipoprotein A-V and APOA5 gene transcripts in humans. J Intern Med 264(5):452–462. doi:10.1111/j.1365-2796.2008.01987.x
Gillett MJ (2009) International expert committee report on the role of the A1c assay in the diagnosis of diabetes: Diabetes Care 32(7):1327–1334 (Clin Biochem Rev Aust Assoc Clin Biochem 30(4):197–200)
Niederseer D, Ledl-Kurkowski E, Kvita K, Patsch W, Dela F, Mueller E, Niebauer J (2011) Salzburg skiing for the elderly study: changes in cardiovascular risk factors through skiing in the elderly. Scand J Med Sci Sports 21(Suppl 1):47–55. doi:10.1111/j.1600-0838.2011.01341.x
Ding C, Gao D, Wilding J, Trayhurn P, Bing C (2012) Vitamin D signalling in adipose tissue. Br J Nutr 108(11):1915–1923. doi:10.1017/S0007114512003285
Uberti F, Lattuada D, Morsanuto V, Nava U, Bolis G, Vacca G, Squarzanti DF, Cisari C, Molinari C (2013) Vitamin D protects human endothelial cells from oxidative stress through the autophagic and survival pathways. J Clin Endocrinol Metab. doi:10.1210/jc.2013-2103
Cross HS, Bises G, Lechner D, Manhardt T, Kallay E (2005) The vitamin D endocrine system of the gut—its possible role in colorectal cancer prevention. J Steroid Biochem Mol Biol 97(1–2):121–128. doi:10.1016/j.jsbmb.2005.06.005
Clark SA, Stumpf WE, Sar M, DeLuca HF, Tanaka Y (1980) Target cells for 1,25 dihydroxyvitamin D3 in the pancreas. Cell Tissue Res 209(3):515–520
Brozek W, Manhardt T, Kallay E, Peterlik M, Cross HS (2012) Relative expression of vitamin D hydroxylases, CYP27B1 and CYP24A1, and of cyclooxygenase-2 and heterogeneity of human colorectal cancer in relation to age, gender, tumor location, and malignancy: results from factor and cluster analysis. Cancers 4(3):763–776. doi:10.3390/cancers4030763
Gagnon C, Lu ZX, Magliano DJ, Dunstan DW, Shaw JE, Zimmet PZ, Sikaris K, Ebeling PR, Daly RM (2012) Low serum 25-hydroxyvitamin D is associated with increased risk of the development of the metabolic syndrome at five years: results from a national, population-based prospective study (The Australian diabetes, obesity and lifestyle study: AusDiab). J Clin Endocrinol Metab 97(6):1953–1961. doi:10.1210/jc.2011-3187
Heaney RP, French CB, Nguyen S, Ferreira M, Baggerly LL, Brunel L, Veugelers P (2013) A novel approach localizes the association of vitamin D status with insulin resistance to one region of the 25-hydroxyvitamin D continuum. Adv Nutr 4(3):303–310. doi:10.3945/an.113.003731
Hurskainen AR, Virtanen JK, Tuomainen TP, Nurmi T, Voutilainen S (2012) Association of serum 25-hydroxyvitamin D with type 2 diabetes and markers of insulin resistance in a general older population in Finland. Diabetes Metab Res Rev 28(5):418–423. doi:10.1002/dmrr.2286
Dalgard C, Petersen MS, Weihe P, Grandjean P (2011) Vitamin D status in relation to glucose metabolism and type 2 diabetes in septuagenarians. Diabetes Care 34(6):1284–1288. doi:10.2337/dc10-2084
Protiva P, Cross HS, Hopkins ME, Kallay E, Bises G, Dreyhaupt E, Augenlicht L, Lipkin M, Lesser M, Livote E, Holt PR (2009) Chemoprevention of colorectal neoplasia by estrogen: potential role of vitamin D activity. Cancer Prev Res (Phila) 2(1):43–51. doi:10.1158/1940-6207.CAPR-08-0103
Barzi A, Lenz AM, Labonte MJ, Lenz HJ (2013) Molecular pathways: estrogen pathway in colorectal cancer. Clin Cancer Res Off J Am Assoc Cancer Res 19(21):5842–5848. doi:10.1158/1078-0432.CCR-13-0325
Lechner D, Cross HS (2003) Phytoestrogens and 17beta-estradiol influence vitamin D metabolism and receptor expression-relevance for colon cancer prevention. Recent Results Cancer Res 164:379–391
Atteritano M, Marini H, Minutoli L, Polito F, Bitto A, Altavilla D, Mazzaferro S, D’Anna R, Cannata ML, Gaudio A, Frisina A, Frisina N, Corrado F, Cancellieri F, Lubrano C, Bonaiuto M, Adamo EB, Squadrito F (2007) Effects of the phytoestrogen genistein on some predictors of cardiovascular risk in osteopenic, postmenopausal women: a two-year randomized, double-blind, placebo-controlled study. J Clin Endocrinol Metab 92(8):3068–3075. doi:10.1210/jc.2006-2295
Somjen D, Weisman Y, Kohen F, Gayer B, Limor R, Sharon O, Jaccard N, Knoll E, Stern N (2005) 25-Hydroxyvitamin D3-1alpha-hydroxylase is expressed in human vascular smooth muscle cells and is upregulated by parathyroid hormone and estrogenic compounds. Circulation 111(13):1666–1671. doi:10.1161/01.CIR.0000160353.27927.70
Yao S, Ambrosone CB (2013) Associations between vitamin D deficiency and risk of aggressive breast cancer in African-American women. J Steroid Biochem Mol Biol 136:337–341. doi:10.1016/j.jsbmb.2012.09.010
Laporta E, Welsh J (2013) Modeling vitamin D actions in triple negative/basal-like breast cancer. J Steroid Biochem Mol Biol. doi:10.1016/j.jsbmb.2013.10.022
Chiu KC, Chu A, Go VL, Saad MF (2004) Hypovitaminosis D is associated with insulin resistance and beta cell dysfunction. Am J Clin Nutr 79(5):820–825
Deleskog A, Hilding A, Brismar K, Hamsten A, Efendic S, Ostenson CG (2012) Low serum 25-hydroxyvitamin D level predicts progression to type 2 diabetes in individuals with prediabetes but not with normal glucose tolerance. Diabetologia 55(6):1668–1678. doi:10.1007/s00125-012-2529-x
Voorham QJ, Rondagh EJ, Knol DL, van Engeland M, Carvalho B, Meijer GA, Sanduleanu S (2013) Tracking the molecular features of nonpolypoid colorectal neoplasms: a systematic review and meta-analysis. Am J Gastroenterol 108(7):1042–1056. doi:10.1038/ajg.2013.126
Lee K (2013) Body composition and vitamin D status: the Korea National Health And Nutrition Examination Survey IV (KNHANES IV). J Hum Nutr Diet Off J Br Dietetic Assoc 26(Suppl 1):105–113. doi:10.1111/jhn.12047
Bolland MJ, Grey AB, Ames RW, Mason BH, Horne AM, Gamble GD, Reid IR (2007) The effects of seasonal variation of 25-hydroxyvitamin D and fat mass on a diagnosis of vitamin D sufficiency. Am J Clin Nutr 86(4):959–964
Acknowledgments
We gratefully acknowledge laboratory technical support by Elke Albrecht, Monika Ratkowitsch, Carmen Winkler, Oberndorf Hospital; Angela Eich, First Department of Medicine, Paracelsus Medical University Salzburg; Silke Winkler, Department of Internal Medicine 3 and Institute for Clinical Immunology, University of Erlangen-Nuremberg, Germany and support from SPAR Austria to Christian Datz is gratefully acknowledged.
Conflicts of interest
None of the authors have any potential conflicts of interest to declare with regard to this investigation.
Human and animal rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Informed consent
Informed consent was obtained from all patients for being included in the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Managed by Massimo Porta.
Wolfgang Patsch and Christian Datz have contributed equally to this manuscript.
Rights and permissions
About this article
Cite this article
Stadlmayr, A., Aigner, E., Huber-Schönauer, U. et al. Relations of vitamin D status, gender and type 2 diabetes in middle-aged Caucasians. Acta Diabetol 52, 39–46 (2015). https://doi.org/10.1007/s00592-014-0596-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-014-0596-9