Abstract
The prevalence of very severe obesity has increased progressively and faster than other classes of obesity over the last years. It is unclear whether the prevalence of obesity-related complications and health risks increases progressively or reaches a plateau above a certain degree of obesity. The aim of our study was to investigate whether the severity of obesity was correlated with the prevalence of type 2 diabetes mellitus (T2DM), impaired fasting glucose, impaired glucose tolerance (IGT), metabolic syndrome (MS), and cardiovascular diseases (CVDs) in a large cohort of patients with different degrees of obesity. A cross-sectional study was conducted in 938 obese patients without a previous diagnosis of diabetes. Patients were assigned to different categories of obesity: mild-moderate obesity (BMI 30–39.9 kg/m2), morbid obesity (BMI 40–49.9 kg/m2), and super-obesity (SO, BMI ≥50 kg/m2). The prevalence of IGF, IGT, screen-detected T2DM, MS, and CVD was higher in SO patients than in the other groups. Interestingly, the association between SO and either MS or CVD was independent of glucose tolerance status, indicating that factors other than glucose metabolism also favor cardio-metabolic complications in obese patients. In patients without screen-detected T2DM (n = 807), insulin sensitivity and secretion OGTT-derived indexes indicated that SO patients had the worst glucose homeostasis relative to the other categories of obesity, which was indicated by the most reduced disposition index in these patients, a predictor of future T2DM. In conclusion, SO patients have an extremely high prevalence of glucose metabolism deterioration, and cardio-metabolic complications are more prevalent in these patients compared to less obese patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity is dramatically increasing throughout the world. A recent study showed that more than one-third of US adults are obese [1]. Similarly, almost half of Italian men and approximately one-third of Italian women are overweight or obese. From 2001 to 2008, the age-standardized prevalence of overweight and obesity increased in Italy by 1.4 and 1.9 % in men and 0.4 and 0.5 % in women, respectively [2]. Obesity increases mortality from all causes and cardiovascular risk. In particular, obesity is associated with insulin resistance and other metabolic complications such as type 2 diabetes mellitus (T2DM), dyslipidemia, and hypertension. Obesity is also a major component of metabolic syndrome, a cluster of metabolic and clinical conditions associated with elevated cardiovascular disease risk [3, 4]. The T2DM prevalence increases with age [5] and BMI, reaching 18.3 % in obese individuals (over 35 kg/m2) [6]. Data on the prevalence of these metabolic diseases in very morbidly obese patients are scarce.
Very morbid obesity (BMI >50 kg/m2), also defined as super-obesity, has increased significantly and faster than any other class of obesity [7]. Its prevalence increased by 52 % in the USA between 2000 and 2005 [8]. It is unclear whether the prevalence of obesity-related metabolic complications and health risks increases progressively with BMI or reaches a plateau above a certain degree of obesity [9, 10]. While some data indicate that the risk of developing complications is proportional to the degree of obesity [11], the presence of metabolic abnormalities varies widely among obese individuals of the same category.
The aim of our study was to define the prevalence of cardio-metabolic risk factors (such as impaired fasting glucose, impaired glucose tolerance, T2DM, and metabolic syndrome) and cardiovascular events in a continuous series of obese patients with different degrees of obesity.
Patients and methods
A total of 1,258 obese (BMI ≥30 kg/m2) patients (387 males, 871 females; mean age = 40.2 ± 13.4 years, range 18–75 years; mean BMI 44.7 ± 9.4 kg/m2, range 30.0–84.2 kg/m2) referred to our Obesity Center (University of Catania Medical School, Garibaldi Hospital Medical Center, Catania, Italy) for weight loss management were consecutively recruited from January 2009 to December 2010. The exclusion criteria were pregnancy (n = 24) and the presence of acute and/or severe organ disease (n = 73). To evaluate the effect of obesity on cardio-metabolic complications, patients with known T2DM were excluded (223 out of a total of 1,258 patients screened, 17.7 %) from the study to avoid the confounding effect of hyperglycemia on the parameters examined. In total, 938 obese patients were included in the study (270 males, 668 females).
All patients gave informed consent, and investigations were performed in accordance with the principles of the Declaration of Helsinki. The Ethical Committee of the hospital approved the study.
All participants underwent a physical examination and were maintained on a weight-maintaining diet for 4 days before performing the metabolic study. The age of obesity onset was recorded from self-reports. Height was measured to the nearest 0.1 cm, and body weight was measured with a 0.1 kg precision with the subjects wearing light indoor clothing without shoes. Blood pressure was measured twice with the subject in a sitting position after a minimum of 5 min of acclimatization and before blood sampling. The mean of the two blood pressure measurements was used in the analysis.
Blood specimens were obtained after an overnight fast as previously described, and glucose, insulin, triglycerides, and total and HDL cholesterol levels were measured using commercially available kits [12].
Classification of obesity
BMI was calculated as weight (kg) divided by height × height (m2). Obesity was defined as BMI ≥30 kg/m2. The patients were assigned to three categories according to BMI: mild-moderate obesity (MMO, n = 306, BMI 30–39.9 kg/m2), morbid obesity (MO, n = 374, BMI 40–49.9 kg/m2), and super-obesity (SO, n = 258, BMI ≥50 kg/m2).
Glucose tolerance status and metabolic syndrome
All patients with fasting plasma glucose (FPG) <7 mmol/l (889 out of 938) underwent an oral glucose tolerance test (OGTT), measuring glucose and insulin values before and 30, 60, 90, and 120 min after glucose load (75 g). T2DM, impaired fasting glucose (IFG), and impaired glucose tolerance (IGT) were defined according to the ADA criteria [13]. Individuals who had not been diagnosed as diabetic but who had a fasting plasma glucose level ≥7 mmol/l and/or 2 h plasma glucose ≥11.1 mmol/l were classified as having screen-detected T2DM (n = 131).
Metabolic syndrome was defined according to the ATP-III classification [3], which requires three or more of the following five components: large waist circumference (>102 cm in men and >88 cm in women), hypertriglyceridemia (≥1.7 mmol/l) or antihyperlipidemia treatment, low HDL cholesterol level (<1.0 mmol/l in men or <1.3 mmol/l in women), elevated blood pressure (systolic ≥130 mmHg and/or diastolic ≥85 mmHg and/or antihypertensive treatment or a history of hypertension), and elevated fasting plasma glucose (≥5.5 mmol/l).
Insulin sensitivity and secretion
Insulin sensitivity and secretion were evaluated by OGTT-derived indexes in patients who had not been classified as having screen-detected T2DM (n = 807). Insulin sensitivity was calculated according to Matsuda’s index (insulin sensitivity index, ISI), as previously described [14]. Insulin secretion was calculated according to the insulinogenic index (IGI) [15]. The disposition index (DI) was calculated as IGI × ISI [15, 16]. Of note, potential violations of the hyperbolic shape (IGI × ISI = k, where k is a constant value) were excluded using a goodness-of-fit test for the following nonlinear model IGI = k/ISI (R 2 = 0.41, p < 0.0001).
Cardiovascular disease
The recorded cardiovascular comorbidities included a documented history of myocardial infarction (MI) or stroke, heart failure (HF), atrial fibrillation (AF), or deep vein thrombosis (DVT) [17].
Statistical analysis
Values are provided as the mean ± SD (text and table) or as the mean ± SEM (figures). No normally distributed variables (plasma insulin, triglycerides, IGI, and DI) were log transformed for analysis.
Continuous variables were compared between groups using an unpaired t test or an analysis of variance (ANOVA). After adjusting for several covariates, differences between groups were evaluated by a covariance analysis (ANCOVA) followed by a post hoc analysis with Fisher’s protected least-significant difference test (PLSD). Simple and multiple regression models were used to test for correlations between continuous variables.
Categorical variables were compared by the chi-square test. Multivariate logistic regression models were applied to assess the risk of cardio-metabolic diseases in the different categories of obesity. The dependent variable in this model was the binary status of cardio-metabolic disease (T2DM, prediabetes, metabolic syndrome, and cardiovascular disease). The degree of obesity was the main predictor included as a continuous variable (MMO category = 0, MO = 1, SO = 2). Analyses were adjusted for age and gender, and the results are presented as adjusted odds ratios (ORs) with 95 % confidence intervals (CIs).
The significance limit was set at p values <0.05. Data analyses were performed using the StatView 5.01 (SAS Institute, Cary, North Carolina, USA) and SPSS (version 15; SPSS Inc., Chicago, IL, USA) statistical packages.
Results
Obesity, age of onset, and gender
The anthropometric and clinical characteristics of the 938 patients included in the study are shown in Table 1 stratified in three categories according to BMI.
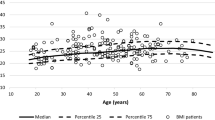
The male/female ratio decreased progressively with the increasing severity of obesity from MMO (76/230 subjects, 33 %) to MO (103/271, 38 %) and SO (91/167, 54 %) patients (p for trend ≤0.01 after adjusting for age). Super-obese patients were slightly but significantly older (39.5 ± 12.3 years) than MMO (35.6 ± 11.8 years) and MO patients (37.0 ± 12.0 years) (p ≤ 0.01 for both after adjusting for gender). Interestingly, patients with more severe obesity (MO and SO) reported an earlier onset of obesity than MMO patients (mean age at onset 14.1 ± 10.5 and 14.4 ± 10.3 vs. 21.7 ± 12.0 years, respectively; p < 0.0001 after adjusting for age and gender). Additionally, a longer disease duration was observed from MMO (13.9 ± 8.9 years) to MO (23.0 ± 11.5 years) and SO (25.1 ± 11.1 years) patients (p < 0.0001 after adjusting for age and gender). In the post hoc analysis, the obesity duration was significantly higher in SO individuals compared with MO (p < 0.005) and MMO (p < 0.0001) individuals; the difference between the MO and MMO categories was also highly significant (p < 0.0001). Moreover, a significant linear correlation (r = −0.23, p < 0.0001) was found between the individual BMIs and the age of obesity onset. Together, these data suggest that the most severe degrees of obesity are associated with an increasing percentage of male patients with an earlier onset of obesity.
Prevalence of glucose metabolism abnormalities and metabolic syndrome
The fasting blood glucose, serum insulin and triglycerides, and systolic and diastolic blood pressure progressively increased from MMO to MO and SO patients (differences between groups in the post hoc analysis after adjusting for age and gender are shown in Table 1).
The prevalence of screen-detected T2DM was 14 % in the entire cohort and progressed significantly from MMO (6.5 %, 20/230 subjects) to MO (15.5 %, 58/271) and SO (20.5 %, 53/167) patients (p for trend <0.0001) (Table 2). In the multivariate logistic regression analysis, the risk of having screen-detected T2DM significantly increased from MMO to MO and SO patients (OR 1.67; CI 1.30–2.16; p < 0.0001 after adjusting for age and gender). Similarly, the prevalence of prediabetes (IFG and/or IGT) was 41.4 % in the entire cohort and progressed significantly from MMO (34.3 %) to MO (41.2 %) and SO (50.0 %) patients (p for trend <0.0001) (Table 2). The multivariate logistic regression analysis confirmed that the risk of having prediabetes was significantly increased in MO and SO patients compared to MMO patients (OR 1.34; 95 % CI 1.13–1.60; p ≤ 0.001 after adjusting for age and gender).
The prevalence of metabolic syndrome was 58.2 % in the entire cohort and progressed significantly from MMO (47.1 %) to MO (56.7 %) and SO (73.6 %) patients (p for trend <0.0001). The risk of this syndrome increased significantly and progressively from MMO to MO and SO patients (OR 1.60; 95 % CI 1.33–1.93; p < 0.0001 after adjusting for age and gender). Interestingly, the association between the prevalence of metabolic syndrome and the degree of obesity remained significant after adjusting for glucose tolerance status (OR 1.28; 95 % CI 1.05–1.57; p ≤ 0.01 after adjusting for age, gender and glucose tolerance status).
Insulin sensitivity and secretion in non-diabetic obese patients
Insulin sensitivity, evaluated by the ISI value, significantly decreased in the different obesity categories (higher in MMO, lower in SO, p < 0.0001 after adjusting for age and gender) (Fig. 1a). In the post hoc analysis, the ISI value was significantly (p < 0.0001) reduced in SO individuals (2.50 ± 1.18) compared with MO (3.16 ± 1.69) and MMO (3.67 ± 2.18) individuals; moreover, ISI was significantly lower in MO individuals compared to MMO individuals (p < 0.0005) (Fig. 1a). Additionally, insulin secretion, as indicated by the insulinogenic index (IGI) values, progressively decreased from MMO to MO and SO patients (p < 0.05 after adjusting for age and gender) (Fig. 1b). In the post hoc analysis, the IGI value was significantly (p ≤ 0.001) reduced in both SO (27.4 ± 18.3) and MO (27.9 ± 20.0) individuals compared to MMO (30.7 ± 18.8) individuals. Finally, the disposition index (DI; i.e., the product of the IGI and the ISI values) significantly differed across the three groups (p < 0.0001 after adjusting for age and gender) (Fig. 1c). In the post hoc analysis, the DI was reduced in SO (61.7 ± 47.5) individuals when compared with MO (84.9 ± 76.8; p < 0.005) and MMO (110.1 ± 108.3; p < 0.0001) individuals. The difference between the MO and MMO categories was also highly significant (p ≤ 0.005, Fig. 1c).
OGTT-derived indexes in the different obesity categories. Insulin sensitivity index (a), insulinogenic index (b), and disposition index (c) values in MMO (mild-moderate obesity, white bars), MO (morbid obesity, gray bars), and SO (super-obesity, black bars) patients. All data were adjusted for age and gender. a *p < 0.0005 versus MMO; °p < 0.0001 versus MO and MMO; b # p ≤ 0.001 versus MMO; c ^p ≤ 0.005 versus MMO; § p < 0.005 versus MO; + p < 0.0001 versus MMO
Prevalence of cardiovascular disease
The prevalence of cardiovascular disease also increased with increasing obesity (Table 2) with 0.3 % in MMO patients, 1.9 % in MO patients, and 5.8 % in SO patients (p for trend <0.0001), and the risk progressively increased in the different obesity categories (OR 3.4; 95 % CI 1.65–7.08; p < 0.001 after adjusting for age and gender). Interestingly, this association remained significant after adjusting for glucose tolerance status (OR 3.4; 95 % CI 1.61–7.05; p ≤ 0.001 after adjusting for age, gender, and glucose tolerance status).
Discussion
Our data indicate that SO patients have a younger age at obesity onset and higher prevalence of metabolic alterations and cardiovascular disease compared to MMO patients.
The inverse correlation between BMI and age at obesity onset supports the previously reported role of childhood overweight and obesity as a risk factor for the development of severe obesity later in life [18, 19]. Both a longer exposure of these patients to the causative factors of obesity and a genetic background favoring fat accumulation can explain this association. Patients with very morbid obesity (BMI ≥50 kg/m2) have a more abnormal metabolic profile than less obese patients. The risk of having metabolic abnormalities such as undiagnosed diabetes, prediabetes, and metabolic syndrome increased significantly and progressively from mild to severe obesity.
In super-obese patients, the prevalence of undiagnosed diabetes is higher than expected in the adult Italian population [20, 21], and our data demonstrated that it was also 1.3-fold higher in SO patients than in MO patients and 3.1-fold higher when compared to MMO patients. Similar results were observed for the presence of prediabetes (IFG or IGT), with a significant increase from the lowest to the highest degree of obesity. Considering diabetes and prediabetes together, these abnormalities were present in 55 % of obese individuals and reached 70 % in SO patients. Moreover, such a high prevalence of glucose homeostasis abnormalities in the most severe categories of obesity suggests that appropriate screening tools should be used in all these patients, including foremost the OGTT, which can identify both diabetes and IGT.
Additionally, the prevalence of metabolic syndrome increased progressively with the degree of obesity. The observation that the frequency of cardiovascular events increased with increasing obesity independently of the level of glucose metabolism derangement in a multivariate logistic regression analysis suggests that other factors, such as the level of dyslipidemia, increased blood pressure, and increased cardiac effort due to body mass, are major contributors to cardiovascular damage in severely obese patients.
Super-obesity is clearly associated with an increased risk of death due to many chronic diseases. At a BMI of 40–45 kg/m2, median survival is reduced by 8–10 years; for a BMI between 25 and 50 kg/m2, each 5 kg/m2 BMI increase is associated with approximately 40 % higher mortality due to ischemic heart disease, stroke, and other vascular causes [22].
Non-diabetic SO patients also had a more abnormal glucose homeostasis during OGTT due to an inefficient interplay between insulin secretion and insulin sensitivity (i.e., a reduced disposition index), the best predictor of future T2DM. In hyperglycemic individuals, the disposition index may be reduced because of decreased insulin secretion, increased insulin resistance, or both. Our data indicate that higher degrees of obesity are associated with both impaired insulin secretion and increased insulin resistance in non-diabetic patients. Therefore, these individuals have a very high risk of developing T2DM. The insulinogenic index, the ratio of the increment in insulin concentration to the increment in glucose concentration during OGTT, however, is a surrogate measure of insulin secretion. The circulating levels of insulin, indeed, reflect both insulin secretion and clearance and C-peptide concentrations after the OGTT would be preferable to calculate the insulin secretion rate through C-peptide deconvolution. Nevertheless, the OGTT-derived indexes used in this study (insulinogenic index, insulin sensitivity index, and disposition index) have been validated for large-scale and epidemiologic studies [15, 16, 23, 24].
Several previous studies investigated the metabolic abnormalities associated with obesity, but few data are available in super-obese patients. Some of these studies reported that certain parameters of metabolic status worsen as the severity of SO increases, whereas others found that the metabolic situation remains the same or even improves with more severe stages of obesity [9–11, 25]. The reasons for the conflicting results in the various studies are unknown but may occur secondarily to the limited numbers of study subjects in some of these reports. A recent study showed that both pre- and postmenopausal severely obese women had a better lipid profile than moderately obese women [26]. Nevertheless, the use of medications for diabetes and hypertension was significantly higher in the severely obese women when compared to the moderately obese women.
Conclusions
In conclusion, our data demonstrated that the prevalence of metabolic abnormalities (diabetes, prediabetes, and metabolic syndrome) and cardiovascular disease substantially increased with increasing BMI, suggesting that super-obese patients have a higher cardiovascular risk than the moderately obese patients.
These findings have important public health implications for the prevention (which has to begin during childhood with specific educational intervention programs), management (which requires an adaptation of structures designed to accommodate this type of patient), and treatments (surgical and non-surgical) of morbid and very morbid obesity.
References
Flegal KM, Carroll MD, Kit BK, Ogden CL (2012) Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA 307:491–497
Micciolo R, Di Francesco V, Fantin F, Canal L, Harris TB et al (2010) Prevalence of overweight and obesity in Italy (2001–2008): is there a rising obesity epidemic? Ann Epidemiol 20:258–264
Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (2001) Executive summary of the third report of the national cholesterol education program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III). JAMA 285: 2486–2497. http://www.ncbi.nlm.nih.gov/pubmed/11368702
Oda E (2012) Metabolic syndrome: its history, mechanisms, and limitations. Acta Diabetol 49:89–95
Cowie CC, Rust KF, Byrd-Holt DD, Gregg EW, Ford ES et al (2010) Prevalence of diabetes and high risk for diabetes using A1C criteria in the U.S. population in 1988–2006. Diabetes Care 33:562–568
Gregg EW, Cadwell BL, Cheng YJ, Cowie CC, Williams DE et al (2004) Trends in the prevalence and ratio of diagnosed to undiagnosed diabetes according to obesity levels in the U.S. Diabetes Care 27:2806–2812
Flegal KM, Carroll MD, Ogden CL, Curtin LR (2010) Prevalence and trends in obesity among US adults, 1999–2008. JAMA 303:235–241
Sturm R (2007) Increases in morbid obesity in the USA: 2000–2005. Public Health 121:492–496
Dixon JB, O’Brien P (2001) A disparity between conventional lipid and insulin resistance markers at body mass index levels greater than 34 kg/m(2). Int J Obes Relat Metab Disord 25:793–797
Wolf AM, Buffington C, Beisiegel U (2006) Comparison of metabolic risk factors between severely and very severely obese patients. Obesity (Silver Spring) 14:2177–2183
Nguyen NT, Magno CP, Lane KT, Hinojosa MW, Lane JS (2008) Association of hypertension, diabetes, dyslipidemia, and metabolic syndrome with obesity: findings from the national health and nutrition examination survey, 1999 to 2004. J Am Coll Surg 207:928–934
Baratta R, Amato S, Degano C, Farina MG, Patane G et al (2004) Adiponectin relationship with lipid metabolism is independent of body fat mass: evidence from both cross-sectional and intervention studies. J Clin Endocrinol Metab 89:2665–2671
American Diabetes Association (2011) Diagnosis and classification of diabetes mellitus. Diabetes Care 34 (Suppl 1):S62–S69. http://www.ncbi.nlm.nih.gov/pubmed/21193628
Baratta R, Di Paola R, Spampinato D, Fini G, Marucci A et al (2003) Evidence for genetic epistasis in human insulin resistance: the combined effect of PC-1 (K121Q) and PPARgamma2 (P12A) polymorphisms. J Mol Med (Berl) 81:718–723
Baratta R, Rossetti P, Prudente S, Barbetti F, Sudano D et al (2008) Role of the ENPP1 K121Q polymorphism in glucose homeostasis. Diabetes 57:3360–3364
Abdul-Ghani MA, Williams K, DeFronzo RA, Stern M (2007) What is the best predictor of future type 2 diabetes? Diabetes Care 30:1544–1548
Murphy NF, MacIntyre K, Stewart S, Hart CL, Hole D et al (2006) Long-term cardiovascular consequences of obesity: 20-year follow-up of more than 15 000 middle-aged men and women (the Renfrew-Paisley study). Eur Heart J 27:96–106
O’Connell J, Kieran P, Gorman K, Ahern T, Cawood TJ et al (2010) BMI > or = 50 kg/m2 is associated with a younger age of onset of overweight and a high prevalence of adverse metabolic profiles. Public Health Nutr 13:1090–1098
Ferraro KF, Thorpe RJ Jr, Wilkinson JA (2003) The life course of severe obesity: does childhood overweight matter? J Gerontol B Psychol Sci Soc Sci 58:S110–S119
Monesi L, Baviera M, Marzona I, Avanzini F, Monesi G et al (2012) Prevalence, incidence and mortality of diagnosed diabetes: evidence from an Italian population-based study. Diabet Med 29(3):385–392. http://www.ncbi.nlm.nih.gov/pubmed/21913971
Muntoni S, Atzori L, Mereu R, Manca A, Satta G et al (2009) Prevalence of diagnosed and undiagnosed diabetes mellitus and impaired fasting glucose in Sardinia. Acta Diabetol 46:227–231
Whitlock G, Lewington S, Sherliker P, Clarke R, Emberson J et al (2009) Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet 373:1083–1096
Hanson RL, Pratley RE, Bogardus C, Narayan KM, Roumain JM et al (2000) Evaluation of simple indices of insulin sensitivity and insulin secretion for use in epidemiologic studies. Am J Epidemiol 151:190–198
Goodarzi MO, Cui J, Chen YD, Hsueh WA, Guo X et al (2011) Fasting insulin reflects heterogeneous physiological processes: role of insulin clearance. Am J Physiol Endocrinol Metab 301:E402–E408
Perotto M, Panero F, Gruden G, Fornengo P, Lorenzati B et al (2011) Obesity is associated with lower mortality risk in elderly diabetic subjects: the casale monferrato study. Acta Diabetol [Epub ahead of print]. http://www.ncbi.nlm.nih.gov/pubmed/22068621
Drapeau V, Lemieux I, Richard D, Bergeron J, Tremblay A et al (2006) Metabolic profile in severely obese women is less deteriorated than expected when compared to moderately obese women. Obes Surg 16:501–509
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Communicated by Massimo Federici.
Federica Vinciguerra and Roberto Baratta equally contributed.
Rights and permissions
About this article
Cite this article
Vinciguerra, F., Baratta, R., Farina, M.G. et al. Very severely obese patients have a high prevalence of type 2 diabetes mellitus and cardiovascular disease. Acta Diabetol 50, 443–449 (2013). https://doi.org/10.1007/s00592-013-0460-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-013-0460-3