Abstract
There is a growing debate in the literature on whether glucose variability contributes, as well as high HbA1c levels and longstanding diabetes, to the onset and progression of diabetic retinopathy (DR) in patients with diabetes types 1 (DM1) and 2 (DM2). Few data, obtained only by self-monitoring of blood glucose, support this hypothesis. We used continuous glucose monitoring (CGM) to investigate the association between DR and glucose variability parameters (SD, CONGA 2, MAGE), acute hyperglycemia (HBGI) and chronic exposure to glucose (AG and AUC tot). We studied 68 patients from 19 to 69 years old, 35 with DM1 and 33 with DM2. The prevalence of retinopathy was 43 % in DM 1 patients and 39 % in DM 2 patients. The values of all indicators were obtained by CGM for 72 h. DR was diagnosed on direct or indirect ophthalmoscopic examination, after inducing mydriasis with tropicamide. HbA1c was measured at the baseline and 6 weeks after CGM to test the stability of the patients’ glycemic control. Univariate analysis showed a close association between DR and duration of diabetes (OR 1.11; 1.04–1.19), intensive insulin therapy (OR 5.6, CI 1.14–27.30), SD (OR 1.03; CI 1.01–1.06) and CONGA 2 (OR 1.02; CI 1.00–1.04)—both indicators of variability and HBGI (OR 1.1, CI 1.01–1.18)—a parameter reflecting acute hyperglycemia. There was no significant correlation with HbA1c (p = 0.070). Multivariate regression analysis showed that disease duration is the parameter most significantly correlating with DR (OR 1.05; 1.01–1.15). These results reinforce the evidence that longstanding disease is the factor most closely associated with DR. Our data also suggest, however, that glucose variability—regardless of HbA1c—may also have a role as a risk factor for DR, particularly in the case of acute fluctuations (as represented by CONGA 2 and SD) and acute hyperglycemia (as represented by HBGI).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetic retinopathy (DR) is the most common microvascular complication of diabetes, and one of the leading causes of poor visual acuity and blindness in many developed countries [1]. The Wisconsin Epidemiological Study on Diabetic Retinopathy (WESDR) reported an overall 10-year incidence of retinopathy of 74 % among diabetic patients, while 20 % of them (be they type 1 [DM1] or type 2 [DM2] diabetics) developed macular edema during a 10-year follow-up [2].
In a recent in-depth review published in The Lancet, Cheung et al. [3] included exposure to sustained hyperglycemia, longstanding diabetes, poor blood pressure control and certain ethnic origins among the well-established risk factors for DR. The pathological role of chronic hyperglycemia has been established by large-scale prospective studies, that is, the Diabetes Control and Complications Trial (DCCT) [4] for DM1 and the United Kingdom Prospective Diabetes Study (UKPDS) [5] for DM2. These two landmark trials showed a close relationship between HbA1c and the risk of DR progressing. On the other hand, further analysis of the DCCT data showed that, although intensive therapy reduced the risk of DR progressing by 73 % compared to standard treatment, high HbA1c levels and longstanding diabetes explained only 11 % of the variation in the risk of retinopathy [6], giving the impression that other factors may contribute to the overall risk of DR progression.
Aiming to explain the so-called glycemic memory or legacy effect, Brownlee et al. [7, 8] looked into the epigenetic changes caused by the production of mitochondrial superoxide as a possible mechanism adding to vascular damage. Such a pathological cascade would be triggered by the short-term hyperglycemic spikes typical of patients with a high glucose variability. A number of studies consequently posed the question of whether glucose variability, irrespective of HbA1c, could confer an additional risk for the development of microvascular diabetic complications [9], but its role remains controversial, especially in DM1 [10].
Analyses on the relationship between glucose variability and DR have focused mainly on further analyzing the DCCT findings or data from the self-monitoring of blood glucose (SMBG) [9]. Current continuous glucose monitoring (CGM) systems are capable of grasping the direction and magnitude of short-lived changes in glucose levels and can therefore assess glucose variability more accurately than SMBG measurements [11].
To date, no studies have examined the association between glucose variability (as expressed by CGM readings) and DR in patients with DM1 or DM2.
The aim of this work was therefore to establish whether high glucose variability, as measured by CGM, is associated with an increased risk of DR, regardless of patients’ HbA1c levels and other established risk factors.
Materials and methods
Patients
Data were obtained on 35 DM1 and 33 DM2 patients (37 women and 31 men, aged 19 to 69 years) attending the Diabetology and Dietetics Service in Padua (Italy). These patients had already been recruited for the A1c-derived average glucose (ADAG) trial [12], and additional data were reported in our previous publication [13].
The patients had to have a stable glycemic control (as demonstrated by two HbA1c readings differing by no more than 1 %) during the 6 months prior to the start of the study.
Duration of diabetes was defined as the known years of disease as at the time of recruitment. Patients’ body mass index (BMI) was calculated by dividing their weight in kilograms by the square of their height in meters. Patients with DM2 were treated with oral hypoglycemic agents or insulin (always using a basal bolus regimen for the latter). Macroangiopathy was assessed from clinical history (specified from charts) of myocardial infarction, angina pectoris, coronary artery surgery, angioplasty and peripheral vascular disease (brain and lower extremities). Microalbuminuria was defined as a urinary albumin excretion level between 30 and 299 mg/g creatinine on at least two of three occasions; macroalbuminuria was defined as a urinary albumin excretion level ≥300 mg/g creatinine on at least two of three occasions.
The study was approved by our local human studies committees and has been performed in accordance with the ethical standards of Declaration of Helsinki. Informed consent was obtained from all participants.
Glucose variability measurements and laboratory tests
Glucose variability indicators were calculated from CGM (Medtronic MiniMed) data, disregarding the first 2 h of the monitoring session, which served as the initial instrument calibration period. Data were analyzed retrospectively, and patients were blinded to their glucose values. For the Medtronic MiniMed, previous medical publications have indicated median relative absolute differences (RAD) of 11 % between paired CGM findings and reference serum glucose values, which is lower than with the first-generation CGM equipment [14]. All CGM sessions were completed correctly, with 100 % of the data available for statistical analysis.
The monitoring periods lasted at least 72 h and glucose levels were recorded every 5 min, obtaining a total of ~800 measurements per patient. Using these data, indicators were calculated with complex formulas designed specifically for CGM data [15]. We considered average glucose (AG) as an indicator of metabolic control [16]. Short-lived glucose variability was assessed by measuring the standard deviation of the blood glucose rate of change (SD-BG ROC), the mean amplitude of glucose excursions (MAGE) and the continuous overlapping net glycemic action calculated every 2 h during the monitoring period (CONGA 2). We also considered the HBGI (high blood glucose index) for the purposes of assessing the hyperglycemic risk.
The MAGE was calculated as the arithmetic mean of the differences between consecutive glycemic peaks and nadirs, only considering changes in the glycemic values of more than 1 SD [17]. The CONGA is the SD of the glycemic differences recorded between a specific point on the CGM profile and a point n hours previously (where n = 1,2,3,4,…) [18]. The HBGI and SD-BG ROC were calculated using complex formulas designed specifically to obtain these indicators from CGM data [19].
As for HbA1c levels, four different DCCT-aligned assays were performed according to the ADAG protocol, that is, one high-performance liquid chromatography assay, two immunoassays and one affinity assay (all as approved by the National Glycohemoglobin Study Program), and the mean HbA1c level was considered [12].
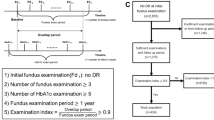
Ophthalmic examinations
Patients were examined by the same ophthalmologist, who knew nothing of the patients’ metabolic control. The fundus was examined using direct and indirect ophthalmoscopy after inducing pupillary dilation, then two-field stereoscopic retinal photographs (50°) were taken according to a standard protocol [20]. Retinal lesions were classified as mild, moderate or severe nonproliferative DR, the key lesions being at least two microaneurysms and/or dot hemorrhages in each eye (mild); venous dilations and/or beading (moderate); and more than 20 microaneurysms and/or dot hemorrhages in four quadrants or venous beading in two quadrants or intraretinal microvascular abnormalities in one quadrant (severe). Proliferative diabetic retinopathy was defined as neovascularization of the optic disk or elsewhere, preretinal hemorrhage, or vitreous hemorrhage [21].
Statistical analysis
Descriptive statistics are given as means and standard deviations. Normality of distribution was tested by calculating skew and kurtosis values. In this cross-sectional study, two logistic regression analyses were performed to assess the impact of different risk factors on DR: In the univariate analysis, a model was constructed using duration of disease, type of therapy, HbA1c levels and glucose variability indicators as independent variables. Since variability indicators correlate closely with one another and with SD-BG ROC [16], a collinearity analysis had to be performed, after which only SD-BG ROC and CONGA 2 remained statistically significant. Based on said univariate and collinearity analyses, a multivariate logistic regression analysis was conducted to identify independent risk factors for DR. The small size of our sample made it impossible to conduct the statistical analysis separately for DM1 and DM2 patients.
Statistical significance was assumed for a p < 0.05. Other statistics were obtained using the unpaired t test. The statistical analyses were completed with the Stata/SE 11.0 software for Windows (StataCorp LP, Texas, USA).
Results
Table 1 shows the baseline clinical characteristics of the 68 DM1 and DM2 patients who underwent CGM. By comparison with patients with no retinopathy, those with DR had longer-standing diabetes, they were more frequently on insulin therapy, and they had a worse glycemic control, though the difference in mean HbA1c levels was not statistically significant (p = 0.06). No differences were observed between the two groups (with and without DR) as regards the prevalence of hypertension and hypercholesterolemia.
The clinical features of the DM1 and DM2 patients are briefly compared in Table 2: DM2 patients were older and had a higher BMI, while the two groups’ HbA1c values did not differ statistically. All the glucose variability indicators considered were significantly higher in DM1 patients (all p values < 0.0001), who carried a more than twofold risk of severe hyperglycemia by comparison with DM2 patients, as shown by comparing the HBGI. None of the patients had history of coronary hearth disease. The two groups were comparable with regard to micro–macroangiopathy.
In particular, the prevalence of DR was 43 % among the DM1 patients and 39 % for the DM2 group (p value n.s.), findings comparable with the prevalence of DR recorded in clinically matched diabetic populations recently studied in two large trials [22, 23]. Almost 90 % of the pathological fundus examinations revealed a nonproliferative DR in patients with both types of diabetes, which was mild in 40 %, moderate in 35 % and severe in 5 % (data not shown).
Univariate analysis (Table 3) showed a significant association between DR and duration of diabetes (OR 1.1; CI. 1.04–1.19), insulin treatment (OR 5.6; CI. 1.14–27.30), AG (OR 1.02; CI. 1.00–1.02), SD-BG ROC (OR 1.03; CI. 1.01–1.06), CONGA 2 (OR 1.02; CI. 1.00–1.04) and HBGI (OR 1.1; CI. 1.01–1.18), whereas no significant association emerged with MAGE, and the association with HbA1c only reached borderline significance. After an appropriate collinearity analysis between the glucose variability indicators and AG, multivariate regression analysis (Table 3) showed that duration of diabetes was the only parameter independently associated with a higher risk of DR in our population.
Discussion
The aim of this cross-sectional study was to analyze the association between glucose variability (as assessed by 72-h CGM) and DR in patients with diabetes mellitus.
Our findings confirm that the duration of the disease is the most relevant risk factor for the onset and progression of DR, as Hammes et al. [22] recently reported. Glucose variability also seemed to have a role in the prevalence of DR, but its significance was lost in multivariate analysis. This finding supports the recent growing interest in studying the effect of glucose variability on the onset of micro- and macrovascular diabetic complications.
While a high glucose variability in DM1 is due mainly to the lack of basal insulin secretion by the beta cells and to intensive insulin therapy [24], glucose fluctuations in DM2 have recently been linked to a much more complex mechanism. The glucotoxicity and lipotoxicity that often precede sustained hyperglycemia can damage early beta cell function [25]. A CGM study by Kohnert et al. [26] on DM2 patients showed that this early beta cell dysfunction develops into a high glucose variability. By triggering oxidative stress, short-lived hyperglycemic spikes can contribute to the progression of DR in both DM1 and DM2 patients, irrespective of any sustained hyperglycemia [7]. So, although HbA1c is the strongest marker of DR risk, it is probably not a comprehensive predictor of DR progression [27]. Consistently with this hypothesis, the HbA1c values in our study only showed a borderline association with DR, even though patients with retinopathy generally had a worse glycemic control. On the other hand, the lack of any association between glucose variability and DR in the multivariate model could be attributable to the high percentage of patients on insulin therapy in our sample. As neatly explained by Monnier et al. [28], exogenous insulin may exert an inhibitory effect on the activation of the pathways involved in oxidative stress, dampening the effect of this co-responsible key factor underlying microvascular injury.
All studies on glucose variability and DR in search of a cause–effect relationship have been based on data from seven-point SMBG profiles [29] or standard deviations obtained from periodic measurements of fasting or post-prandial plasma glucose [30, 31].
It has now been fairly well established that seven-point glucose profiles do not fully reflect real changes in diabetic patients’ blood glucose levels; measuring glucose variability with CGM has proved more accurate [32, 33].
To our knowledge, this is the first study to have examined the association between CGM-assessed glucose variability and the risk of DR. Among the dozens of possible indicators, we chose those capable of specifically describing rapid blood glucose fluctuations and short-lived hyperglycemic spikes, some of which have been strongly and positively correlated with biochemical markers of oxidative stress [34], while others accurately define and quantify the time course of hypo–hyperglycemic fluctuations, especially for hyperglycemic spikes [19].
As mentioned earlier, the very good accuracy of the CGM device used in this study adds to the clinical validity of our results, which can theoretically be extended to a much larger population because our patients had already been included in the ADAG database and consequently followed a standardized multicenter protocol.
The most obvious limitation of this study is the cross-sectional statistical analysis, which does not allow for any assessment of the temporal/causal sequence of events (though this was not the initial aim of the study). Then there is the small sample size, which may also explain the borderline correlation between HbA1c and the prevalence of DR.
Another possible limitation concerns the heterogeneity of the patients involved (cases of DM1 and DM2), but while these diseases are distinct from the pathophysiological and clinical viewpoints, when it comes to glucose variability, they share the same mechanisms of hyperglycemia-induced mitochondrial superoxide production, leading to the epigenetic changes hypothesized to explain the “glycemic memory” phenomenon [35].
In conclusion, despite the above limitations, the present work confirms the pivotal role of the duration of diabetes in determining the progression of DR. We also showed, however, that glucose variability (as expressed by CGM-derived indicators of short-lived glucose fluctuations) is an important part of glycemic control in relation to the prevalence of DR in both DM1 and DM2. Longitudinal trials on large samples of patients, using appropriate measurements of glucose variability obtainable with CGM systems, will be crucially important in future to obtain a definitive picture of the HbA1c-independent role of glucose variability in the onset and progression of DR.
References
Klein BE (2007) Overview of epidemiologic studies of diabetic retinopathy. Ophthalmic Epidemiol 14:179–183
Klein R (2008) Epidemiology of Diabetic Retinopathy. In Duh E (ed.) Diabetic Retinopathy
Cheung N, Mitchell P, Wong TY (2010) Diabetic retinopathy. Lancet 376:124–136
DCCT research group (1993) The effect of intensive treatment of diabetes on development and progression of long-term complications in insulin-dependent diabetes mellitus. N Eng J Med 329:977–986
UK Prospective Diabetes Study group (1998) Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes. Lancet 352:837–853
Lachin JM, Genuth S, Nathan DM, Zinman B, Rutledge BN (2008) Effect of glycemic exposure on the risk of microvascular complications in the diabetes control and complications trial-revisited. Diabetes 57:995–1001
Giacco F, Brownlee M (2010) Oxidative stress and diabetic complications. Circ Res 107:1058–1070
Chang CM, Hsieh CJ, Huang JC, Huang IC (2012) Acute and chronic fluctuations in blood glucose levels can increase oxidative stress in type 2 diabetes mellitus. Acta Diabetol. doi:10.1007/s00592-012-0398-x
Nalysnyk L, Hernandez-Medina M, Krishnarajah G (2010) Glycaemic variability and complications in patients with diabetes mellitus: evidence from a systematic review of the literature. Diabetes Obes Metab 12:288–298
Siegelaar SE, Holleman F, Hoekstra JB, DeVries JH (2010) Glucose variability: does it matter? Endocr Rev 31:171–182
De Block C, Manuel-y-Keenoy B, Van Gaal L (2008) A review of current evidence with continuous glucose monitoring in patients with diabetes. J Diabetes Sci Technol 2:718–727
Hoekstra JB, Nathan DMJ, Borg R, Zheng H, Schoenfeld D, Heine RJ for the A1c-Derived Average Glucose (ADAG) Study Group (2008) Translating the A1C assay into estimated average glucose values. Diabetes Care 31:1473–1478
Sartore G, Chilelli NC, Burlina S, Stefano PD, Piarulli F, Fedele D, Mosca A, Lapolla A (2012) The importance of HbA1c and glucose variability in patients with type 1 and type 2 diabetes: outcome of continuous glucose monitoring (CGM). Acta Diabetol. doi:10.1007/s00592-012-0391-4
Klonoff DC (2005) Continuous glucose monitoring: roadmap for 21st century diabetes therapy. Diabetes Care 28:1231–1239
Ceriello A, Ihnat MA (2010) ‘Glycaemic variability’: a new therapeutic challenge in diabetes and the critical care setting. Diabet Med 27:862–867
Rodbard D (2009) New and improved methods to characterize glycemic variability using continuous glucose monitoring. Diabetes Technol Ther 11:551–565
Service FJ, Molnar GD, Rosevear JW, Ackerman E, Gatewood LC, Taylor WF (1970) Mean amplitude of glycemic excursions, a measure of diabetic instability. Diabetes 19:644–656
McDonnell CM, Donath SM, Vidmar SI, Werther GA, Cameron FJ (2005) A novel approach to continuous glucose analysis utilizing glycemic variation. Diabetes Technol Ther 7:253–263
Kovatchev BP, Cox DJ, Gonder-Frederick LA, Clarke W (2006) Evaluation of a new measure of blood glucose variability in diabetes. Diabetes Care 29:2433–2438
Early Treatment Diabetic Retinopathy Study Research Group (1991) Grading diabetic retinopathy from stereoscopic color fundus photographs—an extension of the modified Arlie house classification. ETDRS report number 10. Ophtalmology 98:786–806
Wilkinson CP, Ferris FL 3rd, Klein RE et al (2003) Proposed international clinical diabetic retinopathy and diabetic macular edema disease severity scales. Ophthalmology 110:1677–1682
Hammes HP, Kerner W, Hofer S, Kordonouri O, Raile K, Holl RW on behalf of the DPV–Wiss Study Group (2011) Diabetic retinopathy in type 1 diabetes—a contemporary analysis of 8,784 patients. Diabetologia 54:1977–1984
Kempen JH, O’ Colmain BJ, Leske MC et al (2004) The prevalence of diabetic retinopathy among adults in the United States. Arch Ophtalmol 122:552–563
Bolli GB, Andreoli AM, Lucidi P (2011) Optimizing the replacement of basal insulin in type 1 diabetes mellitus: no longer an elusive goal in the post-NPH era. Diabetes Technol Ther 13:S43–S52
Stolar M (2010) Glycemic control and complications in type 2 diabetes mellitus. The American Journal of Medicine 123:S3–S11
Kohnert KD, Augstein P, Zander E, Heinke P, Peterson K, Freise EJ et al (2009) Glycemic variability correlates strongly with postprandial β-cell dysfunction in a segment of type 2 diabetic patients using oral hypoglycemic agents. Diabetes Care 32:1058–1062
Lam CSY, Benzie IFF, Choi SW, Chan LYL, Yeung VTF, Woo GC (2011) Relationships among diabetic retinopathy, antioxidants, and glycemic control. Optom Vis Sci 88:251–256
Monnier L, Colette C, Owens D (2012) The glycemic triumvirate and diabetic complications: is the whole greater than the sum of its component parts? Diabetes Res Clin Pract 95:303–311
Kilpatrick ES, Rigby AS, Atkin SL (2009) Effect of glucose variability on the long-term risk of microvascular complications in type 1 diabetes. Diabetes Care 32:1901–1903
Zoppini G, Verlato G, Targer G et al (2008) Is fasting glucose variability a risk factor for retinopathy in people with type 2 diabetes? NMCD 19:334–339
Takao T, Ide T, Yanagisawa H, Kikuchi M, Kawazu S, Matsuyama Y (2011) The effects of fasting plasma glucose variability and time-dependent glycemic control on the long-term risk of retinopathy in type 2 diabetic patients. Diabetes Res Clin Pract 91:e40–e42
Patton SR, Midyett LK, Dolan LM, Powers SW (2011) A comparison of average daily risk range scores for young children with type 1 diabetes mellitus using continuous monitoring and self-monitoring data. Diabetes Technol Ther 14:239–243
Vazeou A (2011) Continuous blood glucose monitoring in diabetes treatment. Diabetes Res Clin Pract 93:S125–S130
Monnier L, Colette C, Owens DR (2008) Glycemic variability: the third component of the dysglycemia in diabetes. Is it important? How to measure it? J Diabetes Sci Technol 2:1094–1100
Ceriello A, Ihnat MA, Thorpe JE (2009) Clinical review 2: the “metabolic memory”: is more than just tight glucose control necessary to prevent diabetic complications? J Clin Endocrinol Metab 94:410–415
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by Massimo Federici.
Rights and permissions
About this article
Cite this article
Sartore, G., Chilelli, N.C., Burlina, S. et al. Association between glucose variability as assessed by continuous glucose monitoring (CGM) and diabetic retinopathy in type 1 and type 2 diabetes. Acta Diabetol 50, 437–442 (2013). https://doi.org/10.1007/s00592-013-0459-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-013-0459-9