Abstract
We wanted to examine proliferative retinopathy as a marker of incident nephropathy in a 25-year follow-up study of a population-based cohort of Danish type 1 diabetic patients and to examine cross-sectional associations between nephropathy and retinopathy in long-term surviving patients of the same cohort. All type 1 diabetic patients from Fyn County, Denmark, were identified as of 1 July 1973. One hundred and eighty four patients were examined in 1981–1982 (baseline) and in 2007–2008 (follow-up). The level of retinopathy was graded by ophthalmoscopy at baseline and nine-field digital colour fundus photographs at follow-up. Single spot urine was used to evaluate nephropathy at both examinations. Proliferative retinopathy was present in 29 patients (15.8%) at baseline. At follow-up, these patients were more likely to macroalbuminuria (20.7% vs. 6.5%) than patients without proliferative retinopathy at baseline. In a multivariate logistic regression adjusted for baseline age, sex, duration of diabetes, smoking, HbA1, systolic and diastolic blood pressure, odds ratio of nephropathy (micro- and macroalbuminuria combined) was 2.98 (95% confidence interval 1.18–7.51, p = 0.02) for patients with proliferative retinopathy at baseline as compared to those without. At follow-up, there was a close relation between retinopathy and nephropathy. The level of macroalbuminuria was 4.3, 4.6 and 13.0% for patients with no or mild non-proliferative retinopathy, moderate non-proliferative retinopathy and proliferative retinopathy, respectively. In conclusion, proliferative retinopathy is an independent marker of long-term nephropathy in type 1 diabetes. Upcoming studies should examine whether these microvascular complications are also causally linked in type 1 diabetes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetic retinopathy and nephropathy are leading causes of blindness and end-stage renal disease in the working-age population of the western world [1]. Retinopathy is almost universal, and nephropathy is found in approximately 40% of all type 1 diabetic patients with a duration of diabetes of more than 25 years [2–4]. Several studies have investigated the relationship between diabetic retinopathy and nephropathy [5, 6], and similarities in the pathogenesis have been described [7].
Nephropathy without retinopathy is not very common as opposed to retinopathy without nephropathy [4, 5, 8]. For instance, in a cross-sectional study of 2,378 type 1 diabetic patients from the EURODIAB IDDM Complications Study it was found that among patients with macroalbuminuria, only 11.5% had no retinopathy [8]. Similar numbers were 60.9 and 44.9% for patients with normo- and microalbuminuria, respectively. Looking at things the other way around, the prevalence of macroalbuminuria was 1.6, 9.0 and 34.0% for patients with no retinopathy, non-proliferative retinopathy (NPDR) and proliferative retinopathy (PDR), respectively.
Even though many cross-sectional studies [4, 5, 8, 9] have examined the association of retinopathy and nephropathy, only a few studies are prospective [10, 11]. Furthermore, long-term studies on the temporal association between retinopathy and nephropathy are lacking. Thus, it has not been described whether proliferative retinopathy is a marker of nephropathy. This is important in order to clarify the pathogenic similarities between these microvascular complications.
Consequently, the aim of this study was to expand on the knowledge of the association between retinopathy and nephropathy in type 1 diabetes. Particularly, we aimed to investigate the influence of proliferative retinopathy on the long-term incidence of nephropathy in a population-based cohort of Danish type 1 diabetic patients.
Subjects, materials and methods
Participants
As previously described [12, 13], insulin prescriptions were used to identify all type 1 diabetic patients living in Fyn County, Denmark, as of 1 July 1973 with an onset before the age of 30 (n = 727). At that time Fyn County approximately had 450,000 inhabitants and was considered a demographically representative 9% sample of Denmark [13]. One hundred and ninety nine patients participated in clinical examinations in both 1981–1982 (baseline) and 2007–2008 (follow-up). Of these, 15 patients already had proteinuria at baseline and were excluded from further analyses. All patients examined at the follow-up gave a written informed consent.
Baseline examination
At baseline, patients underwent a structured interview, and an ophthalmological as well as a clinical examination was performed [12]. Blood pressure was measured by an Erkameter Sphygmomanometer (Morton Medical Ltd, London, UK) on one arm with the patient in sitting position after 10 min of rest. Measurements of the blood included HbA1c made as total Hb-A1 with resin 70 (Bio-Rad, Hercules, CA, USA) at 20°C and pH = 6.70. Urine protein was considered present if greater than or equal to 0.5 g/l protein was found in a spot urine sample. The smoking habits of the patients were noted. Current and ex-smokers were considered to be smokers for the upcoming models. Using tropicamide 1% both pupils were dilated and a slit lamp examination performed (Haag-Streit, Wedel, Germany). Ophthalmoscopy was performed and retinopathy was described and classified by a single trained retinal specialist (AK Sjølie). The patient’s level of retinopathy was determined by the worse eye and classified as no retinopathy, NPDR or PDR. PDR was defined as newly formed vessels or the presence of photocoagulation scars after panretinal photocoagulation.
Registry based data
In order to evaluate renal failure between baseline and the follow-up examination, data were obtained from The Danish National Patient Registry. Renal failure was defined as hospital contacts due to dialysis or renal transplantations. Data on mortality were provided by The Danish Civil Registration System.
Follow-up examination
At follow-up, nephropathy was evaluated in a single spot urine sample. Definitions were the following: normoalbuminuria 0–19 mg/l, microalbuminuria 20–200 mg/l and macroalbuminuria 201 mg/l and above. Pupils were dilated and digital fundus photographs were taken in both eyes. Nine 45° colour fields were captured with Topcon TRC-NW6S (Topcon, Tokyo, Japan) and auto-mosaicked with IMAGEnet (Topcon, Tokyo, Japan). Photographs were graded with a grading protocol [2, 14, 15] according to the Early Treatment Diabetic Retinopathy Study (ETDRS) adaptation of the modified Airlie House classification of diabetic retinopathy [16, 17]. For the upcoming analyses, ETDRS-levels 10–31 were classified as no or mild NPDR, 37–53 as moderate NPDR and 60–85 as PDR. The final category of the patient was determined by the worst eye. All images were graded at the Ocular Epidemiology Research Services, Madison, Wisconsin. Interobserver and intraobserver variations and the validity of the systems have been presented elsewhere [14–16, 18].
The study was approved by the Regional Committee on Biomedical Research Ethics of Southern Denmark.
Statistical analyses
Continuous data are presented as median, and categorical data are presented as per cent. All statistical differences were tested at the 0.05 level. Confidence intervals that do not cross 1.0 were regarded statistically significant. Chi-square tests were used for categorical data, and for continuous data Mann–Whitney test was used to test for differences between two groups.
A multivariate logistic regression was performed to calculate odds ratio for incident nephropathy (micro- or macroalbuminuria) according to the level of PDR at baseline. All patients without proteinuria at baseline who participated at follow-up were considered at risk. Stata Intercooled 9.2 was used for all analyses.
Results
One hundred and ninety nine patients were examined in 1981–1982 and again in 2007–2008. An additional 265 patients were examined at baseline but died prior to the follow-up examination. In general, non-survivors were older, had a longer duration of diabetes, a higher systolic blood pressure, and were more likely to be smokers and to have PDR (Table 1). On the other hand, there was no difference in gender, glycaemic regulation and diastolic blood pressure between patients who participated at the follow-up or died prior to this. Furthermore, there was no statistically significant difference (p = 0.19) between non-survivors (6.8%, 18 of 265) and follow-up participants (4.0%, 8 of 201) in the risk of developing renal failure between baseline and follow-up.
Fifteen patients already had proteinuria at baseline and were thus excluded. Of the 184 patients included in the study, 111 (60.3%) were men and 73 (39.7%) were women. Median age and duration of diabetes at baseline was 33.0 and 16 years, respectively.
At baseline, PDR was present in 29 patients (15.8%). As compared to patients without PDR at baseline, patients with PDR had a longer duration of diabetes (23 vs. 15 years, p < 0.01) (Table 2). There was no statistically significant difference between the groups according to age, sex, smoking, HbA1, systolic or diastolic blood pressure.
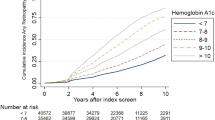
At the follow-up examination, the median age and duration of diabetes was 58.8 and 43 years, respectively, and the number of patients with normo-, micro- and macroalbuminuria was 127 (69.0%), 41 (22.3%) and 16 (8.7%), respectively (Table 3). The level of albuminuria was higher for patients with PDR at baseline (p = 0.04). For instance, macroalbuminuria was present in 20.7 and 6.5% of patients with and without PDR at baseline, respectively. In a multivariate analysis adjusted for baseline-levels of age, sex, duration of diabetes, smoking, HbA1, systolic and diastolic blood pressure, the odds ratio of nephropathy (micro- and macroalbuminuria combined) was 2.98 (95% confidence interval 1.18–7.51, p = 0.02) for patients with baseline PDR as compared to those without.
At the follow-up examination, the level of nephropathy was correlated to the level of retinopathy (p < 0.01) (Table 4). For instance, normoalbuminuria was found in 82.9 and 81.8% of patients with no or mild NPDR, and moderate NPDR, respectively. Patients with PDR, however, were more likely to have albuminuria. Macroalbuminuria was found in 13.0% of patients with PDR, as compared to 4.3 and 4.6% of patients with no or mild NPDR, and moderate NPDR, respectively.
Discussion
Diabetes may lead to various micro- and macrovascular complications [19–22]. A positive association between diabetic retinopathy and nephropathy has been well established in several studies [2, 4–6, 8, 10]. However, this is as far as we know the first long-term prospective study to examine a prospective link between retinopathy and nephropathy in type 1 diabetes. In the present population-based 25-year prospective follow-up study, we found that patients with proliferative retinopathy were three times as likely to develop macroalbuminuria as those without. These findings could not be explained by differences in other possible risk factors for nephropathy and suggest an underlying link between proliferative retinopathy per se and macroalbuminuria in type 1 diabetes.
Brownlee has presented a possible unifying pathogenic mechanism in which the endothelium in retinas capillaries and the mesangial cells in the kidneys glomeruli are both affected [7]. The hyperglycaemia-induced process that leads to tissue damage is caused by an overproduction of superoxide. This leads to oxidative stress and an increased production of reactive oxygen species that causes the damage to the affected cells.
Several studies have found a striking difference in prevalence of retinopathy and nephropathy in type 1 diabetes. Nephropathy rarely occurs without the retinopathy, but retinopathy is often seen in patients without nephropathy [4, 5, 8]. This could be explained by a higher vulnerability of the retina as compared to the kidneys. It is likely that the retina has a greater ability to produce these harmful metabolites as compared to the kidneys, or a reduced ability to repair tissue damage. Another explanation could be that retinal lesions (i.e. microaneurysms) are easier to detect, given that microvasculature is only available for in vivo inspection in the eye. Microalbuminuria reflects a structural damage of the kidneys as compared to retinal microaneurysms which are to some extent reversible. Even though it has been demonstrated that microaneurysms are positively related to progression of retinopathy [23], it has also been found that only 58% of all microaneurysms are still present after 1 year [24]. This reversibility might explain, at least partly, the earlier detection of retinopathy than nephropathy.
Despite the differences in the prevalence rates, several studies have demonstrated a close connection between proteinuria and severe retinopathy [2, 5, 10]. In a 25-year follow-up of the Wisconsin Epidemiological Study of Diabetic Retinopathy, Klein et al. found that the risk of incident PDR was twice as high for patients with microalbuminuria at baseline as in those who had normoalbuminuria [2]. Similar findings were demonstrated in a Spanish follow-up study where the presence of microalbuminuria was a close marker for severe forms of retinopathy (odds ratio 6.31) [10]. Both studies analysed the effect of microalbuminuria as a predictor of proliferative retinopathy, but studies of the reverse relationship are few.
A cross-sectional study from Saudi Arabia found similar results as ours [25]. Thus, the estimated relative risk of nephropathy was 45.5 in patients with PDR compared with patients without retinopathy, suggesting that proliferative retinopathy is a risk indicator for nephropathy. A small Swedish retrospective follow-up study demonstrates results to the contrary. None of the patients with PDR at the baseline developed persistent microalbuminuria within the observation period of 10 years [11]. An interesting aspect of this Swedish study was that all of the patients with PDR at baseline had a diastolic blood pressure under 85 mmHg. Several studies have shown that hypertension is involved in the association between retinopathy and nephropathy [4, 5, 8], which might explain the lack of relationship between retinopathy and nephropathy in the Swedish study.
The major strengths of the current study are the population-based design and the long follow-up. It has been stated in several studies that macroalbuminuria often does not appear during the first 15 years of diabetes [1, 4]. Therefore, a long follow-up and a long duration of diabetes are important to be able accurately to evaluate the long-term effect of retinopathy on nephropathy. The present study also has some limitations. First, survival bias must be considered. All patients at follow-up had survived more than 30 years of diabetes. Since proliferative retinopathy has been proposed as an independent marker of mortality rate among type 1 diabetic patients [26, 27], selective mortality is a concern in the present study. Second, the methods for evaluating retinopathy and proteinuria may lead to inaccuracy. At baseline, retinopathy was evaluated from ophthalmoscopy, which has a lower sensitivity as compared to fundus photographs that are considered the gold standard of today [28]. At both examinations, proteinuria was measured from a single spot urine. The gold standard for evaluating proteinuria is either to use a 24 h collection of urine or to use multiple collections due to the substantial intra-individual and day variability in urinary albumin excretion rate [29]. This was, unfortunately, not possible in the present study.
In conclusion, a close association was found between proliferative diabetic retinopathy and subsequent development of diabetic nephropathy in type 1 diabetic patients. This study suggests that proliferative retinopathy in type 1 diabetic patients may be an independent marker for the long-term incidence of nephropathy. Further studies are needed to examine the applications of this finding.
References
Andersen AR, Christiansen JS, Andersen JK, Kreiner S, Deckert T (1983) Diabetic nephropathy in Type 1 (insulin-dependent) diabetes: an epidemiological study. Diabetologia 25:496–501
Klein R, Knudtson MD, Lee KE, Gangnon R, Klein BE (2008) The Wisconsin Epidemiologic Study of Diabetic Retinopathy: XXII the twenty-five-year progression of retinopathy in persons with type 1 diabetes. Ophthalmology 115:1859–1868
Grauslund J, Green A, Sjolie AK (2009) Prevalence and 25 year incidence of proliferative retinopathy among Danish type 1 diabetic patients. Diabetologia 52:1829–1835
Johansen J, Sjolie AK, Elbol P, Eshoj O (1994) The relation between retinopathy and albumin excretion rate in insulin-dependent diabetes mellitus. From the Funen County Epidemiology of Type 1 Diabetes Complications Survey. Acta Ophthalmol (Copenh) 72:347–351
Cruickshanks KJ, Ritter LL, Klein R, Moss SE (1993) The association of microalbuminuria with diabetic retinopathy. The Wisconsin Epidemiologic Study of Diabetic Retinopathy. Ophthalmology 100:862–867
Kofoed-Enevoldsen A, Jensen T, Borch-Johnsen K, Deckert T (1987) Incidence of retinopathy in type I (insulin-dependent) diabetes: association with clinical nephropathy. J Diabet Complicat 1:96–99
Brownlee M (2005) The pathobiology of diabetic complications: a unifying mechanism. Diabetes 54:1615–1625
Stephenson JM, Fuller JH, Viberti GC, Sjolie AK, Navalesi R (1995) Blood pressure, retinopathy and urinary albumin excretion in IDDM: the EURODIAB IDDM Complications Study. Diabetologia 38:599–603
Jerneld B, Algvere P (1987) Proteinuria and blood glucose levels in a population with diabetic retinopathy. Am J Ophthalmol 104:283–289
Romero P, Salvat M, Fernandez J, Baget M, Martinez I (2007) Renal and retinal microangiopathy after 15 years of follow-up study in a sample of Type 1 diabetes mellitus patients. J Diabetes Complicat 21:93–100
Lovestam-Adrian M, Agardh E, Agardh CD (1998) The incidence of nephropathy in type 1 diabetic patients with proliferative retinopathy: a 10 year follow-up study. Diabetes Res Clin Pract 39:11–17
Sjolie AK (1985) Ocular complications in insulin treated diabetes mellitus. An epidemiological study. Acta Ophthalmol Suppl 172:1–77
Green A, Hauge M, Holm NV, Rasch LL (1981) Epidemiological studies of diabetes mellitus in Denmark. II. A prevalence study based on insulin prescriptions. Diabetologia 20:468–470
Klein R, Klein BE, Moss SE, Davis MD, DeMets DL (1989) The Wisconsin Epidemiologic Study of Diabetic Retinopathy. IX. Four-year incidence and progression of diabetic retinopathy when age at diagnosis is less than 30 years. Arch Ophthalmol 107:237–243
Klein R, Klein BE, Magli YL, Brothers RJ, Meuer SM, Moss SE, Davis MD (1986) An alternative method of grading diabetic retinopathy. Ophthalmology 93:1183–1187
Grading diabetic retinopathy from stereoscopic color fundus photographs–an extension of the modified Airlie House classification. ETDRS report number 10. Early treatment diabetic retinopathy study research group. Ophthalmology 98:786–806
Fundus photographic risk factors for progression of diabetic retinopathy. ETDRS report number 12. Early treatment diabetic retinopathy study research group. Ophthalmology 98:823–833
Klein BE, Davis MD, Segal P, Long JA, Harris WA, Haug GA, Magli YL, Syrjala S (1984) Diabetic retinopathy. Assessment of severity and progression. Ophthalmology 91:10–17
Miyamoto M, Kotani K, Okada K, Fujii Y, Konno K, Ishibashi S, Taniguchi N (2011) The correlation of common carotid arterial diameter with atherosclerosis and diabetic retinopathy in patients with type 2 diabetes mellitus. Acta Diabetol [Epub ahead of print]
Kim BY, Jung CH, Mok JO, Kang SK, Kim CH (2011) Association between serum C-peptide levels and chronic microvascular complications in Korean type 2 diabetic patients. Acta Diabetol [Epub ahead of print]
Ciardullo AV, Daghio MM, Bevini M, Feltri G, Novi D, Fattori G, Borsari S, Donato CD (2010) Joint and distinct risk factors associated with micro- and macrovascular complications in a cohort of type 2 diabetic patients cared through disease management. Acta Diabetol 47:301–308
Tarallo S, Beltramo E, Berrone E, Dentelli P, Porta M (2010) Effects of high glucose and thiamine on the balance between matrix metalloproteinases and their tissue inhibitors in vascular cells. Acta Diabetol 47:105–111
Klein R, Meuer SM, Moss SE, Klein BE (1989) The relationship of retinal microaneurysm counts to the 4 year progression of diabetic retinopathy. Arch Ophthalmol 107:1780–1785
Hellstedt T, Immonen I (1996) Disappearance and formation rates of microaneurysms in early diabetic retinopathy. Br J Ophthalmol 80:135–139
El-Asrar AM, Al-Rubeaan KA, Al-Amro SA, Moharram OA, Kangave D (2001) Retinopathy as a predictor of other diabetic complications. Int Ophthalmol 24:1–11
van Hecke MV, Dekker JM, Stehouwer CD, Polak BC, Fuller JH, Sjolie AK, Kofinis A, Rottiers R, Porta M, Chaturvedi N (2005) Diabetic retinopathy is associated with mortality and cardiovascular disease incidence: the EURODIAB prospective complications study. Diabetes Care 28:1383–1389
Grauslund J, Green A, Sjolie AK (2008) Proliferative retinopathy and proteinuria predict mortality rate in type 1 diabetic patients from Fyn County, Denmark. Diabetologia 51:583–588
Lin DY, Blumenkranz MS, Brothers RJ, Grosvenor DM (2002) The sensitivity and specificity of single-field nonmydriatic monochromatic digital fundus photography with remote image interpretation for diabetic retinopathy screening: a comparison with ophthalmoscopy and standardized mydriatic color photography. Am J Ophthalmol 134:204–213
Klein R, Klein BE, Moss SE (1991) The incidence of gross proteinuria in people with insulin-dependent diabetes mellitus. Arch Intern Med 151:1344–1348
Acknowledgments
This work was supported by grants from Velux Foundation, The Danish Eye Health Society, Sehested Hansen’s Foundation, Danish Diabetes Association, Synoptik Foundation, The A. P. Møller Foundation for the Advancement of Medical Science and Institute of Clinical Research at University of Southern Denmark.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Karlberg, C., Falk, C., Green, A. et al. Proliferative retinopathy predicts nephropathy: a 25-year follow-up study of type 1 diabetic patients. Acta Diabetol 49, 263–268 (2012). https://doi.org/10.1007/s00592-011-0304-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-011-0304-y