Abstract
The aim of this study is to determine safe fasting plasma glucose (FPG) levels. We included data on 5,960 individuals aged ≥20 years at baseline with at least one follow-up examination. Diabetes was ascertained in accordance with American Diabetes Association criteria, using standard 2-h post-challenge plasma glucose test. Multivariate restricted cubic splines Weibull regression was implemented for interval-censored survival data on incident diabetes. We used Harrell’s C statistic for discrimination, Nam-D’Agostino χ2 for calibration, and Royston’s R 2 for variations in the outcome explained by models. During a 6-year median follow-up, 369 incident cases of diabetes were ascertained. Family history of diabetes, systolic blood pressure, waist-to-height ratio, and triglyceride-to-high-density lipoprotein cholesterol ratio, independent of FPG and each other remained associated with incident diabetes. The cubic splines model achieved good calibration (χ2 = 12.1) and discrimination (C = 0.828) and explained 75% of variation in the time until incident diabetes. A J-shaped FPG-diabetes relationship was observed. Descending arm of the dose–response relationship curve corresponded to increasing FPG levels up to 4.0 mmol l−1, where it started increasing. The risk of incident diabetes decreased with decreasing levels of FPG down to 4.0 mmol l−1, where the risk stopped decreasing. Multivariate-adjusted risk of incident diabetes was zero at FPG = 5.05 mmol l−1. Although currently there is no firm evidence to show that early intervention among individuals with the elevated FPG levels could prevent or delay onset of diabetes, individuals with FPG levels below 5.05 mmol l−1 could be safely reassured about their near-term risk of developing incident diabetes and screened on a less frequent basis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
International Diabetes Federation estimated that by 2025 330 million people will have diabetes [1]. Clinical trials have shown that diabetes, in high-risk individuals, can be prevented or the onset delayed by lifestyle modifications [2]. Such promising finding, in the light of the steadily increasing prevalence of diabetes, underpinned the shifting of care for diabetes from secondary to primary prevention [3]. Lifestyle modification programs may entail substantial costs and medication interventions incur costs and may cause harm, which may outweigh benefits when these interventions are applied to individuals at relatively low risk for diabetes [4]. Diabetes-related complications have been shown to begin in the prediabetes estate [5–8], which refers to impaired fasting glycemia (IFG) and impaired glucose tolerance (IGT) [9]. Recently, it has been shown that fasting plasma glucose (FPG) levels below IFG threshold could still confer risk of developing diabetes [10–12]. Increasing insulin resistance and progressive β-cell failure result in nondiabetic glycemia that could eventually escalate to diabetes [9].
The diagnosis of prediabetes has been made based on the glucose criteria, namely categories of IFG and IGT. The adequacy of cutoff points for establishing diagnosis of IFG has been subject of considerable discussions, recently [13, 14]. “To the best of our knowledge, there is no consensus on an FPG threshold below which risk of progressing to diabetes is small enough to practically ignore.” It has been reported that the risk of cardiovascular diseases (CVD) as well as incident diabetes maintains a linear association with glycemia well below the present diagnostic thresholds for diabetes. It may further extend to lower glucose levels than those defined by IFG or IGT into a range of glucose otherwise considered normal [14]. These observations have given rise to the question of whether any individual FPG cut point must be considered as being somewhere in a continuum of hyperglycemia or there is a cutoff point below which one could safely be reassured about his/her risk of developing diabetes in the future.
Using new statistical method, we investigated the nonlinear contribution of FPG to the risk of incident diabetes in order to determine the safe levels of FPG. This approach allowed us to determine an FPG level at which the risk of incident diabetes show a step increase. This cutoff point is where further decreases in FPG levels are unlikely to reduce risk of incident diabetes. We provided a model to reconcile our findings and those of others.
Methods
Study population
Tehran Lipid and Glucose Study (TLGS) is a prospective population-based study performed on a representative sample of the Tehran population, with the aim of determining the prevalence of noncommunicable disease risk factors and developing a healthy lifestyle to improve them [15]. The baseline survey was performed from February 1999 to July 2001 (the first examination). After this cross-sectional phase, individuals were assigned to a prospective study with follow-up examinations on a triennial basis. For the current analysis, we used the data from 10,368 individuals older than 20 years of age attending the baseline examination. Participants with prevalent diabetes (n = 1,164), and those whose diabetes status could not be ascertained (n = 989), or those with missing data on potential predictors (n = 94) were excluded consecutively. After these exclusions, there were 8,121 participants free of diabetic at baseline. In the current analyses, we included data on 5,960 (3,438 women) individuals who attended at least one of the two follow-up examinations, one from September 2001 to August 2005 (the second examination) and the other from April 2005 to March 2008 (the third examination) (Appendix Figure A1).
Clinical and laboratory measurements
A trained interviewer collected information using a pretested questionnaire. The information obtained included demographic data, family history of diabetes, and drug use. Two measurements of systolic blood pressure (SBP) and diastolic blood pressure (DBP) were taken using a standardized mercury sphygmomanometer on the right arm, after a 15-min rest in a sitting position; mean of the two measurements was considered as the individuals’ blood pressure. Weight was measured, with participants minimally clothed without shoes, using digital scales (Seca 707: range 0.1–150 kg) and recorded to the nearest 100 g. Height was measured in a standing position without shoes, using tape meter while shoulders were in a normal alignment. Waist circumference (WC) was measured at the umbilical level. Waist-to-hip ratio (WHpR) was calculated as waist circumference (WC) divided by hip circumference (HC), and WHtR was calculated as WC divided by height. The standard 2-h post-challenge plasma glucose (2-h PCPG) including fasting plasma glucose (FPG) was performed for all participants older than 20 years of age, not on antidiabetic drugs. Plasma glucose level, serum high-density lipoprotein cholesterol (HDL-C) levels, and serum triglycerides (TGs) levels were measured by using previously reported methods. TG/HDL-C was calculated by dividing TG by HDL-C [15].
Definition of terms
Positive family history of diabetes was defined as having at least one parent or sibling with diabetes. Participants were classified as having diabetes at the baseline or during follow-up if they met at least one of these criteria: FPG ≥ 7 mmol l−1, or 2-h PCPG ≥ 11.1 mmol l−1 or taking antidiabetic medication. Impaired glucose tolerance (IGT) was assigned in accordance with the definition provided by American Diabetes Association, i.e., FPG < 7.0 mmol l−1 and 2-h PCPG 7.8–11.0 mmol l−1 [16].
Statistics
Data are reported as mean (SD) or frequency (%) for continuously and categorically distributed variables, respectively. TG/HDL-C ratios were naturally logarithmically transformed to improve the fitness of models. We used the generalized linear model to test the statistical significance of trends across FPG quintiles.
Multivariable models and estimation of diabetes risk function
Weibull proportional hazard regression models were developed for interval-censored survival data, since the precise date of developing diabetes could not be determined and the TLGS records provided only an interval for each diabetes diagnosis. Age, family history of diabetes, SBP, WHtR, and TG/HDL-C ratio were considered as potential cofounders of the association between FPG and incident diabetes [10]. Instead of using arbitrary predetermined cut points, we used multivariate restricted cubic splines, with four knots defined at 5th, 25th, 75th, and 95th percentiles. It is unlikely that moving the knots would have had a major impact on the conclusions [17]. Splines functions, as phrased by Harrell, are “piecewise polynomials within the intervals of a variable that are connected across different intervals of that variable [17].” This flexible approach guarantees that both nonlinear and linear trends are well captured [17]. In variable selection, we dropped a variable if its removal causes a nonsignificant increase in deviance. We set the significance levels for covariate selection by backward elimination at 0.1. For FPG, however, we set the significance level at unity, forcing it into the model, leaving others to be selected or not.
Assessment of model performance
To compare the overall predictive values of linear term only and cubic splines models, we used deviance (D statistic) as measure of goodness of fit, Akaike information criterion (AIC) as a measure of bias-variance trade-off [18], Harrell’s C statistic as a measure of discrimination [17], Nam and D’Agostino χ2 as a measure of calibration [19], and Royston’s R 2 as an Index of Determination or Explained variation [20].
Using Brier score, we compared the predictive performances of the suggested FPG cutoff point and IGT. The Brier score is an aggregate measure of disagreement between the observed outcome and a prediction. A perfect prediction rule would have a Brier score of zero. Spiegel halter’s z statistic was calculated for testing whether an individual Brier score is low enough [21].
We certify that all applicable institutional and governmental regulations, concerning the ethical use of human volunteers, were followed during this research. Informed written consent was obtained from all participants and the Ethical Committee of Research Institute for Endocrine Sciences approved this study. We set the statistical significance level at a two-tailed type I error of 0.05. All statistical analyses were performed using STATA version 11.0 (STATA, College Station, Texas, USA).
Results
The mean age of the study population was 42 years at enrollment, and the mean FPG level was 4.99 mmol l−1. During a median follow-up of 6 years, 369 incident cases of diabetes were ascertained. Age-adjusted annual incidence rate per 1,000 individual was 10.62 (95% CIs 10.50–10.74). Table 1 presents baseline characteristics of study population according to quintiles of FPG. All risk factors increased in stepwise fashion across FPG quintiles, excluding family history of diabetes (P values <0.001). Incidence rates of diabetes across three first FPG quintiles were alike, and trivial increases observed were not statistically significant (P values >0.20). The steepness of slopes, however, dramatically increased for the 4th and 5th quintile (P values <0.001). Sex was not significantly associated with risk of incident diabetes, the analyses, therefore, performed on a sex-pooled sample.
In univariate analysis, continuous FPG levels showed a J-shaped association with incident diabetes (data not shown). When we introduced quintiles FPG, in both univariate and multivariate model, we observed step increases in risk of incident diabetes in 4th quintile (FPG ≥ 5.05 mmol l−1). In univariate model, HRs of the 2nd through 5th quintiles, as compared to the 1st quintile, were 1.09 (95% CIs 0.61–1.97), 1.33 (95% CIs 0.74–2.39), 3.27 (95% CIs 2.00–5.32), and 11.41 (95% CIs 7.26–17.96), respectively. In multivariate analyses, family history of diabetes, SBP, WHtR, and TG/HDL-C remained, independent of FPG and each other, associated with risk of incident diabetes. We retained age in the linear term-only survival model, since it improved the calibration of the model. The HRs of the 2nd through 5th quintiles as compared to the 1st quintile were 1.11 (95% CIs 0.61–2.01), 1.25 (95% CIs 0.69–2.26), 2.81 (95% CIs 1.71–4.64), and 8.55 (95% CIs 5.36–13.64), respectively.
The Harrell’s C (95% CIs), Nam-D’Agostino χ2 (P value), Royston’s R 2 (95% CIs), AIC, and deviance for linear terms-only model were 0.828 (0.808–0.849), 12.1 (0.206), 0.74 (95% CIs 0.69–0.79), 5,687, and 5,675, respectively. The corresponding figures for cubic splines model were 0.833 (0.812–0.854), 8.5 (0.476), 0.75 (95% CIs 0.70–0.81), 5,673, and 5,653, respectively. Difference in deviance (21.7) was significant (P = 0.0002). The cubic splines model outperformed the linear terms-only model, in terms of bias-variance trade-off as indicated by smaller deviance and smaller AIC. Both models achieved good calibration and discrimination. The linear term-only survival model explained 0.74 (95% CIs 0.69–0.79) of variance in the time until incident diabetes. The very similar corresponding figure for the restricted cubic splines survival model was 0.75 (95% CIs 0.70–0.81). The point estimates are almost identical, and the confidence intervals are moderately wide; therefore, statistical significance of a difference is very unlikely (Appendix Table A1).
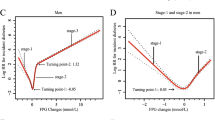
Figure 1 depicts the dose–response relationship between risk of incident diabetes and FPG levels. A J-shaped relationship was observed between FPG levels and 6-year risk of developing incident diabetes. Risk of incident diabetes decreased monotonously as FPG levels decreased down to the FPG level of approximately 4.0 mmol l−1. The log-HR of incident diabetes for FPG level of 5.05 mmol l−1 was zero. The decreasing trend in the risk of diabetes along with decreasing levels of FPG leveled off at 4.0 mmol l−1.
Among incident case of diabetes, we observed higher annual increase in FPG levels among those who had baseline FPG levels above the cutoff point (0.65 mmol l−1, 95% CIs 0.53–0.67) than those with baseline FPG levels below the cutoff point (0.44 mmol l−1, 95% CIs 0.31–0.57).
Among participants with IGT, 71.4% had FPG levels above 5.05 mmol l−1. IGT showed sensitivity (%) of 55.6 (95% CIs 50.3–60.7) and specificity (%) of 89.1 (95% CIs 88.3–89.9) for predicting incident diabetes. The corresponding figures for the FPG cutoff point were 82.1 (95% CIs 77.8–85.9) and 58.3 (95% CIs 57.0–59.6). Prognostic performance of the new FPG cutoff point based on the AROC and Brier score were similar to IGT. AROC was 0.70 (95% CIs 0.68–0.72) for FPG cutoff point and 0.72 (95% CIs 0.70–0.75) for IGT (P = 0.154). Brier score was 0.056 (P for lack of fit = 0.758) for the new FPG cutoff point and 0.052 for IGT (P for lack of fit = 0.756). Negative predictive value was higher for the new FPG cutoff point (Appendix Table A2).
Discussion
It cannot be more emphasized that the current study is not concerned as much with cut point for risk of developing incident diabetes as is with forecasting not developing diabetes. We implemented an appropriate comprehensive statistical analysis on a data set derived from a large population-based prospective study. Using restricted cubic splines model, a J-shaped relationship was observed between FPG levels and 6-year risk of developing incident diabetes. As FPG decreased, a decreasing monotonic dose–response relationship was observed between FPG levels and risk of incident diabetes, with the risk falling below zero for values lower than 5.05 mmol l−1 (91 mg dl−1). The risk decreased monotonously thereafter down to the FPG level of approximately 4.0 mmol l−1.
More than 85% of the study population had FPG levels below 5.6 mmol l−1. This provided a unique opportunity to investigate the influence of FPG levels on risk of incident diabetes among individuals with FPG levels below IFG threshold. We observed that individuals with FPG levels below 5.05 mmol l−1 are very unlikely to develop diabetes within 6 years. Among currently proposed cut points, we believe that 5.05 mmol l−1 should be considered as the cutoff point and individuals with FPG levels below this cutoff point could be reassured about their near-term risk of incident diabetes. This approach can reduce, by half, the costs of screening for incident diabetes among these individuals, which would be expected if they were to be screened based on the currently recommended triennial examination [16]. Using suggested FPG cutoff point will decrease the number of individuals needing further assessment to less than 18% (sensitivity of 82%). One may find it expected for individuals with FPG levels closer to the diabetes diagnostic threshold to develop diabetes sooner than those with lower FPG levels. It is noteworthy that the course of progression to diabetes was more expeditious among those who had baseline FPG levels above the cutoff point than those with baseline FPG levels below the cutoff point. In fact, the former not only were at shorter distances from diabetes but also passed the distance on an accelerated speed. Our finding give support to the notion that hyperglycemia evolves as step rather than gradually over time. Existence of such a line of departure has been shown previously [22].
Meanwhile, we provided a document to suggest that even among those with FPG <6.1 or even 5.6 mmol l−1, there are individuals who might be inadvertently be reassured about their risk of developing incident diabetes. It is, thus, important to raise the awareness among these individuals and their health care providers of the deleterious impacts of the elevated FPG levels. Beneficial effects of intervention measures to prevent or delay onset of diabetes has mainly been shown among those with IGT [23, 24]. Considering that among individuals with IGT, more than 70% had FPG levels above 5.05 mmol l−1, an intensive lifestyle intervention may also be beneficial in preventing or delaying onset of diabetes in individuals with elevated PFG based on the new limit [25]. Our proposed cutoff point had the same discrimination capacity as IGT. With respect to the predictive performance, new FPG cutoff point would keep pace with IGT as was indicated by similar Brier score. The cutoff point suggested here achieved higher sensitivity and higher negative predictive value than did IGT. Nonetheless, overindulging on comparisons of the elevated FPG with IGT is less clinically relevant because, in clinical practice, risk prediction will usually occur using only the FPG without knowledge of the 2-h PCPG. Instead, what is important is the shape of the risk curve relating levels of FPG to the future risk of incident diabetes [26].
In a small case–cohort study of 589 European persons– spline regression with adjustment for age, sex, body mass index, waist circumference, education, physical activity, alcohol consumption, and plasma levels of triglycerides, high-density lipoprotein cholesterol, and γ-glutamyltransferase indicated that FPG was associated with risk in a nonlinear fashion. Risk with higher FPG increased only above ∼84 mg dl−1, the cutoff that would classify the vast majority of the population as at risk and had low sensitivity and specificity [27].
Schriger et al. [13] argued that most of the individuals with elevated FPG levels can be motivated to lose weight and exercise by citing the general benefits of these activities and by pointing to any hypertension, obesity, or dyslipidemia the individual may have. We observed, however, that the risk conferred by elevated levels of FPG was independent of SBP, WHtR, and TG/HDL-C. More than 40% of the population had FPG levels above the cutoff point. It has been postulated that by lowering the cutoff point, we might inadvertently made the elevated FPG so common that people feel it can not be important, since everyone has it and consequently ignore the dietary and exercise recommendations [13]. Practically, there is an important opposing example indicating that increasing trend in obesity has recently leveled off [28, 29] despite the fact that obesity prevailed among considerable number of population. The same may apply to the elevated levels of FPG.
Lowering the cutoff point below 5.05 mmol l−1 is unlikely to produce much in the way of improved outcomes but may increase the cost of medical care. Some investigators questioned, “If the society can afford the costs of treating elevated FPG levels [13].” This question would give rise to a yet unanswered question of “If the society can afford the costs of not treating elevated FPG.” We appreciate that Scylla and Charybdis situations demand meticulous maneuvers.
The strengths of the TLGS study lies on its prospective design; detailed, uniform, and systematic follow-up assisted by a centralized, computerized database; the use of a well-defined end points (using both FPG and 2-h PCPG to ascertain prevalent and incident diabetes); the follow-up measurements of blood and lifestyle variables by using a standard questionnaire in a single center and laboratory; and the direct measurement of anthropometric measures (rather than self-reported). We took a new statistical approach to define the cutoff point. The American Diabetes Association’s Expert Committee on the Diagnosis and Classification of Diabetes Mellitus recommended the cutoff value for the diagnosis of IFG to be reduced from 6.1 to 5.6 mmol l−1 [16]. The recommendation is mainly based on the predictive value of the FPG to predict diabetes, as measured by the AROC. The ROC analysis gives equal weight for false positive and false negative results. Since the cost of these two errors has not been qualified, it is unclear whether this approach is the ideal one [30]. The ideal method of selecting the lower limit of IFG has been suggested to be the identification of a threshold of FPG at which the risk of developing incident diabetes sharply increases [16]. Data from Mauritius indicate that such a threshold of FPG does not exist for future diabetes [30]. Data from the Pima Indians, however, show that the risk of diabetes does increase markedly at FPG concentrations above 5.7 mmol l−1 [31]. Our findings help reconciles these findings. We observed that the linear term-only and cubic splines model had relatively the same predictive performances. However, an innate short come of models examining linear associations is that they cannot help determining where the patterns of associations change, in general. In this particular case, linear term-only model could not help us determining which FPG level did make risk of incident diabetes stop decreasing. We showed that FPG levels below the cutoff point confer no absolute risk for incident diabetes; meanwhile, we showed that the below this cutoff value individuals with lower levels are more protected than those with higher levels. The descending arm of the J-curve corresponded to the FPG levels that are less commonly observed [32]. Our study sample did not have power to determine the pattern of associations for FPG values below 4.0 mmol l−1. The risk pattern (leveling-off), thus, should be interpreted with caution because of wide confidence intervals. However, clinical implications of our findings might have not been affected, since throughout a 24-h period, blood plasma glucose levels are generally maintained between 4 and 8 mmol l−1 (72 and 144 mg dl−1) [32]. Levels below 4.0 mmol l−1 would best be dealt with respect to hypoglycemia than hyperglycemia.
Our finding, however, has to be interpreted in the light of some limitations. First, glucose levels were measured on one occasion, which is the case in population-based studies. This could potentially cause misclassification of participants’ diabetes status. Second, our finding may not be generalizable to the population of different ethnic origin. Third, sex was not associated with risk of incident diabetes in the TLGS population. Ethnicity can possibly modify the effect of sex on risk of diabetes, whether such an effect modification can displace the cutoff point remains to be determined. Fourth, over 2,000 participants were excluded because they did not have follow-up data. If probability of having follow-up data depended on health outcomes, this could bias the results. However, using propensity score, and thus within its limitations, we have previously shown that such a selection bias might have not affected our results [33]. Fifth, we used only baseline values of covariates some of which might have been subjected to change during follow-up. Regression dilution, however, is a common short come to many longitudinal studies. Sixth, we were unable to distinguish type 1 from type 2 diabetes; however, it is highly likely given the age range of the TLGS’ participants that nearly all had type 2 diabetes [34]. Finally, the mean age of the study sample was 42 years. The results, thus, may not be applicable to older populations.
Conclusion
In conclusion, in nonhypoglycemic range, the relative risk of incident diabetes increases with FPG in linear fashion; the absolute risk, however, seems to be trivial for FPG levels below 5.05 mmol l−1. Although currently there is no firm evidence to show that early intervention among individuals with the elevated FPG levels could prevent or delay onset of diabetes, individuals with FPG levels below 5.05 mmol l−1 could be safely reassured about their near-term risk of developing incident diabetes and screened on a less frequent basis.
References
Unwin N, Gan D, Whiting D (2010) The IDF diabetes atlas: providing evidence, raising awareness and promoting action. Diabetes Res Clin Pract 87:2–3
Harati H, Hadaegh F, Momenan AA, Ghanei L, Bozorgmanesh MR, Ghanbarian A, Mirmiran P, Azizi F (2010) Reduction in incidence of type 2 diabetes by lifestyle intervention in a middle eastern community. Am J Prev Med 38(6):628–636, e621. doi:10.1016/j.amepre.2010.03.003
Goyder EC, McNally PG, Drucquer M, Spiers N, Botha JL (1998) Shifting of care for diabetes from secondary to primary care, 1990–5: review of general practices. BMJ 316(7143):1505–1506
Herman WH (2009) Predicting Risk for diabetes: choosing (or building) the right model. Ann Intern Med 150(11):812–814. doi:10.1059/0003-4819-150-11-200906020-00010
Schaefer C, Biermann T, Schroeder M, Fuhrhop I, Niemeier A, Rüther W, Algenstaedt P, Hansen-Algenstaedt N (2010) Early microvascular complications of prediabetes in mice with impaired glucose tolerance and dyslipidemia. Acta Diabetol 47(Suppl 1):19–27
Atkins RC, Zimmet P (2010) Diabetic kidney disease: act now or pay later. Nephrology 15(1):20–22
Tarquini R, Lazzeri C, Pala L, Rotella CM, Gensini GF (2010) The diabetic cardiomyopathy. Acta Diabetol. doi:10.1007/s00592-010-0180-x
Greco D, Gambina F, Maggio F (2009) Ophthalmoplegia in diabetes mellitus: a retrospective study. Acta Diabetol 46(1):23–26
Nichols GA, Hillier TA, Brown JB (2007) Progression from newly acquired impaired fasting glusose to type 2 diabetes. Diabetes Care 30(2):228–233. doi:10.2337/dc06-1392
Bozorgmanesh M, Hadaegh F, Ghaffari S, Harati H, Azizi F (2010) A simple risk score effectively predicted type 2 diabetes in Iranian adult population: population-based cohort study. Eur J Public Health. doi:10.1093/eurpub/ckq074
Kahn HS, Cheng YJ, Thompson TJ, Imperatore G, Gregg EW (2009) Two risk-scoring systems for predicting incident diabetes mellitus in US adults age 45 to 64 Years. Ann Intern Med 150(11):741–751
Schmidt MI, Duncan BB, Bang H, Pankow JS, Ballantyne CM, Golden SH, Folsom AR, Chambless LE (2005) Identifying individuals at high risk for diabetes: the atherosclerosis risk in communities study. Diabetes Care 28(8):2013–2018
Schriger DL, Lorber B (2004) Lowering the cut point for impaired fasting glucose. Diabetes Care 27(2):592–595. doi:10.2337/diacare.27.2.592
Garber A, Handelsman Y, Einhorn D, Bergman D, Bloomgarden Z, Fonseca V, Timothy Garvey W, Gavin III J, Grunberger G, Horton E (2008) Diagnosis and management of prediabetes in the continuum of hyperglycemia—when do the risks of diabetes begin? A consensus statement from the American College of Endocrinology and the American Association of Clinical Endocrinologists. Endocrine Practice 14(7):933–946
Azizi F, Ghanbarian A, Momenan AA, Hadaegh F, Mirmiran P, Hedayati M, Mehrabi Y, Zahedi-Asl S (2009) Prevention of non-communicable disease in a population in nutrition transition: Tehran lipid and glucose study phase II. Trials 10(1):5. doi:10.1186/1745-6215-10-5
The Expert Committee on the Diagnosis and Classification of Diabetes Mellitus (2003) Follow-up report on the diagnosis of diabetes mellitus. Diabetes Care 26(11):3160–3167. doi:10.2337/diacare.26.11.3160
Harrell FE (2001) Regression modeling strategies. Springer, New York
Akaike H (1974) A new look at the statistical model identification. IEEE Trans Automat Contr AC-19:716–723
D’Agostino RB, Nam BH (2004) Evaluation of the performance of survival analysis models: Discrimination and Calibration measures. In: Balakrishnan N, Rao CR (eds) Handbook of Statistics, Survival Methods, vol 23. Elsevier B.V., Amsterdam, pp 1–25. doi:10.16/S0169-7161(03)23001-7
Royston P (2006) Explained variation for survival models. Stata J 6(1):83–96
Spiegelhalter DJ (1986) Probabilistic prediction in patient management and clinical trials. Stat Med 5(5):421–433
Ferrannini E, Nannipieri M, Williams K, Gonzales C, Haffner SM, Stern MP (2004) Mode of onset of type 2 diabetes from normal or impaired glucose tolerance. Diabetes 53(1):160–165. doi:10.2337/diabetes.53.1.160
Tuomilehto J, Lindstrom J, Eriksson JG, Valle TT, Hamalainen H, Ilanne-Parikka P, Keinanen-Kiukaanniemi S, Laakso M, Louheranta A, Rastas M, Salminen V, Uusitupa M (2001) Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med 344(18):1343–1350
Pan XR, Li GW, Hu YH, Wang JX, Yang WY, An ZX, Hu ZX, Lin J, Xiao JZ, Cao HB, Liu PA, Jiang XG, Jiang YY, Wang JP, Zheng H, Zhang H, Bennett PH, Howard BV (1997) Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance. The Da Qing IGT and diabetes study. Diabetes Care 20(4):537–544. doi:10.2337/diacare.20.4.537
Diabetes Prevention Program Research Group (2002) Reduction in the incidence of Type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 346(6):393–403. doi:10.1056/NEJMoa012512
Forouhi NG, Balkau B, Borch-Johnsen K, Dekker J, Glumer C, Qiao Q, Spijkerman A, Stolk R, Tabac A, Wareham NJ (2006) The threshold for diagnosing impaired fasting glucose: a position statement by the European Diabetes Epidemiology Group. Diabetologia 49(5):822–827. doi:10.1007/s00125-006-0189-4
Schulze MB, Fritsche A, Boeing H, Joost HG (2010) Fasting plasma glucose and type 2 diabetes risk: a non-linear relationship. Diabet Med 27(4):473–476. doi:10.1111/j.1464-5491.2009.02919.x
Sundquist J, Johansson S-E, Sundquist K (2010) Levelling off of prevalence of obesity in the adult population of Sweden between 2000/01 and 2004/05. BMC Public Health 10(1):119
Ogden C, Carroll M, Curtin L, McDowell M, Tabak C, Flegal K (2006) Prevalence of overweight and obesity in the United States, 1999–2004. Jama 295(13):1549
Shaw JE, Zimmet PZ, Hodge AM, de Courten M, Dowse GK, Chitson P, Tuomilehto J, Alberti KG (2000) Impaired fasting glucose: how low should it go? Diabetes Care 23(1):34–39. doi:10.2337/diacare.23.1.34
Gabir MM, Hanson RL, Dabelea D, Imperatore G, Roumain J, Bennett PH, Knowler WC (2000) The 1997 American Diabetes Association and 1999 World Health Organization criteria for hyperglycemia in the diagnosis and prediction of diabetes. Diabetes Care 23(8):1108–1112. doi:10.2337/diacare.23.8.1108
Cryer P (1997) Hypoglycemia: pathophysiology, diagnosis, and treatment. Oxford University Press, USA
Bozorgmanesh M, Hadaegh F, Zabetian A, Azizi F (2010) San Antonio heart study diabetes prediction model applicable to a Middle Eastern population? Tehran glucose and lipid study. Int J Public Health 55(4):315–323. doi:10.1007/s00038-010-0130-y
Pishdad GR (2005) Low incidence of type 1 diabetes in Iran. Diabetes Care 28(4):927–928
Acknowledgments
This study was supported by grant No. 121 from the National Research Council of the Islamic Republic of Iran. We express our appreciation to the participants of district-13 of Tehran for their enthusiastic support in this study. The authors thank Dr. Sarbakhsh, Prevention of Metabolic Disorders Research Center, Research Institute for Endocrine Sciences (RIES), Shahid Beheshti University of Medical Sciences, Tehran, Iran, for her incredible comments.
Conflict of interest
None to disclose.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bozorgmanesh, M., Hadaegh, F., Saadat, N. et al. Fasting glucose cutoff point: where does the risk terminate? Tehran lipid and glucose study. Acta Diabetol 49, 341–348 (2012). https://doi.org/10.1007/s00592-011-0298-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-011-0298-5