Abstract
The role of hyperhomocysteinemia as a risk factor for diabetic long-term complications has not been sufficiently evaluated in prospective studies, considering specific correlates of homocysteine (tHcy) concentration and traditional cardiovascular disease (CVD) risk factors. Fasting tHcy, vitamin B12 and folate plasma levels, the common methylenetetrahydrofolate reductase (MTHFR) C677T gene polymorphism, as well as clinical and lifestyle information were assessed in 216 type 2 diabetic patients attending two outpatient clinics, who had a follow-up evaluation at 65 ± 9 months for the incidence of macroangiopathy. At basal evaluation, mild hyperhomocysteinemia (tHcy ≥ 15 μmol/l) was diagnosed in 21.3% of participants. At follow-up, hyperhomocysteinemia and the distribution of MTHFR C677T genotype did not significantly differ according to the incidence of macroangiopathy. Multiple variables adjusted ORs (95% CI) for CVD associated with mild hyperhomocysteinemia were 1.01 (0.37–2.82); P > 0.05; those associated with MTHFR TT genotype were 0.46 (0.15–1.38); P > 0.05. Although the prevalence of hyperhomocysteinemia was higher in diabetic men (26.9%) than in women (16.1%; P > 0.05), similar results were also observed in a separate sex-analysis. At the multivariate analysis, including in the model other potential CVD risk factors, only creatinine clearance was a significant risk factor for the development of macroangiopathy. In this cohort of diabetic subjects, mild hyperhomocysteinemia and the MTHFR TT genotype are not significant risk factors for the development of macroangiopathy; impaired renal function was confirmed as a significant predictor of this complication.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A moderate increase in total homocysteine (tHcy) plasma levels may contribute to the cardiovascular disease (CVD) risk of type 2 diabetic subjects. However, despite the relationship between tHcy levels and diabetes has been investigated for almost 20 years, the causal role of hyperhomocysteinemia in diabetic long-term complications is still questioned [1–3].
The controversies may partly lie on the cross-sectional design of most of the studies that have investigated these relationships. Furthermore, the vast majority of these studies did not account for potential confounders such as specific predictors of tHcy plasma levels in diabetic subjects [2, 3].
Circulating tHcy derives from the interplay of genetic and environmental factors involved in the homocysteine/methionine metabolic cycle. Ageing and gender, renal function, vitamin B12, B6 and folate, together with lifestyle factors such as smoking [4], as well as a common mutation in the methylenetetrahydrofolate reductase (MTHFR) gene locus [5, 6] are known determinants of tHcy concentration in the general population, and they have been recently reported to account for tHcy variations also in type 2 diabetic subjects [7]. On the contrary, the impact of diabetes-related variables, such as metabolic control, oral hypoglycemic drugs and the degree of insulin resistance on tHcy levels, is still under debate [7–10].
These factors must be taken into account when evaluating whether hyperhomocysteinemia and/or the MTHFR TT genotype would increase the risk of developing diabetic long-term complications.
Consequently, the purpose of this study was to investigate the independent relationships between mild hyperhomocysteinemia, the common MTHFR C677T variant and the incidence of macroangiopathy in a sample of type 2 diabetic subjects, taking into account tHcy determinants specifically individuated in this same population [7], as well as other common CVD risk factors.
Subjects, materials and methods
Study population
Details on the study population have been presented elsewhere [7]. Briefly, unrelated type 2 diabetic patients, attending the outpatient clinics of the Metabolic Units of Messina University Hospital, in Messina and of Chieri Hospital, in Turin, Italy, were consecutively enrolled into the study, after giving their informed consent. Exclusion criteria at enrolment were creatinine values >1.5 mg/dl, macroalbuminuria, medical conditions or medications potentially influencing tHcy levels, as well as invalid measurements or information on the main study parameters.
Of the 312 subjects who participated the baseline evaluation [7], 96 patients did not participate to the follow-up analysis due to impossibility to recall information on 6 patients, death for 11 patients and incomplete data at follow-up for the others. Those (216 subjects) who had a valid follow-up evaluation were considered eligible and included in the present analysis.
No significant baseline demographic and clinical differences were noted between subjects included (n = 216) and those excluded (n = 96) from the present analysis (data not shown); in particular, baseline mean tHcy levels were 13.67 ± 5.25 vs. 12.71 ± 5.94 μmol/l in the excluded vs. the included group, (P > 0.05); similarly, the distribution of MTHFR genotype was not significantly different in the two groups (P > 0.05).
Baseline information relative to personal, clinical and lifestyle data was collected by a questionnaire. Subjects were defined as not smokers or current smokers, including in the latter category also those who had quit within 1 year. Subjects were currently treated with diet, oral agents (OHA), insulin or a combination of these.
All the participants gave their informed consent, and the study was approved by the local ethical committee.
Measurements and assays
Type 2 diabetes was diagnosed according to ADA 1997 criteria [11]. BMI and blood pressure (BP) were measured according to standard procedures. Hypertension was defined as systolic BP > 130 mmHg and/or diastolic BP > 80 mmHg, or current use of antihypertensive medications.
All baseline biochemical variables were measured at study recruitment. Fasting plasma glucose, total cholesterol (T-C), HDL-cholesterol (HDL-C), triglycerides and creatinine were measured with standard automated laboratory methods (Roche Diagnostics, Milan, Italy).
Creatinine clearance (ml/min/1.73 m2) was calculated by the Cockroft and Gault formula, corrected for the body surface area. Hypercholesterolemia was defined as fasting T-C levels ≥ 200 mg/dl or use of medications; hypertriglyceridemia was defined as fasting triglycerides levels ≥ 150 mg/dl or use of medications.
Glycated haemoglobin (HbA1c) was measured using an automated high-performance liquid chromatography (HPLC) analyzer (Diamat; Bio-Rad Laboratories, Milan, Italy); normal range values in our laboratory are 4–6%.
Plasma levels of tHcy and folate/vitamin B12 were assessed by the use of commercially available kit for HPLC measurements (Bio-Rad, Italy) and Simul-TRAC-SNB 125I-RIA (DRG Diagnostics, Germany), respectively.
MTHFR C677T genotyping
All participants were genotyped for the MTHFR C677T polymorphism. Briefly, genomic DNA, extracted from total blood with standard methods, was amplified by polymerase chain reaction (PCR), using the primers specified by Frosst et al. [5]. The PCR products were digested with Hinf I (MspI, MBI Fermentas, Lithuania) restriction enzyme, separated by electrophoresis on agarose gel and visualized in ultraviolet light.
Assessment of macroangiopathy
Macroangiopathy was defined as a composite end-point [12, 13] including documented myocardial infarction, ischaemic heart disease, coronary heart bypass, coronary angioplasty, cerebral thromboembolism and peripheral amputations, or by Minnesota codes 1·1–3, 4·1–4, 5·1–3 at a standard ECG [14].
Statistical analysis
Statistical analysis was performed using the SPSS package, version 13.0. Natural logarithmic transformations were used for positively skewed variables such as tHcy, folate and vitamin B12. In the descriptive analysis, these variables were expressed as geometric means. Univariate inferential statistics were produced by means of the χ2-test for categorical variables and the t-test for continuous measures. One-way ANOVA and GLM were used for univariate unadjusted and multivariate-adjusted analysis, respectively, to investigate possible statistical differences of tHcy, folate and vitamin B12 within the MTHFR genotype categories. The interaction between MTHFR and sex on long-term cardiovascular complications was also investigated.
Univariate and multivariate unconditional logistic regressions were performed to quantify the risk (OR) of developing macroangiopathy based on the presence of mild hyperhomocysteinemia (tHcy ≥ 15 μmol/l) and MTHFR TT genotype. The effect of tHcy increments by 5 μmol/l on complications was ascertained as well.
In the multivariate analysis, the effect of tHcy and genotype was controlled for age, gender, creatinine clearance, vitamin B12, folate, smoking, hypertension, high cholesterol levels, diabetes duration and HbA1c. All statistical comparisons are two-tailed, and they were considered significant at the P < 0.05 level.
Results
Baseline clinical and demographic characteristics of the 216 type 2 diabetic patients attending the two outpatient clinics who completed the follow-up evaluation are given in Table 1. Overall, type 2 diabetic subjects (mean age of 63 years) were obese/overweight with an acceptable metabolic control (mean HbA1c:7.2%) and renal function (creatinine clearance: 82 ml/min/1.73 m2), despite the relatively long duration of the disease (mean 11 years). Overall, 32.4% of subjects were current smokers, 58.6% had hypertension, 25.0 and 17.6%, respectively, had high T-C or high triglycerides values or were under medications for these conditions.
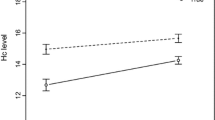
As shown in Table 2, mean baseline tHcy plasma levels were within the normal laboratory range (12.71 ± 5.94 μmol/l), and they were significantly higher in diabetic men than in diabetic women (P = 0.003); conversely, diabetic men had significantly lower concentrations of folate and vitamin B12 when compared to women (P < 0.001, for both comparisons).
The MTHFR C677T genotype distribution did not differ from the frequencies predicted by Hardy–Weinberg equilibrium, and it was comparable between men and women with diabetes, with a TT homozygous frequency of 25% in both groups (Table 2).
Baseline tHcy levels (μmol/l) were [geometric mean and (95% CI)] 11.6 (10.78–12.47) in CC, 11.87 (11.12–12.68) in CT and 12.17 (10.86–13.63) in TT subjects; and folate levels (ng/ml) were 3.8 (3.31–4.36) in CC, 3.43 (2.95–3.89) in CT and 2.96 (2.57–3.38) in TT subjects; these differences were not statistically significant (P > 0.05 for all comparisons); no differences in vitamin B12 concentrations [493.92 (436.51–549.54) pg/ml in CC, 566.72 (512.86–602.55) pg/ml in CT and 541.83 (478.63–608.69) pg/ml in TT subjects] were noted according to genotype. Similar results were also obtained performing a separate sex-analysis (data not shown).
Overall, hyperhomocysteinemia (tHcy ≥ 15 μmol/l) [15] was diagnosed in 21.3% of participants; and its prevalence, as well as that of MTHFR TT genotype, did not significantly differ in diabetic subjects with (n = 10; 4.6%) or without macroangiopathy (n = 206; 95.4%) at baseline evaluation (data not shown).
We evaluated the role of mild hyperhomocysteinemia and the MTHFR variant as risk factors for the development of CVD only in subjects free of that complication at baseline. Over a mean follow-up of 65 ± 9 months, there were 35 (16.5%) incident cases of any CVD (49 new cases per 1,000 person-years).
Baseline hyperhomocysteinemia and the prevalence of MTHFR TT genotype were not associated with macroangiopathy incidence at follow-up, at either univariate or multivariate analysis: the prevalence of hyperhomocysteinemia in those with vs. those without this complication at follow-up was 28.6% vs. 19.9% (P > 0.05). Similarly, TT genotype was present in 17.1% vs. 26.9% (P > 0.05) of those with or without macroangiopathy at follow-up.
Both hyperhomocysteinemia and MTHFR TT genotype were not significant risk factors (OR and 95% CI) for the onset of macrovascular disease, either at univariate or multivariate analysis, after adjusting for major determinants of tHcy levels, specifically identified in this population, as well as for major CVD risk factors (Table 3).
Although the prevalence of hyperhomocysteinemia was higher in men (26.9%) than in women (16.1%; P > 0.05), similar results were also obtained when a separate sex-analysis was performed (Table 3). Furthermore, the test for sex-MTHFR genotype interaction on the risk for macroangiopathy was not significant (P for the interaction term > 0.05)
Moreover, each 5 μmol/l increment of tHcy plasma levels was not associated with an increased risk of macroangiopathy [adjusted ORs (and 95% CI) were 0.77 (0.46–1.31)].
At the multivariate analysis (Table 4), which included in the model baseline values of several potential risk factors, only creatinine clearance [OR (and 95% CI) 0.96 (0.93–0.99)] was a significant risk factor for the development of macroangiopathy in this cohort.
Discussion
In this prospective study of a cohort of outpatient facility type 2 diabetic subjects, we did not find any significant association between high baseline tHcy plasma levels and/or homozygosis for the MTHFR C677T polymorphism and the incidence of macroangiopathy after a ~5 years of follow-up.
In general population, the potential impact of hyperhomocysteinemia and the MTHFR mutation on CVD outcomes has been largely investigated [16], but it is still not clear whether these factors may contribute to increase CVD in high-risk cohorts such as those with diabetes.
In diabetic subjects, mild hyperhomocysteinemia has been variably associated with macrovascular complications.
In one of the first studies, Araki et al. [17] found higher tHcy plasma levels in type 2 diabetic subjects with macroangiopathy than in those without that complications. Furthermore, in the Hoorn Study [1], high circulating tHcy plasma levels were associated with a higher CVD risk in diabetic individuals than in those with impaired or normal glucose tolerance. However, not all the studies were concord with these findings, and other authors failed to show any difference in tHcy concentrations between type 2 diabetic subjects with or without macroangiopathy [18].
In prospective studies, mainly conducted in North European cohorts, hyperhomocysteinemia has been also associated with a higher CVD risk and a higher total mortality [19, 20], although these results were not confirmed by a German study, after taking into account vitamin levels and MTHFR genotype [21].
Thus, despite the numerous studies that have tested the “homocysteine hypothesis”, the causal association between hyperhomocysteinemia and CVD risk is still debated, both in diabetic [2, 3] and in general population [22, 23].
Methodological differences in the assessment of CVD, differences in the baseline characteristics of subjects, and, above all, a different study design may account for the discrepancies between these results.
Part of the controversy in the literature may also lie on the lack of complete information on factors regulating tHcy levels specifically in the setting of diabetes, since these factors may act as potential confounders when evaluating the role of hyperhomocysteinemia in diabetic long-term complications.
Although well-defined in the general population, determinants of tHcy plasma concentration have not been fully elucidated in diabetic subjects, since diabetes-related variables, i.e. insulin resistance, metabolic control and oral hypoglycaemic drugs, may specifically modulate the concentration of this amino acid [7, 10, 24].
In a large cohort of type 2 diabetic subjects, we reported that age, creatinine, folate, vitamin B12 and to a minor extent, sex, smoking, MTHFR TT genotype and systolic BP were significantly associated with circulating tHcy levels, whereas no significant associations were noted with diabetes-related variables [7]. Furthermore, similar to the results reported in the Framingham Offspring cohort [25], a significant sex-MTHFR genotype interaction on tHcy concentration was also noted in diabetic subjects [7].
After accounting for all significant correlates, as well as other major CVD risk factors, the results of the present study conducted on a subset of that same cohort [7] show that hyperhomocysteinemia is not a major risk factor for the development of macroangiopathy, either in men or in women with type 2 diabetes.
The common MTHFR C677T mutation has also been proposed as a genetic risk factor for CVD. In general population, however, it has been reported that the TT genotype is at the most a weak predictor for CVD [6].
Also in diabetic subjects, the MTHFR mutation has been associated, although not consistently [26, 30] with macroangiopathy. However, in accordance with data from Caucasian populations [29, 30], our findings do not support this hypothesis. The lack of significant association of MTHFR mutation with CVD outcomes was also confirmed after conducting a sex-specific analysis, despite sex-genotype interactions with MTHFR polymorphism have been reported both in general [25] and in diabetic populations [7].
Although a different genetic background may partly account for the differences between some of the positive studies [26–28] and our results, the most likely explanation is that MTHFR TT genotype, by modestly increasing tHcy levels, does not influence the natural history of macrovascular complications in type 2 diabetes.
Since a major shortcoming of our study is the relatively small number of incident CVD events at the follow-up evaluation, probably due to the acceptable metabolic and CVD risk factors control of our patients, it cannot be excluded that the association between high tHcy levels, MTHFR TT genotype and macroangiopathy would become significant with a longer follow-up.
However, this is not a likely scenario, since macrovascular complications may be already present at the diagnosis of diabetes, and up to 1/3 of patients remain undiagnosed until long-term complications appear.
Moreover, since our population has been regularly visited in the outpatient facility of our hospitals, it may be not representative of general diabetic population. However, the results of our study, conducted in a typical outpatient clinical setting, are in agreement with the emerging hypothesis that hyperhomocysteinemia is rather a marker than a causal factor associated with CVD [22, 23], an hypothesis that has gained support from the results of recent intervention trials not confirming the beneficial effects of tHcy lowering with B-vitamins on CVD outcomes [31, 32], even in subjects with diabetes [31].
Conversely, we found that renal function, i.e., creatinine clearance, was a significant predictor of the development of macrovascular disease in this population. Serum creatinine and glomerular filtration rate have been conclusively shown to be significant correlates of tHcy levels [4], and we have demonstrated that creatinine clearance is the primary determinant of tHcy levels also in type 2 diabetic patients [7]. Furthermore, a reduced glomerular filtration rate (GFR) has been associated with high CVD morbidity and mortality in the general population and in several cohorts of type 2 diabetic subjects [33, 34].
In conclusion, mild hyperhomocysteinemia and the common MTHFR TT mutation do not predict the incidence of macrovascular complications in a cohort of type 2 diabetic patients, whereas an impaired renal function was confirmed as significant CVD risk factor in this population.
References
Hoogeveen EK, Kostense PJ, Beks PJ, Mackaay AJ, Jakobs C, Bouter LM et al (1998) Hyperhomocysteinemia is associated with an increased risk of cardiovascular disease, especially in non-insulin-dependent diabetes mellitus: a population-based study. Arterioscler Thromb Vasc Biol 18:133–138
Elias AN, Eng S (2005) Homocysteine concentrations in patients with diabetes mellitus—relationship to microvascular and macrovascular disease. Diabetes Obes Metab 7:117–121
Audelin MC, Genest J Jr (2001) Homocysteine and cardiovascular disease in diabetes mellitus. Atherosclerosis 159:497–511
Jacques PF, Bostom AG, Wilson PW, Rich S, Rosenberg IH, Selhub J (2001) Determinants of plasma total homocysteine concentration in the Frammingham Offspring Cohort. Am J Clin Nutr 73:613–621
Frosst P, Blom HJ, Milos R, Goyette P, Sheppard CA, Matthews RG et al (1995) A candidate genetic risk factor for vascular disease: a common mutation at the methylenetetrahydrofolate reductase. Nat Genet 10:111–113
Klerk M, Verhoef P, Clarke R, Blom HJ, Kok FJ, Schouten EG, The MTHFR Studies Collaboration Group (2002) MTHFR 677 CT polymorphism and risk of coronary heart disease. JAMA 288:2023–2031
Russo GT, Di Benedetto A, Giorda C, Alessi E, Crisafulli G, Ientile R et al (2004) Correlates of total homocysteine plasma concentration in type 2 diabetes. Eur J Clin Invest 34:197–204
Passaro A, Calzoni F, Volpato S, Nora ED, Pareschi PL, Zamboni PF et al (2003) Effect of metabolic control on homocysteine levels in type 2 diabetic patients: a 3-year follow-up. J Intern Med 254:264–271
Hoogeven EK, Kostense PJ, Jakobs C (1997) Does metformin increase the serum total homocysteine level in NIDDM? J Int Med 242:389–394
Buysschaert M, Dramais AS, Wallemacq PE, Hermans MP (2000) Hyperhomocysteinemia in type 2 diabetes: relationship to macroangiopathy, nephropathy, and insulin resistance. Diabetes Care 23:1816–1822
The Expert Committee on the Diagnosis of Diabetes Mellitus (1997) Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care 20:1183–1197
Giorda CB, Avogaro A, Maggini M, Lombardo F, Mannucci E, Turco S, Diabetes and Informatics Study Group (2008) Recurrence of cardiovascular events in patients with type 2 diabetes: epidemiology and risk factors. Diabetes Care 31:2154–2159
The DAI Study Group (2004) Prevalence of coronary heart disease in a cohort of type 2 diabetic patients in Italy: the DAI study. Diabet Med 21:738–745
Rose GA, Blackburn H (1968) Cardiovascular survey methods. Monogr Ser World Health Organ 56:1–188
Welch GN, Loscalzo J (1998) Homocysteine and atherothrombosis. N Engl J Med 338:1042–1050
Ueland PM, Refsum H, Beresford SA, Vollset SE (2000) The controversy over homocysteine and cardiovascular risk. Am J Clin Nutr 72:324–332
Araki A, Sako Y, Ito H (1993) Plasma homocysteine concentrations in Japanese patients with non insulin-dependent diabetes mellitus: effect of parenteral methylcobalamin treatment. Atherosclerosis 103:149–157
Chico A, Perez A, Cordoba A, Arcelus R, Carreras G, De Leiva A et al (1998) Plasma homocysteine is related to albumin excretion rate in patients with diabetes mellitus: a new link between diabetic nephropathy and cardiovascular disease? Diabetologia 41:684–693
Hoogeveen EK, Kostense PJ, Jakobs C, Dekker JM, Nijpels G, Heine RJ et al (2000) Hyperhomocysteinemia increases risk of death, especially in type 2 diabetes: 5-year follow-up of the Hoorn study. Circulation 101:1506–1511
Soinio M, Marniemi J, Laakso M, Lehto S, Ronnemaa T (2004) Elevated plasma homocysteine level is an independent predictor of coronary heart disease events in patients with type 2 diabetes mellitus. Ann Intern Med 140:94–100
Ndrepepa G, Kastrati A, Braun S, Koch W, Kölling K, Mehilli J et al (2006) A prospective cohort study of predictive value of homocysteine in patients with type 2 diabetes and coronary artery disease. Clin Chim Acta 373:70–76
Selhub J (2006) The many facets of hyperhomocysteinemia: studies from the Framingham cohorts. J Nutr 136:1726S–1730S
Brattström L, Wilcken DEL (2000) Homocysteine and cardiovascular disease: cause or effect? Am J Clin Nutr 72:315–323
Passaro A, D’Elia K, Pareschi P, Calzoni F, Carantoni M, Fellin R et al (2000) Factors influencing plasma homocysteine levels in type 2 diabetes. Diabetes Care 23:420–421
Russo GT, Friso S, Jacques PF, Rogers G, Cucinotta D, Wilson PW et al (2003) Age and gender affect the relation between methylenetetrahydrofolate reductase C677T genotype and fasting plasma homocysteine concentrations in the Framingham Offspring Study cohort. J Nutr 133:3416–3421
Arai K, Yamasaki Y, Kaijmoto YY, Watada H, Umayahara Y, Kodama M et al (1997) Association of methylenetetrahydrofolate reductase gene polymorphism with carotid arterial wall thickening and myocardial infarction risk in NIDDM. Diabetes 46:2102–2104
Hasegawa G, Obayashi H, Kamiuchi K, Nakai M, Kanatsuna T, Yamaguchi M et al (2003) The association between end-stage diabetic nephropathy and methylenetetrahydrofolate reductase genotype with macroangiopathy in type2 diabetes mellitus. Exp Clin Endocrinol Diabetes 111:132–138
Sun J, Xu Y, Xue J, Zhu Y, Lu H (2005) Methylenetetrahydrofolate reductase polymorphism associated with susceptibility to coronary heart disease in Chinese type 2 diabetic patients. Mol Cell Endocrinol 229:95–101
Mazza A, Motti C, Nulli A, Pastore A, Andreotti F, Ammaturo V et al (1999) Serum homocysteine, MTHFR gene polymorphism, and carotid intimal-medial thickness in NIDDM subjects. J Thromb Thrombolysis 8:207–212
Scaglione L, Gambino R, Rolfo E, Lillaz E, Gai M, Cassader M et al (2002) Plasma homocysteine, methylenetetrahydrofolate reductase gene polymorphism and carotid intima-media thickness in Italian type 2 diabetic patients. Eur J Clin Invest 32:24–28
The Heart Outcomes Prevention Evaluation (HOPE) 2 Investigators (2006) Homocysteine lowering with folic acid and B vitamins in vascular disease. N Engl J Med 354:1567–1577
B-Vitamin Treatment Trialists’ Collaboration (2006) Homocysteine-lowering trials for prevention of cardiovascular events: a review of the design and power of the large randomized trials. Am Heart J 151:282–287
Avogaro A, Giorda C, Maggini M, Mannucci E, Raschetti R, Raschetti R, Raschetti R, Raschetti R, Lombardo F, Diabetes, Informatics Study Group, Association of Clinical Diabetologists, Istituto Superiore di Sanità (2007) Incidence of coronary heart disease in type 2 diabetic men and women: impact of microvascular complications, treatment, and geographic location. Diabetes Care 30:1241–1247
Cheng TY, Wen SF, Astor BC, Tao XG, Samet JM, Wen CP (2008) Mortality risks for all causes and cardiovascular diseases and reduced GFR in a middle-aged working population in Taiwan. Am J Kidney Dis 52:1051–1060
Conflict of interest statement
The authors state that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Russo, G.T., Di Benedetto, A., Magazzù, D. et al. Mild hyperhomocysteinemia, C677T polymorphism on methylenetetrahydrofolate reductase gene and the risk of macroangiopathy in type 2 diabetes: a prospective study. Acta Diabetol 48, 95–101 (2011). https://doi.org/10.1007/s00592-009-0169-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-009-0169-5