Abstract
Hyperglycaemia caused by stress and inflammation is common during critical illness. We hypothesised that a latent glucose metabolism disturbance contributes to development of hyperglycaemia and that those patients have increased risk for diabetes. We included patients with sepsis, acute coronary syndrome and acute heart failure with no history of impaired glucose metabolism and divided them in the hyperglycaemia group (glucose ≥ 7.8 mmol/l) and normoglycaemia group. Patients were followed for 5 years. Follow-up was completed for 115 patients in the normoglycaemia group, of which 4 (3.5%) developed type 2 diabetes. In the hyperglycaemia group 51 patients finished follow-up and 8 (15.7%) developed type 2 diabetes. Relative risk in 5-year period for patients with hyperglycaemia was 4.51 for development of type 2 diabetes. Patients with hyperglycaemia during critical illness who are not diagnosed with diabetes before or during the hospitalisation should be considered a population at increased risk for developing diabetes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hyperglycaemia during critical illness is a common occurrence and has lately been put in focus after recent studies had shown that tight glycaemic control can be associated with better outcomes in intensive care unit (ICU) patients [1–4]. Hyperglycaemia may occur in patients with established diagnosis of diabetes, in patients with previously unrecognised diabetes, but in many cases in patients with normal glucose metabolism before and after the acute disease.
The mechanisms leading to increase in blood glucose during critical illness are complex and are a part of stress reaction and inflammatory response. Stress is associated with activation of hypothalamic–pituitary–adrenal axis with consequent release of cortisol, but stress response is also associated with increase in secretion of other hormones that can induce hyperglycaemia: catecholamines, glucagon and growth hormone [5, 6]. Proinflammatory cytokines such as interleukin-1 (IL-1) and tumour necrosis factor alpha (TNF-α) cause hyperglycaemia and peripheral insulin resistance by promoting the same counter-regulatory hormones, but also by altering insulin receptor signalling [7–11]. In muscle and fat cells insulin resistance decreases glucose uptake, while in hepatocytes it causes ongoing gluconeogenesis despite hyperglycaemia and increased insulin release. Even with hyperglycaemia and peripheral insulin resistance insulin concentrations may be normal or even decreased [12–14], due to suppression of pancreatic beta-cells caused by proinflammatory cytokines and stimulation of alpha receptors by catecholamines [12, 15]. These endocrine and metabolic changes are physiologic responses to stress and disease and probably occur in all patients, but evident hyperglycaemia is not present in all critically ill patients. It is associated with severity of illness, and has been associated with unfavourable outcomes in several acute conditions [1, 2, 16, 17]. Nevertheless, all patients with severe infections, severe myocardial infarction or other critical illnesses do not develop hyperglycaemia and some will have hyperglycaemia even in milder disease.
Our hypothesis was that hyperglycaemia of critical illness occurs not only as a marker of disease severity, but also as a marker of a latent disturbance in glucose metabolism, and that it may be associated with increased risk of developing overt disorder of glucose metabolism in the period following critical illness.
Patients and methods
This was a single centre study that included patients admitted to the Medical ICU, University Hospital Rebro during 3 years (Jan 2000–Dec 2002).
Adult patients who were hospitalised in our ICU with negative history for disorders of glucose metabolism [diabetes mellitus (DM), impaired fasting glucose (IFG) or impaired glucose tolerance (IGT)] and who were discharged from the hospital alive were considered for inclusion. To enable better congruence of groups and comparison of results, we have selected only the three most frequent admission diagnoses associated with critical care hyperglycaemia in our ICU: sepsis (including severe sepsis and septic shock), acute coronary syndrome (acute myocardial infarction and unstable angina) and acute heart failure (without acute ischaemia).
Two groups of patients were formed: hyperglycaemia group and normoglycaemia group. Patients were included in the normoglycaemia group if their venous blood glucose (random measurements) during the whole ICU stay never exceeded 7.7 mmol/l, while the patients who had hyperglycaemia (random venous blood glucose ≥7.8 mmol/l) on at least two occasions formed the hyperglycaemia group. Patients with only one hyperglycaemic episode were excluded to prevent possible measurement errors. We also excluded patients who were receiving corticosteroid treatment during or 2 months before the ICU admission and those with an endocrine disorder that may alter glucose metabolism. Absence of hyperglycaemia was confirmed before hospital discharge to rule out patients with previously unrecognised diabetes or impaired glucose metabolism, and if the diagnosis of IFG, IGT or DM was established, the patient was excluded from the study. Other exclusion criteria were: disseminated malignant disease, end-stage chronic disease or any other acute or chronic condition that was expected to cause early fatality and hinder follow-up. Patients who were unwilling to participate were, also excluded from the study.
The follow-up time had to be at least 5 years, during which, the onset of fasting hyperglycaemia, glucose intolerance or diabetes mellitus was noted. We have concluded the follow up on 1st April 2008.
Definitions
Impaired fasting glucose (IFG), impaired glucose tolerance (IGT) and diabetes mellitus (DM) were defined according to the ADA criteria [18].
Sepsis, severe sepsis and septic shock were defined according to the usual criteria [19].
Acute coronary syndrome, unstable angina and myocardial infarction were defined according to the ACC/AHA criteria [20, 21].
Statistical analyses
MedCalcTM v. 7.2.1.0 statistical software was used for all statistical analyses. Categorical data are presented as absolute and relative frequencies, continuous variables as median with inter-quartile range (IQR). Since the distribution of data of the continuous variables did not always follow normal distribution, Wilcoxon’s test was chosen for group comparisons of continuous variables, Chi-squared test for categorical variables. Statistical significance was set at P < 0.05.
Results
During the three inclusion years there were 1154 admissions to our ICU, 685 (59.3%) with the selected diagnoses (sepsis, acute coronary syndrome and acute heart failure), 553 with no history of hyperglycaemia or diabetes mellitus prior to the admission. Of those, 511 (92.4%) were discharged from the hospital alive and were considered for inclusion in the study. We have excluded 91 patients because of terminal illness (see exclusion criteria), and another 89 patients who had refused to be included in the study.
Of the remaining 331 patients, 168 were normoglycaemic during the whole ICU stay and 135 had two episodes of hyperglycaemia. Only one hyperglycaemic episode was present in 28 patients who were excluded to rule out errors in measurement.
We have excluded 26 patients from the hyperglycaemia group, since previously undiagnosed diabetes or impaired glucose metabolism (IFG or IGT) was established during the hospitalisation. We also excluded 19 patients who had been receiving corticosteroid therapy from the hyperglycaemia group.
Finally, we initiated follow-up for 168 patients in the normoglycaemia group and 90 patients in the hyperglycaemia group. The two groups were well matched: there were no significant differences between the two groups in age, sex distribution, family history of diabetes, body mass index or cholesterol levels (Table 1). Patients in the hyperglycaemia group had higher serum triglyceride concentrations than those in normoglycaemia group (median 1.9 vs. 1.4, respectively; P = 0.045).
During the 5 years of follow-up, 24 (14.3%) patients in the normoglycaemia group and 17 (18.8%) patients in the hyperglycaemia group died. There were 29 patients in the normoglycaemia group and 22 in the hyperglycaemia group who discontinued their assessments and did not enter the final analysis.
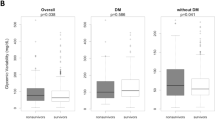
Of 115 patients in the normoglycaemia group who finished follow-up 16 (13.9%) developed fasting hyperglycaemia or impaired glucose tolerance, while 4 (3.5%) were diagnosed as type 2 diabetes mellitus during the follow-up period. In the hyperglycaemia group 51 patients finished follow-up period of which 14 (27.5%) developed IFG or IGT, while 8 (15.7%) developed type 2 diabetes (Table 2). Chi-squared test showed this to be a statistically significant difference (P = 0.001). According to these results, patients with hyperglycaemia (defined as glucose ≥ 7.8 mmol/l) during critical illness had a relative risk for developing IFG or IGT of 1.97 (95% CI 1.04–3.73) and for developing type 2 diabetes a relative risk of 4.51 (95% CI 1.42–14.30).
When we evaluated the three inclusion diagnoses separately we found that the absolute and relative risks for the onset of newly diagnosed impaired glucose metabolism and for type 2 diabetes were similar among the three subgroups (Table 2).
Discussion
Our results show increased risk for the onset of type 2 diabetes mellitus or impaired glucose metabolism (IFG or IGT) in the group of patients who had hyperglycaemia during the ICU stay. Patients in the two groups did not differ significantly in the classical risk factors, so the higher risk in the hyperglycaemia group could be attributed to the (pre-existent) impairment of glucose metabolism, which was latent before the acute illness. During acute illness the hyperglycaemic mechanisms in stress and inflammatory response led to revealing of the disorder with increased blood glucose concentrations which have returned to normal after the insult was weighed down. Nevertheless, the metabolic impairment remained and in some patients grew to overt impairment of glucose metabolism: IFG, IGT or even diabetes during the years following the acute illness.
The results are similar among the three diagnoses included in the study: sepsis, acute coronary syndrome and acute heart failure. Although the mechanisms leading to hyperglycaemia in those three pathophysiologically very different conditions are probably also different, patients suffer comparable risks for development of DM, IFG or IGT. This supports the theory that hyperglycaemia of acute illness is only triggered by stress and/or inflammation and that there is an underlying condition co-responsible for the increase in glucose. Selection of three most common diagnoses enabled better comparability of the groups and analysis of the results, but limits the ability to draw generalised conclusions, for which we shall need studies on unselected ICU populations (surgical and medical).
There is no universal consensus on the definition of hyperglycaemia during critical illness [22]; different studies used different criteria. We have defined hyperglycaemia during critical illness as venous blood glucose concentration >7.7 mmol/l, which is a cut-off value in the Recommendations of the American Heart Association [23] and a threshold for initiation of insulin treatment for ICU patients recommended by the American college of endocrinology [24–26]. We also used personal experience according to which almost all patients have some increase in blood glucose during critical illness, so a lower threshold would not be selective enough. Higher threshold would probably have higher specificity for patients with an inherent glucose metabolism disturbance, but smaller selectivity. The results themselves show that the threshold was well chosen. Definitive verdict on the cut-off value for hyperglycaemia in critical illness is still to be made, based on past and future studies.
Despite the 3 years of inclusion, this was a rather small study in which we were able to finalise the follow-up in only 166 patients. Larger, multi-centre studies with longer follow-up period will be needed to further substantiate our results. We feel that our results are sufficient enough to suggest that the patients with hyperglycaemia during critical illness, who are discharged from the hospital with normal glucose control, should be perceived as patients with increased risk of developing impaired glucose metabolism or diabetes and should as such be regularly monitored and treated appropriately. Change in dietary habits, weight reduction and physical activity should be recommended to all. Regular follow-up should also be initiated (at least once a year). In addition to fasting plasma glucose measurement and oral glucose tolerance test which identify glucose metabolism disturbances, adiponectin could also be measured to detect patients with higher risk of insulin intolerance and thus hither risk of developing type II diabetes [27].
References
Benfield T, Jensen JS, Nordestgaard BG (2007) Influence of diabetes and hyperglycaemia on infectious disease hospitalisation and outcome. Diabetologia 50:549–554
Christiansen C, Toft P, Jorgensen HS et al (2004) Hyperglycaemia and mortality in critically ill patients. A prospective study. Intensive Care Med 30:1685–1688
van den Berghe G, Wouters P, Weekers F et al (2001) Intensive insulin therapy in the critically ill patients. N Engl J Med 345:1359–1367
Malmberg K, Norhammar A, Wedel H et al (1999) Glycometabolic state at admission: important risk marker of mortality in conventionally treated patients with diabetes mellitus and acute myocardial infarction: long-term results from the Diabetes and Insulin-Glucose Infusion in Acute Myocardial Infarction (DIGAMI) study. Circulation 99:2626–2632
Van den Berghe G (2002) Neuroendocrine pathobiology of chronic critical illness. Crit Care Clin 18:509–528
Langouche L, Van den Berghe G (2006) The dynamic neuroendocrine response to critical illness. Endocrinol Metab Clin North Am 35:777–791, ix
McCowen KC, Malhotra A, Bistrian BR (2001) Stress-induced hyperglycemia. Crit Care Clin 17:107–124
Grimble RF (2002) Inflammatory status and insulin resistance. Curr Opin Clin Nutr Metab Care 5:551–559
Marette A (2002) Mediators of cytokine-induced insulin resistance in obesity and other inflammatory settings. Curr Opin Clin Nutr Metab Care 5:377–383
Marik PE, Raghavan M (2004) Stress-hyperglycemia, insulin and immunomodulation in sepsis. Intensive Care Med 30:748–756
Aljada A, Ghanim H, Assian E et al (2002) Tumor necrosis factor-alpha inhibits insulin-induced increase in endothelial nitric oxide synthase and reduces insulin receptor content and phosphorylation in human aortic endothelial cells. Metabolism 51:487–491
Mizock BA (2001) Alterations in fuel metabolism in critical illness: hyperglycaemia. Best Pract Res Clin Endocrinol Metab 15:533–551
Clowes GH Jr, Martin H, Walji S et al (1978) Blood insulin responses to blood glucose levels in high output sepsis and septic shock. Am J Surg 135:577–583
Dahn MS, Jacobs LA, Smith S et al (1985) The relationship of insulin production to glucose metabolism in severe sepsis. Arch Surg 120:166–172
Mehta VK, Hao W, Brooks-Worrell BM et al (1994) Low-dose interleukin 1 and tumor necrosis factor individually stimulate insulin release but in combination cause suppression. Eur J Endocrinol 130:208–214
Metso AJ, Murros K (2007) Hyperglycaemia and the outcome of stroke. Brain 130:e85 (author reply e86)
Cubbon RM, Rajwani A, Abbas A et al (2007) Hyperglycaemia, in relation to sex, and mortality after acute coronary syndrome. Eur J Cardiovasc Prev Rehabil 14:666–671
American Diabetes Association (2008) Diagnosis and classification of diabetes mellitus. Diabetes Care 31(Suppl 1):S55–S60
Levy MM, Fink MP, Marshall JC et al (2003) 2001 SCCM/ESICM/ACCP/ATS/SIS international sepsis definitions conference. Intensive Care Med 29:530–538
Pollack CV Jr, Braunwald E (2008) 2007 update to the ACC/AHA guidelines for the management of patients with unstable angina and non-ST-segment elevation myocardial infarction: implications for emergency department practice. Ann Emerg Med 51:591–606
Braunwald E, Antman EM, Beasley JW et al (2000) ACC/AHA guidelines for the management of patients with unstable angina and non-ST-segment elevation myocardial infarction. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on the Management of Patients With Unstable Angina). J Am Coll Cardiol 36:970–1062
Goran KP (2007) The consensus is clearly needed for the definition of stress hyperglycaemia in acute myocardial infarction. Eur Heart J 28:2042 (author reply 2042–2043)
Deedwania P, Kosiborod M, Barrett E et al (2008) Hyperglycemia and acute coronary syndrome: a scientific statement from the American Heart Association Diabetes Committee of the Council on Nutrition, Physical Activity, and Metabolism. Circulation 117:1610–1619
Inzucchi SE, Rosenstock J (2005) Counterpoint: inpatient glucose management: a premature call to arms? Diabetes Care 28:976–979
Bryer-Ash M, Garber AJ (2005) Point: inpatient glucose management: the emperor finally has clothes. Diabetes Care 28:973–975
Garber AJ, Moghissi ES, Bransome ED Jr et al (2004) American College of Endocrinology position statement on inpatient diabetes and metabolic control. Endocr Pract 10(Suppl 2):4–9
Kadowaki T, Yamauchi T, Kubota N et al (2006) Adiponectin and adiponectin receptors in insulin resistance, diabetes, and the metabolic syndrome. J Clin Invest 116:1784–1792
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gornik, I., Vujaklija, A., Lukić, E. et al. Hyperglycaemia in critical illness is a risk factor for later development of type II diabetes mellitus. Acta Diabetol 47 (Suppl 1), 29–33 (2010). https://doi.org/10.1007/s00592-009-0115-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-009-0115-6