Abstract
Purpose
Although pubic ramus fractures are common in the elderly, resultant hemodynamic instability is a rare complication. The corona mortis, a vascular anastomosis between the obturator vessels and the external iliac vessels in the retropubic space, is occasionally damaged by fractures of the pubic ramus, causing significant hemorrhage. The purpose of this study was to evaluate the incidence and anatomical position of the corona mortis on the anteroposterior and inlet views.
Methods
Sixty-one cadavers (122 hemipelvizes) were dissected and the incidence of the corona mortis was evaluated. Photographs were then taken simulating anteroposterior and inlet radiographs, and labeled as the anteroposterior and inlet views. The distance from the pubic symphysis to the corona mortis was measured on each of the two views.
Results
The corona mortis was present in 76.1% of hemipelvizes. The corona mortis traverses along the periosteum of the dorsal surface of the pubis. The incidence of arterial corona mortis was 28.3% and that of venous corona mortis was 76.1%. The distance from the superior margin of the symphysis pubis to the corona mortis measured 47.7 ± 9.9 (45.9–49.6) mm on the anteroposterior view, and 59.4 ± 9.2 (57.3–61.5) mm on the inlet view.
Conclusions
In order to predict possible hemodynamic instability of the corona mortis following pubic ramus fractures, it is of clinical significance to precisely establish the anatomical position of the corona mortis on the anteroposterior and inlet views.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fractures of the pubic ramus are common injuries in the elderly. Hill et al [1]. indicated that the incidence of pubic ramus fractures was 25.6 per 100,000 people a year in patients over 60 years of age; a 3.7 times higher incidence than in the overall population. A majority of these injuries in elderly patients are cause by low energy mechanisms and 95% of elderly patients with isolated pubic ramus fractures require hospitalization; however, hemodynamic instability is a rare occurrence [2]. Several studies have presented cases of stable pubic ramus fractures accompanied by massive extraperitoneal hemorrhaging from the corona mortis [3, 4]. The corona mortis is defined as a vascular anastomosis between the obturator vessels and the external iliac vessels in the retropubic space [5]. Its Latin name means “crown of death” due to its risk of significant hemorrhage following vascular injury, and benign pubic ramus fractures have been implicated as a risk factor for significant bleeding from the corona mortis in the elderly [4, 6]. Some previous studies also reported additional risk factors consisting of iatrogenic injuries of the corona mortis in various pelvic surgeries, including laparoscopic hernia repair, surgical procedures for urinary incontinence, and gynecological oncologic procedures [6,7,8]. In order to determine the incidence and location of corona mortis as well as its implications in pelvic and acetabular fractures, some authors performed cadaveric studies with computed tomography (CT) assessment [6, 9].
The pubic ramus fractures are typically diagnosed on anteroposterior and inlet radiographs upon initial presentation [2, 10]; CT imaging is used to identify occult injuries that were equivocal on plain film radiographs [11]. Therefore, knowledge of the location of the corona mortis in relation to fractures would give a higher awareness of their potential injury.
The purpose of this study was to evaluate the incidence and anatomical position of the corona mortis on the anteroposterior and inlet views taken according to conventional radiographic positioning. Our hypothesis was that the accurate anatomical position of the corona mortis would change depending on the specific view. We are not aware of such a study in the previous literature.
Materials and methods
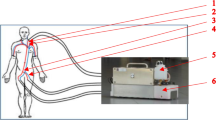
Sixty-one cadavers, ranging in age from 65 to 106 years (mean age 85 years) provided 122 hemipelvizes for this study. There were 58 male and 64 female hemipelvizes. All cadavers were persons who donated for medical education and research to our university. Prior to the donation, written consent from persons and families was obtained. The protocol of the present research project has been approved by the Ethics Committee of our university (No. 2014138). The subcutaneous soft tissue and muscles around the pubic bone were removed, with the exception of obturator vessels, external iliac vessels, inferior epigastric vessels, and corona mortis. We identified the vessels connecting the obturator vessels with the external iliac or inferior epigastric vessels as the corona mortis based on previous studies [5, 6], and then evaluated the incidence and vascular patterns of the corona mortis. To evaluate the vessels macroscopically, thin vessels less than 2 mm in diameter were excluded according to previous studies [12]. The cadavers with vessels less than 2 mm in diameter were 6 hemipelvizes. In addition, 3 hemipelvizes that could not be evaluated were excluded. Finally, 113 hemipelvizes were evaluated. (Fig. 1)
The distance from the pubic symphysis to the corona mortis was also measured on photographs of the pelvic bones. To evaluate the range of the corona mortis on the dorsal surface of the pubic ramus, intersection points of the corona mortis with the superior (■ in Fig. 2) or inferior (△ in Fig. 2) aspects of the dorsal surface of the pubic ramus were identified (Fig. 2). Next, the range of the corona mortis locations with respect to the superior pubic ramus was assessed, measuring the distance between the pubic symphysis and the corona mortis on the superior pubic ramus. A perpendicular line to the superior pubic ramus along its dorsal surface (dotted line in Fig. 2b) was drawn from the intersection point of the corona mortis and the inferior pubic ramus (△). The intersection point of the superior pubic ramus with the perpendicular line was defined as I point (▲ in Fig. 2b), and the intersection point of the corona mortis with the superior pubic ramus was defined as S point (■ in Fig. 2b). Linear distance from the superior margin of the pubic symphysis (● in Fig. 2) to the nearer point in I and S points on the superior pubic ramus was defined as the proximal distance; distance to the farer point was defined as the distal distance. Then photographs of the pelvic bones were taken and the proximal and distal distances were measured to evaluate the position of the corona mortis on the superior pubic ramus on photographs. The pelvic bones were fixed in the standard supine position, and photographs were taken simulating the anteroposterior radiograph technique [13, 14] (Fig. 2c). These photos were labeled as the anteroposterior views. Photographs were also taken with the pelvic bones set at a 45 degrees caudal angle, simulating the inlet radiograph technique; these were labeled as the inlet views [13, 15] (Fig. 2d). The proximal and distal distances of the corona mortis on the superior pubic ramus were measured on both the anteroposterior and inlet views using Image J 1.51 software (National Institute of Health, Bethesda, Maryland, USA) (Fig. 2c, d).
Evaluating method for range of the corona mortis on the dorsal surface of the pubic ramus. a Intersection points of the corona mortis with the superior (■) or inferior (△) pubic ramus were identified on the dorsal surface of the pubic ramus. b To measure the range of the corona mortis on the superior pubic ramus, a perpendicular line to the superior pubic ramus was drawn along the dorsal surface (dotted line) from the intersection point of the corona mortis with the inferior pubic ramus (△). The intersection points of the superior pubic ramus with the perpendicular line were defined as I point (▲), and the intersection point of the corona mortis with the superior pubic ramus was defined as S point (■). c A photograph of the anteroposterior view. d A photograph of the inlet view. The distance from the superior margin of the pubic symphysis (●) to I (▲) and S (■) points of the corona mortis was measured in each of the two views (c) (d). The shorter distance was defined as the proximal distance, and the longer one was defined as distal distance
Results
The corona mortis was observed in 88 of 113 hemipelvizes (76.1%). All traversed along the periosteum of the dorsal surface of the pubic bone. The incidence of arterial corona mortis was 32 of 113 (28.3%) and that of venous corona mortis was 88 (76.1%). All of the arterial corona mortis occurrences also presented with the venous corona mortis (Table 1).
The distance from the superior margin of the symphysis pubis to the corona mortis on the anteroposterior and inlet views is shown in Table 2. On the anteroposterior view, the average of the proximal distance and distal distance was 45.9 ± 9.5 (21.8–68.9) mm and 49.6 ± 9.9 (27.2–74.0) mm, respectively. On the inlet view, the average of the proximal distance and lateral distance was 57.3 ± 9.2 (22.9–85.6) mm and 61.5 ± 8.8 (40.5–85.6) mm, respectively.
Discussion
The corona mortis traverses along the periosteum of the dorsal surface of the pubis from 45.9 to 49.6 mm on the anteroposterior view and 57.3 to 61.5 mm on the inlet view in this present study. The distance on the anteroposterior view was different from previous studies that showed the distance ranged from 50 to 71 mm, measuring along the superior pubic ramus using cadavers and CT scans [6, 16, 17]. Our study may be the first report of anatomical position of the corona mortis on views simulating actual anteroposterior and inlet radiographic technique, and the findings may be useful to predict potential vascular injury of the corona mortis when identifying pubic ramus fractures on anteroposterior and inlet radiographs.
Vascular injury of the corona mortis caused by the pubic ramus fractures can be diagnosed on contrast CT [18]. However, the pubic ramus fractures were typically diagnosed—using anteroposterior and inlet radiographs upon initial presentation, as the plain film can be performed easier, quicker, and with less radiation exposure [2, 10, 19, 20]. CT scans were not absolutely necessary in the routine diagnosis of isolated pubic rami fractures. Patients with pubic ramus fractures often had concomitant posterior pelvic fractures [19]; however, the sensitivity of plain radiographs for anterior pelvic ring fractures was similar to that of CT, and the patients often were not given CT scans [10]. Therefore, it is clinically significant to know the anatomical position of the corona mortis on radiographs in order to predict occurrence of potential hemorrhage from the damaged corona mortis.
Our results are consistent with the previous literature. The overall incidence of corona mortis in our study was 76.1%, with 28.3% for the arterial version and 76.1% for the venous version. Previous reports have shown an overall corona mortis incidence of 72 to 84% [6, 21], with 19 to 43% for the arterial form [9, 12], 59 to 70% for the venous form [6], and 20 to 28% for both forms occurring together [6, 21]. In pelvic fractures, venous injuries have been reported as major source of hemorrhage requiring packing [22]. On the other hand, arterial injuries requiring embolization were less than 10% [18]. In the corona mortis, venous injuries may also be a main factor of significant hemorrhage; consequently, early immediate pelvic packing may be needed if hemodynamic instability has occurred [23] and the low rate of arterial anastomosis in this study also supported this.
This study has several limitations. First, we measured distance from the symphysis pubis to the corona mortis on photographs of anteroposterior and inlet views instead of actual radiographs. Although it may be optimal to measure on radiographs of the pelvic bones, the pictures were taken simulating anteroposterior and inlet radiograph technique and they may still be useful. Second, we excluded vessels under 2 mm in diameter. The average diameter of the vessels has been reported as between 2.4 and 4.2 mm [6, 16], and smaller caliber vessel injuries occurred in only 1.5% of patients in laparoscopic surgery [8]. Okcu et al. excluded the vessels less than 2 mm as not relevant size [12]. We also excluded evaluation of thinner vessels according to these previous studies.
Conclusion
The incidence of the corona mortis was 76.1%, and its distance from the symphysis pubis was 47.7 ± 9.9 mm on the anteroposterior view and 59.4 ± 9.2 mm on the inlet view. To predict possible hemodynamical instability of the corona mortis following pubic ramus fractures, it is clinically significant to know the anatomical position of the corona mortis on both the anteroposterior and inlet views.
References
Hill RM, Robinson CM, Keating JF (2001) Fractures of the pubic rami. Epidemiology and five-year survival. J Bone Jt Surg Br 83(8):1141–1144. https://doi.org/10.1302/0301-620x.83b8.11709
Koval KJ, Aharonoff GB, Schwartz MC, Alpert S, Cohen G, McShinawy A, Zuckerman JD (1997) Pubic rami fracture: a benign pelvic injury? J Orthop Trauma 11(1):7–9. https://doi.org/10.1097/00005131-199701000-00003
Coupe NJ, Patel SN, McVerry S, Wynn-Jones CH (2005) Fatal haemorrhage following a low-energy fracture of the pubic ramus. J Bone Jt Surg Br 87(9):1275–1276. https://doi.org/10.1302/0301-620x.87b9.16696
Theodorides AA, Morgan BW, Simmons D (2011) Haemodynamic instability resulting from a low energy pubic ramus fracture in a 78-year-old woman. A case report and review of the literature. Injury 42(7):722–724. https://doi.org/10.1016/j.injury.2010.08.037
Berberoglu M, Uz A, Ozmen MM, Bozkurt MC, Erkuran C, Taner S, Tekin A, Tekdemir I (2001) Corona mortis: an anatomic study in seven cadavers and an endoscopic study in 28 patients. Surg Endosc 15(1):72–75. https://doi.org/10.1007/s004640000194
Darmanis S, Lewis A, Mansoor A, Bircher M (2007) Corona mortis: an anatomical study with clinical implications in approaches to the pelvis and acetabulum. Clin Anat 20(4):433–439. https://doi.org/10.1002/ca.20390
Pellegrino A, Damiani GR, Marco S, Ciro S, Cofelice V, Rosati F (2014) Corona mortis exposition during laparoscopic procedure for gynecological malignancies. Updat Surg 66(1):65–68. https://doi.org/10.1007/s13304-013-0245-9
Ates M, Kinaci E, Kose E, Soyer V, Sarici B, Cuglan S, Korkmaz F, Dirican A (2016) Corona mortis: in vivo anatomical knowledge and the risk of injury in totally extraperitoneal inguinal hernia repair. Hernia: J Hernias Abdom Wall Surg 20(5):659–665. https://doi.org/10.1007/s10029-015-1444-8
Karakurt L, Karaca I, Yilmaz E, Burma O, Serin E (2002) Corona mortis: incidence and location. Arch Orthop Trauma Surg 122(3):163–164. https://doi.org/10.1007/s004020100341
Berg EE, Chebuhar C, Bell RM (1996) Pelvic trauma imaging: a blinded comparison of computed tomography and roentgenograms. J Trauma 41(6):994–998. https://doi.org/10.1097/00005373-199612000-00009
Krappinger D, Kammerlander C, Hak DJ, Blauth M (2010) Low-energy osteoporotic pelvic fractures. Arch Orthop Trauma Surg 130(9):1167–1175. https://doi.org/10.1007/s00402-010-1108-1
Okcu G, Erkan S, Yercan HS, Ozic U (2004) The incidence and location of corona mortis: a study on 75 cadavers. Acta Orthop Scand 75(1):53–55. https://doi.org/10.1080/00016470410001708100
Pekmezci M, Kandemir U, Toogood P, Morshed S (2013) Are conventional inlet and outlet radiographs obsolete in the evaluation of pelvis fractures? J Trauma Acute Care Surg 74(6):1510–1515. https://doi.org/10.1097/TA.0b013e318292156c
Shi C, Cai L, Hu W, Sun J (2017) Study of the X-Ray diagnosis of unstable pelvic fracture displacements in three-dimensional space and its application in closed reduction. J Investig Surg: j Acad Surg Res. https://doi.org/10.1080/08941939.2017.1370518
Karkhur Y, Tiwari A, Maini L, Bansal V, Kakralia A (2018) Radiological evaluation of pelvic inlet and outlet radiographic view in Indian population. J Clin Orthop Trauma 9(4):334–337. https://doi.org/10.1016/j.jcot.2018.05.005
Steinberg EL, Ben-Tov T, Aviram G, Steinberg Y, Rath E, Rosen G (2017) Corona mortis anastomosis: a three-dimensional computerized tomographic angiographic study. Emerg Radiol 24(5):519–523. https://doi.org/10.1007/s10140-017-1502-x
Sanna B, Henry BM, Vikse J, Skinningsrud B, Pekala JR, Walocha JA, Cirocchi R, Tomaszewski KA (2018) The prevalence and morphology of the corona mortis (Crown of death): a meta-analysis with implications in abdominal wall and pelvic surgery. Injury 49(2):302–308. https://doi.org/10.1016/j.injury.2017.12.007
Tang CH, Shivji F, Forward D (2015) Major haemorrhage in pubic rami fractures. BMJ Case Rep. https://doi.org/10.1136/bcr-2014-208088
Turgut A, Kalenderer Ö, Akan I, Ilyas G, Kumbaraci M, Karapinar L (2017) Do patients with acute isolated pubic ramus fractures have to be hospitalized? Acta Orthop Belg 83(4):574–580
Pekmezci M, Rotter P, Toogood P, Morshed S, Kandemir U (2014) Reexamination of pelvic inlet and outlet images using 3-dimensional computed tomography reconstructions. J Orthop Trauma 28(6):324–329. https://doi.org/10.1097/bot.0000000000000018
Tornetta P 3rd, Hochwald N, Levine R (1996) Corona mortis. Incidence and location. Clin Orthop Relat Res 329:97–101
Tötterman A, Madsen JE, Skaga NO, Røise O (2007) Extraperitoneal pelvic packing: a salvage procedure to control massive traumatic pelvic hemorrhage. J Trauma 62(4):843–852. https://doi.org/10.1097/01.ta.0000221673.98117.c9
Parry JA, Smith WR, Moore EE, Burlew CCC, Mauffrey C (2020) The past, present, and future management of hemodynamic instability in patients with unstable pelvic ring injuries. Injury. https://doi.org/10.1016/j.injury.2020.02.101
Acknowledgements
The authors wish to acknowledge the generosity of the donors and their families for their great gift to our anatomical bequest program, which made the research possible, and also thank Enago (www.enago.jp) for the English language review.
Funding
None.
Author information
Authors and Affiliations
Contributions
TW (first author) mainly wrote this manuscript and performed dissection of the cadavers. YI (corresponding author), TN, AK, and KI were assistant of dissection. YI, YM, and MI discussed and advised about the dissection and evaluating. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
This study was approved by the ethics committee for medical research of our university (No.2014138), and written consent from persons and families was obtained prior to the donation.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wada, T., Itoigawa, Y., Wakejima, T. et al. Anatomical position of the corona mortis relative to the anteroposterior and inlet views. Eur J Orthop Surg Traumatol 32, 341–345 (2022). https://doi.org/10.1007/s00590-021-02983-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-021-02983-5