Abstract
Background
The management of limb deformity, shortening, and bone defects in treatment of Ollier’s disease is a major challenge. This study aims to summarize and compare the different surgical treatments, and to evaluate the outcome and possible prognostic factors of leg lengthening in these patients.
Materials and methods
A systematic review of the literature from 1993 to 2017 was performed. Nineteen articles were found including a total of 121 patients with limb deformities because of Ollier’s disease. The mean patients’ age at the time of first surgery was 12 years. A total of 272 segments were surgically treated (14 segments in the upper limbs) with variable techniques including osteotomies and external fixation, intramedullary nails, as well as epiphysiodesis and lengthening over nail. We studied the bone healing index (BHI), distraction index (DI), distraction time, gained length, total treatment time, and complications.
Results
Available implants and techniques allowed correction of patients’ deformities (lengthening and correction of angular defects) in most cases. External fixators, circular or monolateral frames were the most commonly used technique. The Ilizarov external fixator was the most commonly used frame (196 segments). The BHI was significantly better when the external fixation was combined with intramedullary nails. Epiphysiodesis was most likely to be more associated with the past than to the present. Joint stiffness, infection, early consolidation, pathological fracture, deformity recurrence, delayed union, non-union, neurapraxia, and overlengthening were the reported complications with an overall rate of 27.9%.
Conclusions
There is no consensus for the optimal surgical technique and implants for correction of limbs deformities in patients with Ollier’s disease. External fixators most commonly circular are the most commonly used implants; however, complications do occur.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ollier’s disease, known as multiple enchondromatosis, is a rare non-hereditary benign skeletal disorder, characterized by circumscribed lesions (3 or more) of cartilage arranged in a linear fashion with an asymmetric distribution [1]. Multiple enchondromatosis appears in early childhood. The estimated prevalence is 1:100,000, although the real incidence is unknown because mild phenotypes without skeletal deformities or secondary consequences are often not detected. Ollier’s disease is probably attributable to a failure of the normal enchondral ossification resulting from the proliferation of ectopic islands of chondroid tissue, or to the incapacity of the epiphyseal plate to become mature, causing residual chondroid proliferation in the bones [1, 2]. As a consequence, these patients experience bowing of the long bones and longitudinal growth anomalies resulting in deformities such as limb length discrepancies (LLD), genu valgus, and broadening of the metaphyses [3,4,5,6,7,8]. The affected bones show numerous islands of cartilage in close proximity to the physis and the adjacent metaphysis. All bones can be affected in variable degree, with the femur and tibia most often involved. LLD may range up to 10–25 cm by skeletal maturity [1, 2]. Cosmesis is partly a concern; shortening of a lower limb affects the vertebral column and causes stiffness of the ankle joint of the shortened leg and gait disturbances. The presence of weak bone and enchondromas is associated with an increased risk of pathological fractures. Last, patients with Ollier’s disease should be monitored for the risk of malignant degeneration to chondrosarcoma ranging from 10 to 30% [2].
Before the development of external fixators and distraction osteogenesis, the correction of the deformities and LLD in patients with Ollier’s disease was performed with conventional surgical treatments such as curettage of the cartilaginous lesions, bone grafting, osteotomies, and internal osteosynthesis with plates and screws; however, these options were not feasible in many patients with Ollier’s disease because the affected bone was weakened and LLD was usually substantial [3,4,5,6,7,8]. Internal osteosynthesis implants have been associated with complications, and importantly, they did not allow for lengthening of the involved bone. Therefore, unilateral and circular external fixation frames have become a popular treatment option in the last years [6,7,8,9,10,11,12,13,14,15,16,17,18]. The Ilizarov technique is the most common approach used to correct and lengthen LLD, although other types of external fixators have been developed such as the Multi-Axial Correction (MAC) System (Biomet Trauma, Warsaw, Indiana), the Orthofix fixators (Orthofix®, Verona, Italy), and the Taylor Spatial Frame (TSF, Smith and Nephew, Tennessee, USA). Combined techniques including lengthening intramedullary nailing, intramedullary nailing, and circular external fixators have been further described [15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30].
Because of the rarity of Ollier’s disease, there is still no standard consensus concerning the optimal surgical technique and implant. Therefore, we performed this study to summarize the current data with regard to surgical techniques used to manage LLD in patients with Ollier’s disease, to evaluate the outcomes of the obtained corrections, and to find a possible relationship between the type of correction technique and local recurrence or malignant degeneration in these patients.
Materials and methods
A systematic review was conducted using PubMed and Google Scholar research libraries. Level II to V studies published in the English language from 1993 to March 15 2017 were selected. Studies selection was repeated by a second reviewer for validity, and any discrepancies were resolved by a third reviewer. The search terms used in combination were “Ollier’s disease,” “bone lengthening,” “limb reconstruction,” “limb length discrepancy,” “distraction osteogenesis,” “external fixation,” “deformity treatment.” Previous articles were not considered as the techniques that were described by those authors are not consistent with current methods.
Inclusion criteria included Ollier’s disease patients, surgery in upper and lower limbs, both skeletally mature and immature patients, all lengthening techniques, staged and not surgery, primary and revision cases, and any possible complications. Exclusion criteria included enchondromas of the hands, skull, spine, or any localization not eligible for lengthening, or treated only by curettage. The clinical data extracted from the selected studies included the technique used, clinical results, and complications. The demographic data included age, gender, number and site of operated limbs, and LLD. The clinical results were categorized into objective outcomes including the bone healing index (BHI) or external fixation index (EFI), the distraction index (DI), the distraction time (DT), gained length (GL), and total treatment time (TTT), if reported by the studies’ authors. The BHI and EFI are similar; the BHI measures the time until bony union in days in the frame per the amount of lengthening in centimeters, and the EFI measures the time in the external fixator in days per the amount of lengthening in centimeters (days/cm). The DI measures the amount of lengthening per day (mm/day), and the TTT measures the number of days in the external fixator [3]. Complications were defined as any intraoperative or postoperative event that was likely to have a negative influence on the patient’s outcome, including pin track infection, non-union, early consolidation, pathological fracture, joint stiffness, nerve injury, and deformity recurrence.
Results
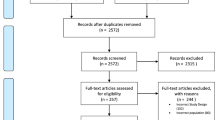
Study selection
The search strategy returned 84 studies; 23 studies were excluded as duplicates, 28 studies were excluded by their title, 10 studies were excluded by their abstract, and 4 studies were excluded by their full text. This left us 19 studies for further analysis [2, 5,6,7, 9,10,11,12, 14,15,16,17,18, 22,23,24,25,26, 30] (Fig. 1). The included studies consisted of case reports and retrospective case series. Because of substantial study heterogeneity and small samples sizes, the data obtained from the selected studies were not adequate to perform a meta-analysis. For these reasons, a descriptive approach to data analysis was performed. Among the 19 studies, 12 were specific on Ollier’s disease, while 7 studies described limb corrective treatments in variable disorders and benign tumors (fibrous dysplasia, fibular hemimelia, hemiatrophy osteomyelitis, giant cell tumor of bone, non-ossifying fibroma, osteochondroma and congenital multiple exostosis, desmoid fibroma, chondromyxoid fibroma, unicameral bone cyst, and Maffucci’s syndrome) including Ollier’s disease. Of the 198 total patients described in the identified studies, 121 patients had a diagnosis of Ollier’s disease and were considered in this analysis; the remaining 77 patients had deformities from the causes mentioned above and were excluded.
Study characteristics
Gender was reported for 57 patients, and age was reported for 112 patients only; there were 34 male and 23 female patients with an age range of 4–37 years at the time of the first surgery. The site of lengthening was consistently reported in all studies; the lower limbs were affected more common by deformities (110 patients), followed by the upper limbs (8 patients) and both upper and lower limbs (3 patients). Overall, 272 segments were lengthened, most commonly in femurs (146 segments, 53.7%), followed by tibias (113 segments, 41.5%), humeri (9 segments, 3.3%), and forearms (4 segments, 1.4%).
Correction techniques
Four techniques of LLD correction were identified: external fixation, external fixation combined with intramedullary nailing, motorized lengthening nailing, and epiphysiodesis. External fixators alone were used in 252 segments (92.6%). The most commonly used external fixators were circular frames (205 segments, 75.3%); Ilizarov external fixator alone was used in 196 segments (72%), followed by the Taylor Spatial Frame (5 segments), the Sheffield Ring Fixator (2 segments), the Smart External Fixator (1 segment), and the TrueLok ring fixator (1 segment). Unilateral external fixators alone were used in 47 segments (17.2%); the Limb Reconstruction System was used in 22 segments (46.8%), followed by the Orthofix external fixator (10 segments), the Wagner monoaxial external fixator (9 segments), the Heidelberg external fixator (2 segments), the MAC frame (2 segments), and the EBI external fixator (1 segment); in 1 segment, the type of unilateral external fixator was not reported. Combined external fixation and intramedullary nailing was used in 14 segments (5.1%); a circular frame (Ilizarov and TSF in 5 segments each) and elastic stable intramedullary nail were used in 10 segments, and unilateral external fixator and intramedullary nail in 4 segments. Epiphysiodesis was used in 3 segments (1.1%) aiming to shorten the longer limb and correct an angular deformity. Motorized lengthening nails were used in 3 segments (1.1%) in the same patient. Over the years, novel corrections techniques/implants were used, yet external fixators remained the most commonly used techniques/implants, with circular external fixators, most often Ilizarov frames, being used most common.
Outcomes
The BHI was reported in 14 of the 19 studies, and the DI was reported in 13. The BHI changes upon the bone treated (Table 1); the mean BHI for the femur was 33.3 days/cm, for the tibia, it was 34 days/cm, for the humerus, it was 26.4 days/cm, and for the forearm, it was 36.2 days/cm (range, 15.5–83 days/cm). The mean DI was 0.93 mm/day (range, 0.5–1.25). The LLD before treatment was reported in 12 studies, and it ranged from 4.4 to 17.4 cm for the lower limbs and from 4 to 14 cm for the upper limbs. The GL was reported in 15 studies, and it ranged from 2 to 22 cm for the lower limbs and from 4.1 to 14 cm for the upper limbs. The TTT was reported in 13 studies, and it ranged from 90 to 496 days, with a mean of 228.8 days for the upper limbs and 231.1 days for the lower limbs.
Complications related to surgical management
Overall, 76 complications occurred in the 272 lengthening procedures/segments (27.9%) (Table 2). There were 21 cases of joint stiffness (7.7%), especially in patients with simultaneous ipsilateral femoral and tibial lengthening that required long rehabilitation, 14 cases of moderate to severe pin track infection (5.1%) requiring antibiotics and/or hospitalization, 11 cases of early consolidation (4%) most of the times because the DI was too low requiring an increase, 9 cases of pathological fracture (3.3%), due to weakened bone and/or early frame removal, 8 cases of deformity recurrence (2.9%), 5 cases of delayed union (1.8%), 4 cases of non-union (1.4%) because of a high DI that required slowing down the distraction rate and/or bone grafting, 2 cases of radial nerve neurapraxia (0.7%), 1 case of common peroneal nerve neurapraxia (0.3%), and 1 case of overlengthening (0.3%). Minor complications including mild pin track infections were identified in more than 40 lengthened segments. With the available information from the selected papers, we did not conclude any correlation between the correction technique/implant used and the incidence of complications. Although a comparison between the techniques/implants used could not be performed because of the variable implants used by a plethora of surgeons and the use of circular external fixators (most commonly Ilizarov frames) in the majority of cases, it seems that circular frames especially combined with an intramedullary nail provide optimal results with few complications.
Discussion
Conventional surgical treatment for skeletal deformities is not feasible in many of patients with Ollier’s disease because the affected bone is weakened by the disease and the amount of lengthening necessary for correcting the discrepancy usually is substantial [4,5,6,7,8]. Traditional treatments included curettage of the enchondromas, bone grafting, corrective osteotomies, and internal fixation [9]. However, complete curettage of the enchondromas is realistically impossible as the lesions are extensive [4]. In contrast, lengthening is not more complex compared to other cases of LLD; growth disorder involves bone only, while soft tissues are normal, which explains the relatively straight lengthening procedure compared to that performed for the management of LLD in patients with congenital anomalies [7, 10, 11].
Concerns regarding limb lengthening in patients with Ollier's disease include the site of corticotomy, biological response of the bone to the lengthening process, structural quality of the regenerated callus, healing response, pathological fractures, and stability of the external fixator to the bone [2, 4,5,6,7, 9,10,11,12,13,14,15,16]. D’Angelo et al. advised that the osteosynthesis should be done in radiographically healthy bone and corticotomy should be done at the border between healthy and pathological bone [12]. Watanabe et al. reported seven osteotomies performed intralesionally and five extralesionally; in only one of the seven cases, the regenerated tissue appeared as normal bone [7]. Kolodziej et al. in four of five upper limbs lengthenings observed conversion of abnormal cartilage into normal bone on radiographs [5]. Tellisi et al. performed percutaneous osteotomy just distal to weakened bone from Ollier’s disease, but suggested that this can be performed either intra- or extralesionally [9]. Van Loon performed a corticotomy through a small incision at the margin of enchondroma and healthy bone and observed in radiographs regeneration of healthy bone within the region of diseased bone [17]. Groote et al. reported 20 intralesional, 6 transitional, and 14 extralesional corticotomies performed at the apex of the deformity or at a suitable level after the external fixator is anchored to the bone [18]. In their study, the site of corticotomy did not appear to be an important predictor of healing; on radiographs, the regenerated bone looked normal; however, no histological studies confirmed that [18] Madan and Baumgart, using external fixators or intramedullary nails, respectively, performed all osteotomies through enchondromas, and all formed normal bone [2, 6]. Martson and Jesus-Garcia were the only authors that performed a needle biopsy through the regenerated bone and showed that the benign neoplastic tissue was replaced with normal bone [10, 16]. Pandey et al. indicated that osteogenesis under tension occurs by intramembranous rather than by enchondral ossification, which explains the formation of normal regenerated bone [14, 19, 20].
The neo-ossification of regenerated bone at enchondromas is independent from the enchondromatosis because it involves the periosteum and not the physis [21]. Despite the concern of poor quality of the diseased bone, the healing response for fractures and limb lengthening has been remarkably good; healing of pathological and/or iatrogenic fractures was uncomplicated in all cases, either conservative or with adjustment of the implants in situ [4, 6, 7, 9, 10, 15, 18]. Limb lengthening has a similar healing response [5, 6, 9, 15, 18, 22]. The present systematic review showed a wide range of BHI ranging from 15.5 days/cm to 83 days/cm; this can be explained by the variable implants used and sites of lengthening. Additionally, some authors described lengthening in patients affected by variable comorbidities; this bias does not allow to verify whether there is a statistically significant difference between one technique or another for patients with Ollier’s disease only [11, 22,23,24,25,26]. The most commonly used implants were Ilizarov external fixators; this explained by the fact that application of the Ilizarov frames provides enough mechanical strength to perform elongation and axial correction. In contrast, unilateral external fixators are easier to apply and more comfortable for the patients compared to circular frames; however, their use is limited for simple leg lengthening in patients with Ollier’s disease [7]. Combined external fixators and intramedullary nails was reported in 5.2% of cases, and has been associated with significantly lower BHI [15].
Early consolidation of bone lengthening is more common in patients with Ollier’s disease [27]. Myers et al. noticed a tendency for hypertrophic bone regeneration in patients with achondroplasia and Ollier's disease [13] and recommended a higher rate of distraction. Similarly, Tellisi et al. described early consolidation in a case of humeral lengthening and recommended to accelerate the rate of lengthening of the humerus from 1 to 1.25 mm/day [9], which, however, was not recommended by Van Loon et al. [17]. Madan et al. described three cases of early consolidation in 10 patients that required manipulation under anesthesia and osteoclasis, or cessation of lengthening [6]. Groote et al. reported five cases of early consolidation in 40 femurs and performed repeated corticotomy and closed osteoclasis [18].
Delayed union or non-union may also occur in patients with Ollier’s disease [5, 14, 18]. Pandey et al. [5] and Kolodziej et al. [14] decreased the rate of distraction and concluded that DI of 1 mm/day for the forearm is too fast and half speed is advisable [5, 14]. The factors responsible for non-union include traumatic corticotomy, instability of the frame, initial diastasis, too rapid distraction, infection, malnutrition or multiple lengthenings through the same bone, and lengthened bone itself.
Pathological fractures are a concern during lengthening in Ollier’s disease because lengthening is performed within or around a tumor [6, 9, 10, 15, 18]. Popkov et al. reported pathological fractures in 3 cases through enchondromas after frame removal in the group with external fixator only [15]. In contrast, the group with combined external fixator and intramedullary nail had no pathological fractures; therefore, intramedullary nailing provides for additional mechanical stability at the lengthened site after frame removal. In general, the regenerate bone appears to be sufficiently strong after lengthening is completed and bone is healed, without long-term sequela. The timing of external fixator removal depends largely on qualitative assessment of the newly formed bone. However, trabeculation in at least three cortices must be visible in the anteroposterior and lateral radiographs for bone healing to be considered complete before frame removal [22].
Joint stiffness or contracture was a common complication in most studies; this is explained by the persistent muscle contracture, duration of adjacent joints immobilization, amount and rate of lengthening, and pressure through the joint surface [6, 10, 14, 16, 18, 22, 24, 26]. Most cases resolved with intense physiotherapy, bracing for soft tissue tension management, and, when possible, minimizing the TTT [11, 15, 18]. Malignant degeneration is another important concern in Ollier's disease [28, 29]. In the studies included in this review, malignant degeneration was not reported in any of the included patients at the site of limb lengthening. Groote et al. reported one patient who developed a low-grade chondrosarcoma of the proximal femur; however, the location of the sarcoma was not in the area of lengthening [18]. Therefore, lengthening in patients with Ollier’s disease should be considered safe.
Conclusion
Correction of deformities and LLD in patients with Ollier's disease is challenging. Although there is currently no consensus concerning the optimal surgical technique/implants for lengthening, it seems that circular frames with or without an intramedullary nail provide optimal results with few complications. Nevertheless, the regenerated bone is structurally normal. Early consolidation should be considered, and appropriate adjustment should be made in the rate of lengthening. Non-union is unusual in these patients but can occur. Joint stiffness and contracture can be avoided with intense physiotherapy. Malignant degeneration has not been reported, and the patients should be followed as recommended for their disease.
References
Ollier M (1900) De la dyschondroplasie. Bull Soc Chir Lyon 3:22–27
Baumgart R, Bürklein D, Hinterwimmer S, Thaller P, Mutschler W (2005) The management of leg-length discrepancy in Ollier's disease with a fully implantable lengthening nail. J Bone Joint Surg 87(B):1000–1004
De Bastiani G, Aldegheri R, Renzi-Brivio L, Trivella G (1987) Limb lengthening by callus distraction (callotasis). J Pediatr Orthop 7(2):129–134
Shapiro F (1982) Ollier's disease. An assessment of angular deformity, shortening, and pathological fracture in twenty-one patients. J Bone Joint Surg 64:95–103
Kolodziej L, Kołban M, Zacha S, Chmielnicki M (2005) The use of the ilizarov technique in the treatment of upper limb deformity in patients with Ollier's disease. J Pediatr Orthop 25(2):202–205
Madan SS, Robinson K, Kasliwal PD, Bell MJ, Saleh M, Fernandes JA (2015) Limb reconstruction in Ollier's disease. Strat Trauma Limb Recon 10:49–54
Watanabe K, Tsuchiya H, Sakurakichi K, Yamashiro T, Matsubara H, Tomita K (2007) Treatment of lower limb deformities and limb-length discrepancies with the external fixator in Ollier's disease. J Orthop Sci 12:471–475
Ilizarov GA (1990) Clinical application of the tension-stress effect for limb lengthening. Clin Orthop Relat Res 250:8–26
Tellisi N, Ilizarov S, Fragomen AT, Rozbruch SR (2008) Humeral lengthening and deformity correction in Ollier's disease: distraction osteogenesis with a multiaxial correction frame. J Pediatr Orthop B 17:152–157
Jesus-Garcia R, Bongiovanni JC, Korukian M, Boatto H, Seixas MT, Laredo J (2001) Use of the Ilizarov external fixator in the treatment of patients with Ollier's disease. Clin Orthop Relat Res 382:82–86
Curran AR, Kuo KN, Lubicky JP (1999) Simultaneous Ipsilateral Femoral and tibial lengthening with the Ilizarov Method. J Pediatr Orthop 19(3):386–390
D'Angelo G, Petas N, Donzelli O (1996) Lengthening of the lower limbs in Ollier's disease: problems related to surgery. Chir Organi Mov 81(3):279–285
Myers GJ, Bache CE, Bradish CF (2003) Use of distraction osteogenesis techniques in skeletal dysplasias. J Pediatr Orthop 23:41–45
Pandey R, White SH, Kenwright J (1995) Callus distraction in Ollier's disease: a case report. Acta Orthop 66:479–480
Popkov D, Journeau P, Popkov A, Haumont T, Lascombes P (2010) Ollier's disease limb lenghtening: should intramedullary nailing be combined with circular external fixation? Orthop Trauma Surg Res 96:348–353
Märtson A, Haviko T, Kirjanen K (2005) Extensive limb lengthening in Ollier's disease: 25-year follow-up. Medicina (Kaunas) 41(10):861–866
Van Loon P, Lammens J (2008) Malformation of the humerus in a patient with Ollier’s disease treated with the Ilizarov technique. J Shoulder Elbow Surg 17:e9–e11
Goote P, Altiok H, Beck J, Smith P, Ackman J, Hassani S, Kurapati N (2017) Limb lengthening in pediatric patients with Ollier's disease. J Limb Lengthen Reconstr 3:37–44
Aronson J, Good B, Stewart C, Harrison B, Harp J (1990) Preliminary studies of mineralization during distraction osteogenesis. Clin Orthop Relat Res 250:43–49
Ilizarov GA (1989) The tension-stress effect on the genesis and growth of tissue: Part 1. The influence of stability of fixation and soft tissue preservation. Clin Orthop Relat Res 238:249–281
Cattaneo R, Villa A, Catagni M, Tentori L (1988) Limb lengthening in achondroplasia by Ilizarov's method. Int Orthop 12(3):173–179
Maffulli N, Pattinson RC, Fixsen JA (1993) Lengthening of congenital limb length discrepancy using callotasis: early experience of the hospital for sick children. Ann R Coll Surg Engl 75:105–110
Chew DK, Menelaus MB, Richardson MD (1998) Ollier's disease: varus angulation at the lower femur and its management. J Pediatric Orthop 18(2):202–208
Raimondo RA, Skaggs DL, Rosenwasser MP, Dick HM (1999) Lengthening of pediatric forearm deformities using the ilizarov technique: functional and cosmetic results. J Hand Surg 24A:331–338
Tsuchiya H, Morsy AF, Matsubara H, Watanabe K, Abdel-Wanis ME, Tomita K (2007) Treatment of benign bone tumors using external fixation. J Bone Joint Surg 89(B):1077–1783
Eralp L, Bilen FE, Rozbruch SR, Kocaoglu M, Hammoudi AI (2016) External fixation reconstruction of the residual problems of benign bone tumours. Strat Traum Limb Recon 11(1):37–49
Paley D (1990) Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop Relat Res 250:81–104
Liu J, Hudkins PG, Swee RG, Unni KK (1987) Bone sarcomas associated with Ollier's disease. Cancer 59:1376–1385
Schwartz HS, Zimmerman NB, Simon MA, Wroble RR, Millar EA, Bonfiglio M (1987) The malignant potential of enchondromatosis. J Bone Joint Surg Am 69:269–274
Richards SB, Cherkashin A, Samchukov M (2014) Varus deformity of the distal femur and LLD secondary to Ollier's disease corrected by gradual deformity correction and lengthening. In: Robert Rozbruch S, Hamdy Reggie (eds) Limb lengthening and reconstruction surgery case Atlas, pp 1–9. Springer International Publishing, Switzerland. https://doi.org/10.1007/978-3-319-02767-8_84-1
Funding
No benefits have been or will be received from a commercial party related directly or indirectly to the subject matter of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Angelini, A., Baracco, R., Dolci, A. et al. Limb lengthening for deformities in Ollier’s disease: a systematic review. Eur J Orthop Surg Traumatol 30, 1325–1332 (2020). https://doi.org/10.1007/s00590-020-02692-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-020-02692-5