Abstract
Purpose
Tibial-side avulsion injuries of the posterior cruciate ligament are rare injuries. In displaced fracture, the reduction and fixation is the treatment of choice, although the optimal surgical management has not yet been determined. The aim of this study was to evaluate the clinical, functional, and radiological outcome after an open reduction and internal fixation with staples of a posterior cruciate ligament tibial avulsion.
Methods
A historical cohort of patients who underwent open reduction and internal fixation with staple due to a posterior cruciate ligament tibial avulsion were reviewed. Minimum follow-up was 2 years. Demographic, clinical, and radiological data, including stress X-ray, were analyzed. Also, International Knee Documentation Committee Score, Tegner Knee Score, Lysholm Knee Score, Short-Form Health Survey, and four-point Likert scale were evaluated.
Results
Four males (57%) and 3 females (43%) were included in the final analysis. The mean age was 39 years (range 27–54). All patients had a fracture union. No implant migration was observed. Postoperative posterior drawer, reverse pivot shift, and varus/valgus stress were negative. In stress TELOS X-ray, no statistically significant differences were observed between the postoperative and contralateral knee. All evaluated scores had good or excellent results.
Conclusions
Our study provides further evidence that the use of an open reduction and internal fixation with a staple could be a simple and reliable management for posterior cruciate ligament avulsion fractures of the tibia. In our study, the postoperative stress TELOS X-ray analyze showed a correct fixation and biomechanical function of the posterior cruciate ligament.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Posterior cruciate ligament (PCL) is the stronger of the two cruciate ligaments of knee and have a major role in stabilizing the knee joint [1, 2]. Although, in countries like China and India in which motorcycle accidents are frequent, PCL bony avulsion fractures are usually considered rare injuries [3]. The general consensus is that surgical treatment of displaced tibial avulsion fractures of the PCL is regarded as necessary to achieve anatomic reduction, restore proper tension to the ligament and achieve knee stability, to prevent delayed osteoarthritis and permanent knee pain [1, 4, 5].
Several open surgical approaches and arthroscopic techniques have been described for treating these fractures [4, 5]. Although arthroscopic surgical fixation is more popular nowadays, open reduction is an acceptable procedure due to its safety, facility, direct visualization of the fracture site, and perfect anatomic reduction. Moreover, arthroscopic repair is technically more challenging, requires specialized equipment, and has a long learning curve, and the fracture fixation is potentially unstable [4, 6, 7]. On the other hand, there is a wide variety of materials available for internal fixation, including plates, staples, lag screws, steel wires, absorbable screws, suture anchors, and straddle nails [5, 8,9,10,11]. All these types of fixation have shown favorable results; however, the comminution of the fracture presented in the 50% of cases can make not only the reduction a difficult task but also the stable fixation [11]. Nowadays, none of the surgical managements has been considered a gold standard for avulsion fractures of the PCL [4, 5].
Stress radiography is a widely used diagnostic tool that provides objective quantification of knee ligament stability [12]. However, in the current literature, only several reports have use stress X-ray to measure the laxity of the PCL after this kind of surgery [2, 4, 7]. The aim of our study was to evaluate the clinical, functional, and radiological outcome after open reduction and internal fixation of tibial avulsion injuries of the PCL using staples. We hypothesized that by using an easily available implant and a simple approach a good clinical and functional outcome is obtained. Furthermore, a review of the literature of this disease and its surgical treatment has been performed.
Materials and methods
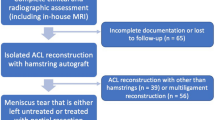
A retrospective case series study was performed. Institutional review board approval was obtained to retrospectively review patients who had undergone surgery because of a posterior cruciate ligament tibial avulsion between 2005 and 2012. Patients were identified through our institutional registry. The inclusion criteria were: (a) patients were aged > 18 and < 65 years. (b) Patients who had fracture displacement > 3 mm. (c) patients who underwent open fixation with staples. (d) Patients with acute fracture and surgery done in the first 4 weeks after the injury. (e) Patients with a minimum follow-up of 2 years. Patients with conservative treatment, chronic fractures, other type of fixation, or incomplete clinical data were excluded. Diagnosis in all patients was based on clinical, X-ray, CT, and MRI. These examinations allowed us to find associated knee injuries.
Surgical procedure
A single team of knee orthopedic surgery specialists (EC, JM) performed all surgeries. Under spinal/epidural anesthesia, a pneumatic tourniquet was placed around the thigh, and it was occasionally inflated. The patient was turned in prone position with the knee in mild flexion. Skin vertical incision was made over the posterior aspect of the knee with optional horizontal extension. We performed the posterior approach described by Burks and Schaffer [13]. Blunt dissection was done in the plane between the medial head of the gastrocnemius and semitendinosus down to the joint capsule. Subsequently, a partial disinsertion of the medial head of the gastrocnemius and retraction of the gastrocnemius laterally was done. The retraction of the gastrocnemius laterally allowed the protection of the neurovascular structures. Vertical incision was made through the capsule, exposed the bony structures of the knee, including the tibial attachment of the PCL. With a direct visualization of the fracture, an anatomy reduction and an internal fixation with one or two staples were performed. Two staples were used in the cases when we observed, intraoperatively, bone fragments that were not stabilized correctly with only one staple. In some patients, the surgery treatment of additional lesion was done in the same surgery or in a two-stage operations.
Postoperatively, all patients started the same physical rehabilitation program. In the first 6-week phase, patients were immobilized with a blocked orthosis in extension and a limited weight bearing were allowed. Also isometric contractions, emphasized on quadriceps and hamstring stretching, were done. In the second phase, patients started full weight bearing and passive and active range motion exercises were performed. By the third month, when consolidation of the fracture and stability of the knee was observed, the orthosis was removed. Clinical and union assessment by X-ray was done in all cases by knee orthopedic surgery specialist.
Follow-up and outcome measures
Patient’s demographic, clinical, and radiological data were collected preoperatively, postoperatively, and during the follow-up period (1, 3, 6, 12, and 24 months postoperatively). The latest data from each patient were used for analysis. Demographic and clinical data included: patient’s age at the time of surgery, gender, injury mechanism, range of motion, and ligament instability assessed using the posterior drawer test, varus–valgus stability test at 30° knee flexion and reverse pivot-shift test on both knees. In addition, at final follow-up, the subjective International Knee Documentation Committee (IKDC) Score (0–100; < 65 = poor, 65–83 = fair, 84–90 = good; > 90 = excellent), the Lysholm Knee Score (0–100; < 65 = poor, 65–83 = fair, 84–90 = good; > 90 = excellent), and the Tegner Knee Score (0–10; 0 = on sick leave/disability) were collected. To assess quality of life and patient satisfaction at final follow-up, we used the Short-Form Health Survey (SF-36) questionnaire (0–100) and the five-point Likert scale (very unsatisfied, unsatisfied, neutral, satisfied, and very satisfied). The four physical SF-36 components (physical functioning, role limitations due to physical health, bodily pain, and general health) and the four mental components (vitality, social functioning, role limitations due to emotional problems, and mental health) along with their respective summary components were calculated. All scores were measured by the same observer, a knee orthopedic surgery specialist (DM).
Radiological analysis included an anterior–posterior and a lateral X-ray in the healthy and injured knee. After 12 months, a comparative stress X-ray were performed. The first radiograph was a lateral decubitus X-ray with the knee in 90° of flexion, and the second X-ray was in the same position with the applied of a 20 kPa in the anterior region of the proximal tibia by a Telos GAII (Telos, Weterstadt, Germany) as described by Margheritini et al. [14]. The measurement of the posterior displacement of the tibia was made with the anatomical references described by Jacobsen and Staubli on the femur [15]. Due to the interposition of the staples, it was not possible to use the reference in the tibia described by the authors. Two parallel lines were traced on the posterior cortex margins of the tibia, and measured the distance between the two lines (Fig. 1). A translation of more than 3 mm was considered pathological [15].
Radiographic measurement of the posterior displacement of the tibia. a Stress radiograph to assess the posterior translation of the tibial plateau. A line is drawn tangent to the medial tibial plateau. Next a line is drawn perpendicular to the tangent to the medial tibial plateau and passing through the posterior cortex of the tibia shaft. Subsequently, another line is drawn passing through the posterior aspect of medial femoral condyle. The posterior translation is then calculated by measuring the distance between the two perpendiculars drawn. b Postoperative anterior–posterior radiograph
Statistical analysis
Descriptive statistics were used to present the results by mean, median and range. The quantitative variable of displacement in the stress X-ray were compared between the injured knee and the contralateral healthy knee by the nonparametric Mann–Whitney U test. A boxplot diagram was used to represent the distribution of the cases with respect to the TELOS in the injured knee and the contralateral knee. Statistical analysis was conducted using IBM SPSS ver. 20.0 (IBM Corp., Armonk, NY, USA).
Results
Among 11 patients, only seven met our inclusion criteria and were available for analysis (Table 1). Undisplaced fractures were excluded (4 cases) because the indication for surgery in such cases is questionable. There were four males (57%) and three females (43%) with a mean age of 39.6 years (range 27–54 years) at the time of surgery. The mean follow-up was 41.4 months (range 25–97 months). The most common mechanism of injury was road traffic accident (58%) with a majority involving motorcycle accident, followed by fall (28%) and sports-related injury (14%). Four patients presented a comminution fracture (58%). Five cases had associated knee injuries like meniscal injury, open patellar fracture, tibial plate fracture, femoral shaft fracture, rupture of the anterior cruciate ligament (ACL), or rupture of the lateral collateral ligament (LCL).
Mean time between injury and surgery was 11.4 days (range 6–26). The fragment fixation was carried out with two staples in four patients and one staple in the remaining cases. In any case, there was an intraoperative complication. In the postoperative period, two patients presented complications: 1. The second patient, presented a complex regional pain at 4 postoperative weeks. 2. The seventh patient, who had also an ACL rupture and meniscal injury, presented an arthrofibrosis. This patient required arthrolysis under sedation 6 months after the intervention. She presented an improvement in flexion from 90° to 130°. Despite the complications, one year after surgery, all patients showed fracture union.
Clinical tests of posterior drawer, reverse pivot shift, and varus–valgus stress at 30° knee flexion were negative in all patients. The median and range of the different questionnaires were: IKDC: 88.2 (range 87.7–96.6), Lysholm: 91.5 (range 85–100), Tegner preoperative score: 5.6 (range 2–9) and postoperative score: 3.6 (range 2–5). The median in the quality of life questionnaire SF-36 was 89.2 (range 85.4–91.6), in the physical component 89.3 (range 86.9–91.7) and in the mental component 90.3 (range 85.7–94.6). Patient satisfaction score were very satisfied in five cases and satisfied in the remaining. Stress radiographic study with Telos GAII showed a median distance of 1.2 mm (range 0.2–1.4 mm) in the healthy knee and 1.1 mm (range 0.2–2.5 mm) in the injured knee (Table 2). In our series, a translation of more than 3 mm was not obtained in any patient. The boxplot shows the representation of all the cases of the injured knee and the contralateral knee. We can see the similarity between the injured knee and the contralateral knee group (Fig. 2).
Boxplot diagram of the stress radiographic study with Telos GAII. In the stress radiographic study with Telos GAII, when we compare the postoperative knee with the healthy contralateral knee, no pathological translation is observed. In our series, a translation of more than 3 mm was not obtained in any patient
Discussion
There are currently a variety of treatment approaches for PCL avulsion fractures; however, the optimal surgical management have not been determined yet [4, 5]. Stress radiography is a widely used diagnostic tool that provides an objective quantification of knee ligament stability, although in the current literature only several reports have used this tool to analyze the laxity of the PCL after this kind of surgery [2, 4, 7]. The aim of our study was to evaluate the clinical, functional, and radiological outcome after open reduction and internal fixation of tibial avulsion injuries of the PCL using staples.
A review of the literature on the subject reveals many clinical cases and short heterogeneous series [1,2,3, 6,7,8,9,10,11, 13, 16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31] (Table 3). Even the different approaches described [13], we used the posteromedial approach described by Burks and Schaffer in all patients without intraoperative complications. The direct visualization of the fracture site with this approach provides several advantages. Not only simplifies reduction and fixation of the fracture with staple, but also permits us to locate the staple perpendicular to the plane of the fracture, which is important for the success of the treatment [24]. In recent years, several publications have reported good results with arthroscopy, however, the current literature suggests that each surgical approach (open vs. arthroscopic) renders similar outcomes for patients with displaced tibial-sided PCL avulsion fractures [4, 6, 7]. It has been published that the most common reason to recommend the arthroscopic approach has been the complexity of classic approaches and the risk of injury to neurovascular structures in the popliteal region [4,5,6,7]. In our experience, the Burks and Schaffer approach avoids dissecting the neurovascular structures and allow to protect these structures by the muscle belly of the gastrocnemius, which is why we found that the risk of neurovascular injury is lower.
There is also a controversy regarding the ideal fixation method. Nowadays, a wide variety of devices for internal fixation have been reported [4, 6,7,8,9, 11, 16, 17]. Screw fixation has been the most common method used and has shown favorable results; however, the comminution of the fracture presented in more of the 50% of cases can make not only the reduction a difficult task but also the stable fixation [4, 11]. Conventional screws may not fix the fracture fragments firmly enough and can lead to fragmentation of the bones [11]. For that reason, some studies have used toothed plate or have combined screw with suture and anchor systems [3, 4, 11]. In our experience, the size of the fragments or the presence of comminution was not problems to achieve a correct reduction and a stable fixation with the use of staples. The size (8 or 11 mm) or number of staples (one or two) used to repair the fracture depended on the size and fragmentation of the fracture. At 1 year postoperative follow-up, all cases had a successful bone union. The complications in our series were an arthrofibrosis in a patient that have had several associated lesions and, another case with a complex regional syndrome in a patient who manifested pain prior to surgery on the ipsilateral foot and without a diagnosis of local injury. We believe that these complications are not related to the technique or surgical procedure. Moreover, these complications have been reported in other series [4].
The results of surgical treatment in our series were assessed with clinical and radiographic tests that demonstrated a competent PCL. Like some other studies reported, in our study the questionnaires of functional assessment, quality of life and patient satisfaction reported good or excellent scores [3, 6, 7, 10, 11, 13, 17, 18, 21, 23, 26, 29,30,31]. In our study, we have a two-point decrease in the median of the Tegner scale, which compares sports activity before and after the injury. We believe that this decrease may be related to the fear of suffering a new knee injury since the scores on the other functional scales (generic scale of quality of life, and patient satisfaction) are high. Posterior drawer and the reversed pivot shift were both negative in all our patients. These tests are the best clinical tests to detect the competence of the LCP and the joint competition with the posterolateral complex, respectively [4, 5]. It is important to assess the competence of the posterolateral complex due to its association in 60% of PCL lesions [4]. In our study, only one patient presented a joint lesion of the posterolateral complex. Our study differs from other studies because in most of the studies the competence of the fracture union is not evaluated with stress radiographs. To our knowledge, only 2 studies have used this method of evaluation [2, 7]. In our study, the stress radiographic demonstrated the competence of the LCP, with a posterior displacement difference of the tibia less than 2 mm compared with the contralateral knee.
One of the limitations of this study is the retrospective nature of our study as well as its relatively small sample size that might limit the scope of the findings reported here. Our series is short because it is a rare pathology in our environment. In our article, from the 26 articles reviewed, only 2 were done in an European country [17, 19]. Even, if we reviewed arthroscopic treatment of this injury, to our knowledge, only 2 reports in Europe were done [32, 33]. Moreover, nowadays in the literature, the biggest study only reported 31 patients [1]. It is important to highlight that our study is the biggest series of cases of patients with PCL tibial avulsion treated with staple fixation. Most all study have used screw fixation [4, 5]. We believe that a multicenter long-term follow-up of patients will needed to determine which approach and which methods of fixation is the best in the management of this injury.
In summary, our study provides further evidence that the use of an open reduction and internal fixation with staples could be a simple and reliable management of posterior cruciate ligament avulsion fractures of the tibia. In our study, the patients present good outcomes with no clinical instability and correct values of the tested scores. Also postoperative stress TELOS X-ray showed a correct fixation and biomechanical function of the posterior cruciate ligament.
References
Rezazadeh S, Solooki S, Aboulhasani S, Reza Vosoughi A (2011) Midterm results of open reduction and internal fixation of isolated posterior cruciate ligament avulsion fracture. Eur Orthop Traumatol 1:191–195. https://doi.org/10.1007/s12570-011-0045-y
Khatri K, Sharma V, Lakhotia D, Farooque K (2015) Posterior cruciate ligament tibial avulsion treated with open reduction and internal fixation through the burks and schaffer approach. Malays Orthop J 9:2–8. https://doi.org/10.5704/MOJ.1507.004
Abdelbadie A, Arafa MS (2017) Treatment of posterior cruciate ligament tibial avulsion by a minimally-invasive open posterior approach. Injury 48:1644–1649. https://doi.org/10.1016/j.injury.2017.05.032
Hooper PO 3rd, Silko C, Malcolm TL, Farrow LD (2018) Management of posterior cruciate ligament tibial avulsion injuries a systematic review. Am J Sports Med 46:734–742. https://doi.org/10.1177/0363546517701911
Katsman A, Strauss EJ, Campbell KA, Alaia MJ (2018) Posterior cruciate ligament avulsion fractures. Curr Rev Musculoskelet Med 11:503–509. https://doi.org/10.1007/s12178-018-9491-2
Sabat D, Jain A, Kumar V (2016) Displaced posterior cruciate ligament avulsion fractures: a retrospective comparative between open posterior approach and arthroscopic single-tunnel suture fixation. Arthrosc J Arthrosc Relat Surg. https://doi.org/10.1016/j.arthro.2015.06.014
Pardiwala DN, Agrawal D, Patil V, Saini U, Dhawal P (2012) Paper 133: comparison of open versus arthroscopic fixation for isolated pcl tibial bony avulsions: a prospective randomized study with minimum 2 year follow-up. Arthroscopy 28:e413–e414. https://doi.org/10.1016/j.arthro.2012.05.616
Meyers MH (1975) Isolated avulsion of the tibial attachment of the posterior cruciate ligament of the knee. J Bone Joint Surg Am 57:669–672. https://doi.org/10.2106/00004623-197557050-00015
Torisu T (1977) Isolated avulsion fracture of the tibial attachment of the posterior cruciate ligament. J Bone Joint Surg Am 59:68–72
Joshi S, Bhatia C, Gondane A, Rai A, Singh S (2017) Open reduction and internal fixation of isolated posterior cruciate ligament avulsion fractures: clinical and functional outcome. Knee Surg Relat Res 29:210–216. https://doi.org/10.5792/ksrr.17.022
Chen W, Luo W, Chen Z, Jiang Y (2016) Treatment of posterior cruciate ligament avulsion fractures of the tibia using a toothed plate and hollow lag screw. Singapore Med J 57:39–44. https://doi.org/10.11622/smedj.2016010
James EW, Williams BT, LaPrade RF (2014) Stress radiography for the diagnosis of knee ligament injuries: a systematic review. Clin Orthop Relat Res 472:2644–2657. https://doi.org/10.1007/s11999-014-3470-8
Gavaskar AS, Karthik B, Gopalan H, Srinivasan P, Tummala NC (2017) Novel techniques A novel MIS technique for posterior cruciate ligament avulsion fractures. Knee 24:890–896. https://doi.org/10.1016/j.knee.2017.03.014
Margheritini F, Mancini L, Mauro CS, Mariani PP (2003) Stress radiography for quantifying posterior cruciate ligament deficiency. Arthroscopy 19:706–711. https://doi.org/10.1016/S0749-8063(03)00399-2
Staubli HU, Noesberger B, Jakob RP (1992) Stressradiography of the knee. Acta Orthop Scand 63:S2–S27. https://doi.org/10.3109/17453679209155044
Chiu FY, Wu JJ, Hsu HC, Lin L, Lo WH (1994) Management of avulsion injury of the PCL with reattachment. Injury 25:293–295. https://doi.org/10.1016/0020-1383(94)90238-0
Seitz H, Schlenz I, Pajenda G, Vécsei V (1997) Tibial avulsion fracture of the posterior cruciate ligament: K-wire or screw fixation? A retrospective study of 26 patients. Arch Orthop Trauma Surg 116:275–278. https://doi.org/10.1007/BF00390052
Chen CH, Chen WJ, Shih CH (1999) Fixation of small tibial avulsion fracture of the posterior cruciate ligament using the double bundles pull-through suture method. J Trauma 46:1036–1038. https://doi.org/10.1097/00005373-199906000-00009
Nikiforidis P, Babis G, Kateros K, Vlamis J, Korres DS (2000) Isolated avulsion fracture of the tibial attachment of the posterior cruciate ligament. Eur J Orthop Surg Traumatol 10:257–259. https://doi.org/10.1007/BF01682139
Yang C-K, Wu C-D, Chih C-J, Wei K-Y, Su C-C, Tsuang Y-H (2003) Surgical treatment of avulsion fracture of the posterior cruciate ligament and postoperative management. J Trauma 54:516–519. https://doi.org/10.1097/01.TA.0000047048.37775.32
Inoue M, Yasuda K, Kondo E, Saito K, Ishibe M (2004) Primary repair of posterior cruciate ligament avulsion fracture: the effect of occult injury in the midsubstance on postoperative instability. Am J Sports Med 35:1230–1237. https://doi.org/10.1177/0363546503262201
Zhang C, Xu H, Li MQ (2006) Posteromedial approach of gastrocnemius for reduction and internal fixation of avulsed tibial attachment of posterior cruciate ligament. Chin J Traumatol 9:25–28
Kashani FO, Mazloumi M, Ariamanesh A (2007) Fixation of tibial avulsion fractures of the posterior cruciate ligament using pull through suture and malleolar screw. J Res Med Sci 12:24–27
Nicandri GT, Klineberg EO, Wahl CJ, Mills WJ (2008) Treatment of posterior cruciate ligament tibial avulsion fractures through a modified open posterior approach: operative technique and 12- to 48-month outcomes. J Orthop Trauma 22:317–324. https://doi.org/10.1097/BOT.0b013e31817279d1
Jazayeri SM, Esmaili Jah AA, Karami M (2009) A safe postero-medial approach to posterior cruciate ligament avulsion fracture. Knee Surg Sport Traumatol Arthrosc 17:244–247. https://doi.org/10.1007/s00167-008-0665-0
Chiarapattanakom P, Pakpianpairoj C, Liupolvanish P, Malungpaishrope K (2009) Isolated PCl avulsion from the tibial attachment: residual laxity and function of the knee after screw fixation. J Med Assoc Thail 92:S181–S188
Ali M, Agrawal P, Katakdhond N, Arshadullah M (2011) Avulsion fracture of tibial insertion of PCL—operative management and outcome. Pulse 4:14–15. https://doi.org/10.3329/pulse.v4i1.6957
Bali K, Prabhakar S, Saini U, Dhillon MS (2012) Open reduction and internal fixation of isolated PCL fossa avulsion fractures. Knee Surg Sport Traumatol Arthrosc 20:315–321. https://doi.org/10.1007/s00167-011-1618-6
Chen W, Tang D, Kang L (2012) Effects of microendoscopy-assisted reduction and screw fixation through a single mini-incision on posterior cruciate ligament tibial avulsion fracture. Arch Orthop Trauma Surg 132:429–435. https://doi.org/10.1007/s00402-011-1426-y
Lamichhane A, Mahara DP (2012) Management of posterior cruciate ligament avulsion by cannulated screw fixation. J Inst Med 34:28–31
Zhang X, Cai G, Xu J, Wang K (2013) A minimally invasive postero-medial approach with suture anchors for isolated tibial avulsion fracture of the posterior cruciate ligament. Knee 20:96–99. https://doi.org/10.1016/j.knee.2012.10.016
Gwinner C, Hoburg A, Wilde S, Schatka I, Krapohl BD, Jung TM (2016) All-arthroscopic treatment of tibial avulsion fractures of the posterior cruciate ligament. GMS Interdiscip Plastic Reconstr Surg DGPW 5:1–7. https://doi.org/10.3205/iprs000081
Wajsfisz A, Makridis KG, Van Den Steene JY, Djian P (2012) Fixation of posterior cruciate ligament avulsion fracture with the use of a suspensory fixation. Knee Surg Sports Traumatol Arthrosc 20:996–999. https://doi.org/10.1007/s00167-011-1702-y
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No conflicts of interest were declared by the authors.
Rights and permissions
About this article
Cite this article
Reverte-Vinaixa, M.M., Nuñez, J.H., Muñeton, D. et al. Outcomes of posterior cruciate ligament tibial avulsion treated with staple fixation: stress TELOS X-ray evaluation. Eur J Orthop Surg Traumatol 29, 883–891 (2019). https://doi.org/10.1007/s00590-019-02371-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-019-02371-0