Abstract
Malunion is a common complication of distal radius fractures, especially those treated conservatively. In clinical studies, a significant correlation between anatomic reduction and wrist function has been shown. Corrective osteotomy is the preferred treatment for symptomatic cases, notwithstanding the technical challenges. The use of computer simulation improves pre-operative understanding of the three-dimensional deformity. Patient-specific surgical guides, based on precise pre-operative planning, lead to superior perioperative accuracy and reproducibility. The pre-operative planning and surgical technique of distal radius corrective surgery using three-dimensional computer technology are described in detail. The preliminary results demonstrate the excellent clinical and radiographic outcome of this technique.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The overall incidence of distal radius fractures is approximately 0.26% [1], and malunion is a common complication, occurring in approximately 5% of cases [2].
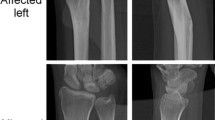
Patients with malunion of the distal radius can experience a myriad of clinical symptoms, such as wrist pain, crepitus in the radiocarpal joint, decreased range of motion, reduced grip strength, instability of the distal radio-ulnar joint, a cosmetic deformity and median nerve neuropathy (Fig. 1) [3,4,5,6,7,8,9,10,11,12,13]. In addition, intra-articular deformities of the distal radius with a step-off of more than 2 mm can lead to early posttraumatic osteoarthritis [10].
Clinical picture of a 17-year-old boy who sustained a complex distal radius fracture treated conservatively. On physical examination, forearm pro- and supination were restricted to 30° and 25°, respectively (a). Pre-operative radiographs showed pronounced three-dimensional deformity of the distal radius (b)
Clinical studies have shown a significant correlation between anatomic reduction and wrist function in patients with malunion [2, 3, 14]. For this reason, osteotomy of the distal radius to restore alignment in relation to the carpus and the distal ulna is the treatment of choice and often indicated in symptomatic patients.
Corrective osteotomies are technically challenging procedures, especially when multiplanar extra- and/or intra-articular deformity is present. Rotational and intra-articular deformities are difficult to assess on two-dimensional plain radiographs [15], and the use of three-dimensional computer simulation and patient-specific guides makes it more feasible to address these problematic malunions.
Pre-operative planning
High-resolution bilateral computed tomography (CT) scans of the forearm are obtained (slice thickness 0.4 mm, slice increment 0.2 mm, pixel size 0.29 mm, 120 kVp). The CT-generated DICOM images are loaded into medical image processing software (Mimics Medical or Mimics InPrint, Materialise NV, Technologielaan 15, 3001 Leuven, Belgium) to convert them into three-dimensional bony models (STL files) of the radius and ulna. These STL files can be manipulated virtually on the computer, allowing precise assessment of the deformity and planning of corrective surgery.
A mirrored version of the normal contralateral side is superimposed on the malunited radius, providing a comprehensive three-dimensional assessment of the distal radius deformity (Fig. 2).
Subsequently, a virtual correction of the present deformity is planned in a CAD program (3-Matic, Materialise NV, Technologielaan 15, 3001 Leuven, Belgium) following a number of steps: (1) definition of the osteotomy plane, (2) simulation of the osteotomy, (3) correction of the distal radius part toward the mirrored contralateral side and (4) selection and positioning of the most appropriate fixation plate and screws (Fig. 3). During these steps, bone loss due to the saw blade thickness is taken into account. Besides precise correction of distal radius alignment, restoration of normal ulnar variance and a congruent DRUJ are checked.
To allow reproduction of the virtual osteotomy in the operating room, patient-specific surgical guides are designed with reversed engineering (Fig. 4a). The corrected bony parts and the corresponding screws trajectories are transferred back to the original position. Based on the previous steps, a patient-specific cutting and drill guide are designed, which are compatible with the standard instruments of a distal radius plating system.
In addition to the patient-specific guides, anatomic models of the native malunited and planned post-operative radius are 3D-printed to further assist the surgeon and make sure that the virtual planning is transferred correctly to the patient.
All models are labeled with a unique code and are three dimensionally printed in ‘European Commission’ (CE) or ‘Food and Drug Administration’ (FDA) certified medical grade material (polyamide) and are sterilized prior to surgery.
Surgical technique
In most of our cases, a standard volar approach is used, according to Arnold K. Henry [16], but other approaches can be used when more appropriate.
The patient-specific drilling guide is closely fit onto the volar surface of the distal radius at the exact predetermined location and secured with K-wires. It is evident that exact positioning of the guide is essential to obtain the planned correction, and fluoroscopy as well as the printed bone model can be used to confirm this.
Using the drilling guide, all the trajectories for later screw insertion are predrilled into the bone of the distal radius. Next, the drill guide is removed and replaced by the cutting guide, over the retained K-wires. A bone saw is used to perform the osteotomy at the correct site and along the pre-planned plane. In most cases, the brachioradialis tendon is released distally to facilitate correction and later bone graft insertion.
A standard or, when more appropriate, a 3D printed custom-made plate is fixed with locking screws into the predrilled holes of the distal fragment first. Subsequently, the proximal part of the plate is fixed with cortical screws into the shaft of the radius. Autologous iliac crest or allograft bone graft is used to fill the defect at the osteotomy site.
When deemed necessary, an arthroscopic procedure can be associated with check anatomic reduction of intra-articular fragments.
Post-operative management
The post-operative management depends on the type of deformity and correction as well as the bone quality and fixation method. A splint is provided for the first 2 weeks, followed by a circular cast or removable brace for another 4 weeks. After cast removal, patients can start active and passive range of motion exercises. Clinical and radiographic follow-up is arranged every 4 weeks until complete bony union and maximal return of function is obtained.
Preliminary results
Thirty patients who had correction of an extra-articular or combined intra- and extra-articular deformity of the distal radius were reviewed prospectively. All included subjects were treated with a three-dimensional corrective osteotomy between October 2009 and March 2014. The mean age at the time of surgery was 49 years (range 15–78 years). Seventy-three percent of the patients were women, and 53% of the treated wrists were nondominant. This study has been approved by the appropriate ethics committee and has therefor been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Range of motion and grip strength was assessed in all patients. The Visual Analogue Score (VAS) for pain and the Disability of the Arm, Shoulder, and Hand (DASH) questionnaire were used to measure patient-rated functional outcome, residual disabilities and pain.
At 1-year follow-up, all patients showed an improvement in wrist function. On average, range of motion improved with 18° of wrist flexion, 11° of wrist extension, 12° of forearm pronation and 15° of forearm supination. The grip strength increased with 41% post-operatively, with a remaining difference of minus 22% compared to the contralateral side.
All patient experienced pain before surgery, with a mean VAS of 5. After the three-dimensional corrective osteotomy, pain decreased to a VAS of 2. The mean DASH score decreased from 46 to 17.
One patient developed an acute median nerve neuropathy post-operatively and underwent an open carpal tunnel release. One patient experienced a rupture of the extensor pollicis longus (EPL) tendon, successfully treated with a tendon transfer. No major complications, such as infection or nonunion, were observed.
In addition to the excellent clinical results, the radiographical results and the achieved correction were satisfactory (Fig. 4b). The goal was to restore radial angulation to within 5° of the predetermined planning and ulnar variance to within 2 mm. This was achieved in 22 (73%) patients, and there were no outliers (> 10° difference between planned and final radiographic correction).
Discussion
We prospectively reviewed thirty patients, treated with a 3D assisted corrective osteotomy of the distal radius, and found an overall improvement of wrist function, grip strength, and pain. Moreover, the patient-rated DASH score improved significantly, and no major residual complications have been observed at 1-year follow-up. Radiographic evaluation confirms better outcomes compared to the reported results with conventional techniques [4].
No literature is available that directly compares the results of 3D assisted techniques with more conventional planning techniques [15]. However, there is evidence that especially complex deformities and intra-articular malunions of the distal radius will benefit from three-dimensional simulation and the use of patient-specific guides [6, 13, 15].
The use of fluoroscopy is limited to checking the position of the guide and a final control at the end of the procedure, therefore limiting radiation exposure of the patient and the surgical team compared to conventional techniques.
Disadvantages of the three-dimensional technique include the use of specialized computer programs, radiation exposure during CT scanning, the time and effort needed for pre-operative planning and the extra cost of custom-made surgical guides [8, 15]. In addition, the complication rate found in literature is as high as 16% [15].
Further investigation and development are necessary to define the added value of three-dimensional technology and to lower the associated costs. As an important factor to explain the cost of using this technology lies in the man-hours needed for planning the procedure and designing the patient-specific instruments, further automatization of these processes may decrease the cost.
Conclusion
Although the added value of three-dimensional simulation and the use of patient-specific guides remains to be confirmed, our experience confirms that three-dimensional technology facilitates restoration of normal anatomy, especially in complex deformities of the distal radius [13, 15]. It allows more accurate and reproducible correction compared to conventional techniques, and it reduces surgical time and radiation exposure. It is therefore now routinely used within our unit for the correction of upper limb malunions, not limited to the distal radius.
References
Brogren E, Petranek M, Atroshi I (2007) Incidence and characteristics of distal radius fractures in a southern Swedish region. BMC Musculoskelet Disord 8:1–8. https://doi.org/10.1186/1471-2474-8-48
Cooney WP, Dobyns JH, Linscheid RL (1980) Complications of Colles’ fractures. J Bone Jt Surg 62(4):613–619
Fernandez DL (1982) Correction of post-traumatic wrist deformity in adults by osteotomy, bone-grafting, and internal fixation. J Bone Jt Surg Am Vol 64A(8):1164–1178
Von Campe A, Nagy L, Arbab D, Dumont CE (2006) Corrective osteotomies in malunions of the distal radius: do we get what we planned? Clin Orthop Relat Res 450:179–185. https://doi.org/10.1097/01.blo.0000223994.79894.17
Krukhaug Y, Hove LM (2007) Corrective osteotomy for malunited extra-articular fractures of the distal radius: a follow-up study of 33 patients. Scand J Plast Reconstr Surg Hand Surg 41(6):303–309. https://doi.org/10.1080/02844310701445610
Oka K, Moritomo H, Goto A, Sugamoto K, Yoshikawa H, Murase T (2008) Corrective osteotomy for malunited intra-articular fracture of the distal radius using a custom-made surgical guide based on three-dimensional computer simulation: case report. J Hand Surg 33(6):835–840. https://doi.org/10.1016/j.jhsa.2008.02.008
Leong NL, Buijze GA, Fu EC, Stockmans F, Jupiter JB (2010) Computer-assisted versus non-computer-assisted preoperative planning of corrective osteotomy for extra-articular distal radius malunions: a randomized controlled trial. BMC Musculoskelet Disord. https://doi.org/10.1186/1471-2474-11-282
Miyake J, Murase T, Moritomo H, Sugamoto K, Yoshikawa H (2011) Distal radius osteotomy with volar locking plates based on computer simulation. Clin Orthop Relat Res 469(6):1766–1773. https://doi.org/10.1007/s11999-010-1748-z
Buijze GA, Prommersberger KJ, González Del Pino J, Fernandez DL, Jupiter JB (2012) Corrective osteotomy for combined intra- and extra-articular distal radius malunion. J Hand Surg 37(10):2041–2049. https://doi.org/10.1016/j.jhsa.2012.07.013
Schweizer A, Fürnstahl P, Nagy L (2013) Three-dimensional correction of distal radius intra-articular malunions using patient-specific drill guides. J Hand Surg 38(12):2339–2347. https://doi.org/10.1016/j.jhsa.2013.09.023
Kunz M, Ma B, Rudan JF, Ellis RE, Pichora DR (2013) Image-guided distal radius osteotomy using patient-specific instrument guides. J Hand Surg 38(8):1618–1624. https://doi.org/10.1016/j.jhsa.2013.05.018
Dobbe JGG, Vroemen JC, Strackee SD, Streekstra GJ (2014) Patient-specific distal radius locking plate for fixation and accurate 3D positioning in corrective osteotomy. Strateg Trauma Limb Reconstr 9(3):179–183. https://doi.org/10.1007/s11751-014-0203-1
Stockmans F, Dezillie M, Vanhaecke J (2013) Accuracy of 3D virtual planning of corrective osteotomies of the distal radius. J Wrist Surg 2(212):306–314. https://doi.org/10.1055/s-0033-1359307
Villar RN, Marsh D, Rushton N, Greatorex RA (1987) Three years after Colles’ fracture. A prospective review. J Bone Jt Surg Am Vol 69(4):635–638. https://doi.org/10.1016/0268-0033(88)90160-X
de Muinck Keizer RJO, Lechner KM, Mulders MAM, Schep NWL, Eygendaal D, Goslings JC (2017) Three-dimensional virtual planning of corrective osteotomies of distal radius malunions: a systematic review and meta-analysis. Strateg Trauma Limb Reconstr. https://doi.org/10.1007/s11751-017-0284-8
Conti Mica MA, Bindra R, Moran SL (2017) Anatomic considerations when performing the modified Henry approach for exposure of distal radius fractures. J Orthop 14(1):104–107. https://doi.org/10.1016/j.jor.2016.10.015
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Verstreken has a patent with Materialise with royalties paid. The other authors have no conflicts of interest to report.
Rights and permissions
About this article
Cite this article
Michielsen, M., Van Haver, A., Bertrand, V. et al. Corrective osteotomy of distal radius malunions using three-dimensional computer simulation and patient-specific guides to achieve anatomic reduction. Eur J Orthop Surg Traumatol 28, 1531–1535 (2018). https://doi.org/10.1007/s00590-018-2265-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-018-2265-0