Abstract
Objectives
With the increasing number of primary anterior cruciate ligament (ACL) reconstructions, the need for revision ACL surgery has risen over the past few years. The purpose of the present study is to retrospectively compare the clinical outcome of ipsilateral versus contralateral hamstring tendon autografts for ACL revision surgery, specifically with regard to patient satisfaction, post-operative functional outcomes, and return to sports.
Methods
Between 2004 and 2011, 64 patients underwent ACL revision surgery. Forty-five were successfully recontacted and retrospectively reviewed at an average follow-up of 6.3 years. Twenty-two subjects underwent revision ACL reconstruction with ipsilateral autogenous hamstring tendon grafts; in 23 subjects contralateral hamstring were used for reconstruction. Clinical, arthrometric, and functional evaluations were performed. The Tegner activity level, Knee Injury and Osteoarthritis Outcome Score (KOOS), and International Knee Documentation Committee (IKDC) Subjective Knee Form were used. Objective evaluation included range of motion, Lachman test, pivot shift test and KT-1000 instrumented laxity testing.
Results
No major complications were reported. Follow-up examination showed that there were no significant differences in the IKDC and KOOS scores between the groups. No differences in anterior tibial translation as measured with KT-1000 arthrometer were reported between the groups, although there was a trend for more of the patients undergoing ipsilateral DGST reconstruction to have a glide on the pivot shift test. The percentage of patients returning to pre-injury level was high in both groups.
Conclusions
The use of contralateral hamstring tendon autografts for ACL revision surgery produced similar subjective and objective outcomes at 6-years follow-up compared to revision with ipsilateral hamstring tendon autografts. Patients undergoing revision surgery with contralateral autografts experienced a quicker return to sports compared to patients who underwent ipsilateral DGST revision surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Revision anterior cruciate ligament (ACL) surgery is recommended for patients who have symptomatic objective patholaxity after a failed primary ACL reconstruction. The number of revision ACL surgery has risen over the past few years [1].
The choice of graft in revision surgery remains a debatable issue. Autografts constitute a popular choice as many authors recommend autografts for both primary and revision ACL reconstructions [2–7]; the bone–patellar tendon–bone (BPTB) is frequently used as preferred graft source for ACL reconstruction in case of hamstring failure and vice versa [8].
Post-operative donor-site morbidity and anterior knee pain following ACL surgery may result in substantial impairment for patients. Intraoperative injury to the infrapatellar nerve can lead to donor-site discomfort and kneeling impairment [9].
To minimize donor-site morbidity in a previously operated knee, contralateral doubled gracilis and semitendinosus tendons graft (DGST) or BPTB have been proposed as a viable option for ACL revision surgery [8, 10].
The aim of this study is to compare the clinical outcome of ipsilateral hamstring tendon autografts versus contralateral DGST for ACL revision surgery, specifically with regard to patient satisfaction, activity level, and post-operative functional outcomes.
Patients and methods
Patients recruitment
Between 2004 and 2011, 64 patients who had previously primary ACL BPTB reconstruction underwent revision ACL surgery at the Minimally Invasive Articular Surgery Unit of the G. Pini Orthopaedic Institute of Milan.
Forty-five of them were successfully recontacted and retrospectively reviewed at an average follow-up of 6.3 years (range 2–9 years). Inclusion criteria were failed primary ACL reconstruction using a BPTP graft, confirmed by recurrence of giving-way episodes as revealed by a positive Lachman and pivot shift tests. Exclusion criteria were multiligamentous incompetence, contralateral instability or other significant knee disease, severe chondral damage (grade 3 or 4 of the Outerbridge classification system), or degenerative arthritis (Ahlback grade 3 or 4).
In most subjects (87%), ACL re-injury resulted from noncontact or indirect contact mechanisms. All other patients experienced a direct contact injury.
Twenty-two subjects underwent revision ACL reconstruction with ipsilateral autogenous hamstring tendon grafts; in 23 subjects contralateral hamstring were used for reconstruction. The median time since the first reconstruction was 45 months (range 18–142) in the ipsilateral tendon group and 40 months (range 20–128) in the contralateral tendon group. Table 1 shows complete demographic and anthropometric data.
Written informed consent was obtained. The study was conducted according to the guidelines expressed by the Ethical Committee of the Institute.
Surgical technique of ipsilateral DGST reconstruction
Preliminary arthroscopic inspection was performed in order to confirm the diagnosis. Patients were excluded from the study when intraoperative findings did not match inclusion criteria.
Hamstring tendon autografts were harvested from the ipsilateral knee with a tendon stripper through an incision over the pes anserinus on the AM aspect of the tibia and then prepared to form a 4-stranded replacement graft. The tibial and femoral tunnels were drilled with an arthroscopically assisted transtibial technique. After the remnants of the torn ACL were removed, the tibial tunnel was drilled with the aid of a guide (Acufex; Smith & Nephew, Andover, MA) at a 55 angle in the horizontal plane on the tibial plateau. The femoral tunnel was then drilled with the knee flexed from 90 to 120 in the intercondylar notch posterior and lateral on the medial aspect of the lateral femoral condyle to a depth of 30 mm and a diameter matched to the width of the prepared graft, at the 11 o’clock position in a right knee and at the 1 o’clock position in a left knee. Then, the graft was fixed proximally with the use of a TightRope device (Arthrex, Naples, FL). Distal locking was achieved through a BioRCI screw (Bioadsorbable Rounded Cannulated Interference; Smith & Nephew), having a diameter 1 or 2 mm larger than that of the graft, while the knee was kept at 20 of flexion under maximal manual tension.
Surgical technique of contralateral DGST reconstruction
Operations were carried out in the same way with the exception that hamstring tendon autografts were harvested from the contralateral knee.
Rehabilitation protocol
For the first 4 weeks, walking with partial weight bearing was allowed with the use of 2 crutches. Patients were encouraged to regain proprioception with the use of a balance board and complete knee flexion and extension. Closed kinetic chain exercises were performed for the first 3 months, and thereafter, open kinetic chain exercises were started. Swimming and indoor cycling were permitted after 12 weeks, jogging and noncontact sports were permitted after 5 months, and a return to contact sports was allowed after 6 months.
Follow-up assessment
Patients were evaluated pre-operatively and after an average follow-up of 6.3 years (range 2–9 years). Assessment included Knee Osteoarthritis Outcome score (KOOS), International Knee Documentation Committee (IKDC) Subjective Knee Form, Tegner activity level, and objective examination including instrumented laxity test with KT-1000 arthrometer (MEDmetric Corporation, San Diego, CA, USA) under a 134-N anterior tibial load. Patients’ evaluations were performed by the same equipe.
Statistical analysis
Data extracted were analyzed using the program SPSS version 19.0 (SPSS Inc., Chicago, IL, USA). Wilcoxon test was utilized to compare the pre-operative and follow-up status and the difference between the two groups. Differences with a p value <0.05 were considered statistically significant.
Results
No cases of infection, deep thrombosis, neurovascular injury, or any other major complications were reported.
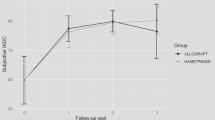
Subjectively, all patients were satisfied with their revision ACL reconstruction. The mean overall KOOS score increased (p < .001) from a pre-operative mean of 61.8 (SD 9.4) to 84.9 (SD 6.7), showing a statistically significant difference (p < .001). IKDC subjective score improved from 29.2 (SD 10.4) to 81.1 (SD 6.4) (p < .001). The median Tegner activity rating significantly improved (p < 0.001) from a pre-operative mean of 6.5 (range 4–10) to 7.5 (range 7–10). The outcomes of clinical assessment regarding Lachman test and pivot shift sign were clearly improved when compared with pre-operative status. The mean side-to-side KT-1000 value was 1.8 mm (SD 2.4). Of the patients, 43 (96%) reported a value equal to or less than 3 mm compared with the contralateral knee. Thirty of 45 (67%) achieved a return to pre-primary ACL reconstruction activities. A detailed overview of the results of overall clinical assessment is shown in Table 2.
The differences in the outcomes between the two groups are reported in Table 3. Using Wilcoxon test, there was no significant difference for subjective scores and activity level between the two groups with regards to point scales (p = n.s.). The percentage of patients returning to pre-injury level was high in both group; 58% of patients returned to cutting and pivoting sports, (Table 4). Anterior tibial translation according to manual laxity testing and as measured with KT-1000 arthrometer was not statistically different in the two groups (p = n.s.). With regards to return to sports, patients undergoing revision surgery with contralateral autografts experienced a quicker return to sports compared to patients who underwent ipsilateral DGST revision surgery.
No subjective loss of motion or strength of the contralateral knee, rotational injuries following tendon harvesting nor long-term significant morbidity at follow-up was reported.
Discussion
The use of contralateral hamstring tendon autografts for ACL revision surgery produced similar subjective and objective outcomes at 6.3-year follow-up compared to revision with ipsilateral hamstring tendon autografts. Patients undergoing revision surgery with contralateral DGST autografts experienced a quicker return to sports compared to patients who underwent ipsilateral DGST revision surgery. Both surgical techniques led to good results with improvement in knee stability and knee score values.
The present study shows favorable results for revision ACL reconstruction concerning subjective knee function and knee stability as well as ability to resume sport activities. Results are comparable to the most satisfactory outcomes reported in literature [1, 8].
Subjectively all patients reported that they would have the surgery again and were satisfied compared with their pre-revision status. After an average time of 6 years from surgery, mean KOOS was 84.9, while subjective IKDC score was 81.1.
No donor-site discomforts were reported by patients in our case series. Temporary loss of anterior sensitivity was reported in two patients 1 year after surgery, but recovered at follow-up. None of the patients experienced subjective loss of motion or strength of the contralateral knee or long-term significant morbidity at follow-up.
Our study shows no statistically significant differences with regards of knee stability between the two groups in ACL revision surgery. There was a trend for more of the patients undergoing ipsilateral DGST reconstruction (14%) to have a glide on the pivot shift test compared with the other cohort of patients (4%).
Shelbourne et al. [11] reported a rate to return to sports ranging from 62 to 74% in sportsmen who underwent revision ACL reconstruction with a patellar tendon autograft.
In our case series, 67% of patients were able to return to their pre-primary level of activity and sport. This result is in line with that of other studies with similar follow-up [12]. Revision ACL reconstruction either with ipsilateral or contralateral grafts may therefore be one possible option in patients with recurrent knee instability following primary repair who wish to return to their pre-injury activity level.
Patients undergoing revision surgery with contralateral autografts experienced a quicker return to sports compared to patients who underwent ipsilateral DGST revision surgery.
This may be explained since an ACL-reconstructed knee which is not affected by donor-site morbidity experiences a less aggressive surgical procedure. In fact, by harvesting hamstring from the contralateral limb, donor-site pain is shifted to the healthy side and allows the knee which is subjected to ACL reconstruction to an easier rehabilitation.
Therefore, reharvesting hamstring tendons in a previously ACL-reconstructed knee using patellar tendon may result in delayed return to sports compared to revision with contralateral hamstrings.
Limitations of the present study include the relatively small sample size. The limited study population may not have allowed for detection of small differences between groups regarding some parameters. A greater number of patients in each group could have enhanced the statistical significance of the results obtained.
Conclusions
The use of contralateral hamstring tendon autografts for ACL revision surgery produced similar subjective and objective outcomes at 6-year follow-up compared to revision with ipsilateral hamstring tendon autografts. Patients undergoing revision surgery with contralateral autografts experienced a quicker return to sports compared to patients who underwent ipsilateral DGST revision surgery.
References
Kamath GV, Redfern JC, Greis PE, Burks RT (2011) Revision anterior cruciate ligament reconstruction. Am J Sports Med 39:199–217
Colosimo AJ, Heidt RS Jr, Traub JA, Carlonas RL (2001) Revision anterior cruciate ligament reconstruction with a reharvested ipsilateral patellar tendon. Am J Sports Med 29:746–750
Kamath GV, Redfern JC, Greis PE, Burks RT (2011) Revision anterior cruciate ligament reconstruction. Am J Sports Med 39:199–217
Kartus J, Stener S, Lindahl S, Eriksson BI, Karlsson J (1998) Ipsi or contralateral patellar tendon graft in anterior cruciate ligament revision surgery. A comparison of two methods. Am J Sports Med 26:499–504
Noyes FR, Barber-Westin SD (2001) Revision anterior cruciate surgery with use of bone-patellar tendon-bone autogenous grafts. J Bone Joint Surg Am 83-A:1131–1143
Garofalo R, Djahangiri A, Siegrist O (2006) Revision anterior cruciate ligament reconstruction with quadriceps tendon-patellar bone autograft. Arthroscopy 22:205–214
Noyes FR, Barber-Westin SD (2006) Anterior cruciate ligament revision reconstruction: results using a quadriceps tendon-patellar bone autograft. Am J Sports Med 34:553–564
Ferretti A, Monaco E, Caperna L, Palma T, Conteduca F (2013) Revision ACL reconstruction using contralateral hamstrings. Knee Surg Sports Traumatol Arthrosc 21:690–695
Kartus J, Magnusson L, Stener S, Karlsson J (1999) Complications following arthroscopic anterior cruciate ligament reconstruction. A 2–5-year follow-up of 604 patients with special emphasis on anterior knee pain. Knee Surg Sports Traumatol Arthrosc 7:2–8
Rubinstein RA Jr, Shelbourne KD, Van Meter CD, McCarroll JC, Rettig AC (1994) Isolated autogenous bone-patellar tendon-bone graft side morbidity. Am J Sports Med 22:324–327
Shelbourne KD, Benner RW, Gray T (2014) Return to sports and subsequent injury rates after revision anterior cruciate ligament reconstruction with patellar tendon autograft. Am J Sports Med 42:1395–1400
Peterson RK, Shelton WR, Bomboy AL (2001) Allograft versus autograft patellar tendon anterior cruciate ligament reconstruction: a 5-year follow-up. Arthroscopy 17:9–13
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Legnani, C., Peretti, G., Borgo, E. et al. Revision anterior cruciate ligament reconstruction with ipsi- or contralateral hamstring tendon grafts. Eur J Orthop Surg Traumatol 27, 533–537 (2017). https://doi.org/10.1007/s00590-016-1894-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-016-1894-4