Abstract
Introduction
Nonunions after operative fixation of the femur, although infrequent, remain a challenge for orthopedic surgeons. The aim of this study was to assess the effectiveness of double locking plate fixation in the treatment for femoral shaft nonunions.
Materials and methods
From 2009 to 2013, 21 patients with femoral nonunions (mean age 46.9 years, range 25–81) were treated and evaluated utilizing double locking plate fixation. Patients were followed for at least 6 months postoperatively or until they achieved complete union to investigate bone healing and functional outcomes in femoral shaft nonunions treated with double locking plate and autogenous cancellous bone graft.
Results
The main outcomes evaluated were the presence of bony union, time to achieve union, and SF-36 score. All 21 femoral nonunions healed (100 % union rate). The average time to bony union was 5.3 months (range, 4–7). The mean follow-up duration time was 24.8 months (range, 6–60). Average scores of the physical function and bodily pain components of the SF-36 were 96 (range, 90–99) and 94.2 (range, 92–99), respectively. No significant complications were noted postoperatively.
Conclusion
Because of the high union rates and lack of significant complications in our series, double locking plate fixation can serve as an effective method of addressing femoral shaft nonunions. No significant complications were found postoperatively.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although surgical stabilization of femoral shaft fractures has become very successful with current treatment modalities, nonunions can result and can lead to pain, loss of function, deformity, and other complications [1–3]. Various treatment modalities exist to address femoral shaft nonunions, which include nail dynamization, exchange nailing, plate fixation, bone grafting, Ilizarov technique, and combinations thereof. Despite the success rates reported in the literature for these revision techniques, each methodology has its own set of complications and failures. Although reported failure rates of Ilizarov external fixation for long bone nonunions are less than 6 %, they often require prolonged use (which can lead to pin tract infections, subjective inconvenience, and discomfort) [4, 5]. While most surgeons are more familiar and comfortable with revision intramedullary nailing, complication rates are higher, as reported in the literature [6]. Some studies have reported a 27 % complication rate of failure for intramedullary nailing (range 0–67 %) as compared to 18 % for plate fixation (range 0–30 %). Reported union rates also favor plate fixation, with union rates of 96 % for plate fixation (range 91–100 %) as compared to 75 % for IM nailing (range 56–100 %) [7–15].
Despite the reported success rates of plate fixation with autogenous bone grafting, [16, 17] success is influenced by technique. It does require significant dissection which, when poorly performed, can lead to suboptimal results. Furthermore, success is influenced by significant bone defects, poor bone quality, and osteoporosis. Additionally, in torsional wedge nonunion patterns (AO classification type 32-B/32-C), single-plate fixation may be a suboptimal construct. Absolute stability is difficult to achieve in these instances and can leave a residual gap that makes standard single compression plating prone to failure should healing not occur quickly.
Because of these limitations, we are trying to use a double plate construct for femoral nonunions. In addition to addressing the mechanical need for successful nonunion repair, addition of autogenous cancellous bone would also address the biological need for successful nonunion repair. Double plating can potentially be used to address femoral nonunions with bone loss (i.e., lack of good cortical contact), where nailing (i.e., small canal, presence of previous hardware blocking canal access) and Ilizarov are not viable options. Utilizing such techniques can allow maintenance of length, alignment, and rotation, while permitting bone grafting and early weight-bearing. In this study, we assess the results and outcomes of double locking plate constructs and autogenous cancellous bone graft for the treatment for femoral shaft nonunions.
There are widespread controversies about nail or plate or both for femur union revision. Nail or plate revision for femur shaft nonunion showed different union rate (Table 1) [8, 9, 11, 12, 14, 18–27]. Double locking plate fixation can be used for long bone nonunion and with great results in previous studies [28–30]. Murray et al. use it for long bone nonunion and got 94.1 % union rate in 1964. Parker et al. use it for tibial shaft nonunion and got 100 % union rate in 1974. Martinez et al. use it for humeral shaft nonunion and got 100 % union rate in 2009. The previous studies of exchange nail showed that the union rate is unstable (range 53–96 %). The union rate of double plate is more stable than exchange nail and higher than 90 %. That means exchange nails should have second or third revisions but double plate should not. That may cost additional medical fees and increase patients’ psychological burden. In this study, we theorize that the use of locking plates can further enhance biomechanical stability (absolute stability) and lead to more stable successful results (defined as adequate bony union) with low complication rates.
Materials and methods
We retrospectively reviewed all of our femoral shaft fracture cases presenting with a nonunion, with documented cutaneous temperature, white blood cell count, C-reactive protein levels, and erythrocyte sedimentation rates to exclude infection. Cases that were included in the study required documentation of pathological examination at the nonunion site during the revision to verify that it was an aseptic nonunion. We defined “nonunions” according to the US Food and Drug Administration (FDA) criteria, where a fracture that is at least 9 months old and has not shown any signs of healing for three consecutive months [31, 32]. We also did the CT scan to confirm the nonunion.
The inclusion contains adult femur shaft closed fracture with internal fixation and nonunion. The exclusion criteria contain infection or pathologic fracture. From our review, from 2009 to 2013, we identified 33 femoral nonunion cases, 21(15 males, six females) of which were addressed with double locking plate fixation. The lateral plate is the main plate which is long and more locking screws (about 6–8 locking screws, double cortex fixation), and the medial plate is assisted plate which is short and less locking screws (4–6 locking screws, single cortex fixation). We advocate use bone autogenous bone grafting. It not only can provide the biomechanical connection in the defect part but also can improve and reconstruct the blood circulation. We also use 360° completely surrounding fracture site autogenous bone grafting. The autogenous bone graft was obtained from anterior iliac crest. We do not use BMP or PRP. The mean age was 46.9 years (range 25–81). All of these cases initially presented as closed fractures, without neurovascular compromise. According to the OTA/AO classification, there were five 32-A, nine 32-B, and seven 32-C cases [33]. Initial treatments varied and included intramedullary nailing, single lateral plate fixation, and external fixation (due to physiologic instability). We classified 14 of the nonunion cases as atrophic nonunions. Patient demographics are listed in Table 2.
The defects often were found in 32-B- or 32-C-type fracture which was in the medial side of the diaphysis fracture. There are five bone defects in our cases. The average of the biggest defect length was 3.7 mm (range 2.1–6.5 mm) in the vertical plane which were measured by CT scan. Two of the defects were by bone resorption, and three cases were community fracture segment which cannot be fixed.
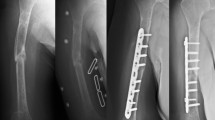
For the nonunions treated with double locking plate fixation, we used the lateral approach, and the construct consisted of a long locking plate laterally and a shorter plate anteromedially. The lateral plate was a large fragment, 4.5 mm plate, while the medial plate was a small fragment, 3.5 mm plate. All the plates were supplied by Synthes. Fixation was achieved using biologically preserving techniques (Fig. 1). We standardized our fixation construct so that all lateral plates had, along each fragment, at least six cortices of support, and all medial plates had at least four cortices of support.
After a period of non-weight-bearing for approximately 4 weeks, patients were advanced from partial to full weight-bearing over the next 1–2 months. Patients were followed serially in clinic at the 2 weeks, 4 weeks, and monthly until we noted fracture union by AP, later view and CT scan. We evaluated the mean time to fracture union, the rates of complications (defined as failure of construct, infection, and other surgical complications), and SF-36 scores [34].
Results
After employing our protocol, all the cases achieved union. We have the union rate 100 % in total 33 cases, no matter hypertrophic or atrophic nonunion. The average union time was 5.3 months (range, 4–7). The mean follow-up duration time was 24.8 months (6–60). No infections were noted postoperatively. Additionally, we did not encounter patients with recalcitrant pain, hardware failure, or construct failure. No other complications were noted in our series. No implant-related complications (screw loosening or breakage) or loss of correction was observed. Average scores noted on the physical function and bodily pain components of the SF-36 were 96 (range, 90–99) and 94.2 (range, 92–99), respectively. Average scores of the SF-36 are listed in Table 3.
Discussion
Femur shaft nonunion is common and frequently result from poor operative techniques and infection [35, 36]. The key factors leading to effective treatment for delayed unions and nonunion are solid fixation, fracture compression and good bone contact in simple fracture patterns, and osteogenic potential [9, 37–39]. Although multiple techniques exist to address nonunions, nail or plate fixation has always been controversies [8, 9, 11, 12, 14, 18–27]. Reamed exchange nail fixation has the unstable union rate (range 53–96 %). In our experience, plate or nail has their own advantages and limitations. We should consider the previous fixation and whether it is still working. If the previous fixation is nail, and it is still working, we can provide an additional plate to enhance the stability and bone graft. If the nail has been swinging in medullary canal or breakage or causing deformity, we should remove it, ream and exchange the bigger nail, or use plate. The nail has several advantages such as minimally invasive, simple procedure, and shorter operation time. Unfortunately, nail can only provide relative stability and non-anatomic reduction, especially for 32-B- or 32-C-type fractures with bone defect or fragment displacement that will increase the nonunion rate [36]. Plate fixation with bone grafting has been shown to produce excellent results, while allowing for adequate anatomic reduction with minimization of fracture gap. However, some nonunions cannot be addressed with conventional treatment techniques. In particular, OTA/AO 32-B/32-B or 32-C/32-C fractures that result in nonunions are difficult to treat due to lack of medial side support (comminution or bone defect). It is these nonunions, in particular, that we feel our double locking plate construct serves as a reasonable alternative.
Double-plate fixation has more stable union rate and above 90 %. We think that the absolute stability offered by double plate is more important for union. Because of the potential for enhanced biomechanical support, locking technology may offer advantages. In certain unstable fracture patterns (OTA/AO 32-B and 32-C) which lack medial support, locking plate constructs provide a distinct advantage over nonlocking constructs. While plates placed laterally help to counteract the tensile forces laterally (as the plate acts as a “tension band”), this construct is compromised when there is lack of cortical support medially. Anatomic reduction and more stable fixation will be achieved with lateral locking plate fixation. The short plate in the medial side can help about the reduction in the medial fragment and strength the ability of anti-rotation stability of the fracture. With a lateral locking plate serving as the primary source of construct strength, the shorter medial plate helps to support any gaps and distribution the stress medially that could fatigue the lateral construct. In such instances (where there is circumferential or atypical bone loss), double plating is advantageous which can have absolute stability, providing axial and torsional protection (Fig. 2).
A diagram shows the effect of the axial load with a single or double locking plate in the presence of a medial cortical defect (AO 32-B/32-C-type fracture). a Femoral shaft fracture in the presence of a medial cortical defect (AO 32-B/32-C: type fracture). b Femoral shaft fracture with lateral locking plate. c Biomechanical forces, as indicated by the red arrow (tensile stress and compression stress). Stress concentration indicated by the black circle. The fracture is unstable and can result in fixation failure and nonunion. d Femoral shaft fracture addressed with double locking plate. e Double locking plate allows for sound biomechanical stress transmission. The fracture is stable, and union is readily achieved with autogenous cancellous bone graft (color figure online)
The results showed 100 % union rate which is higher than nail exchange (53–96 %) and same as Parker’s (100 %) and Martinez’s (100 %) study and higher than Murray’s (94.1 %). Despite some of the patients undergoing several surgeries before our revision we still have 100 % union rate that proves the effectiveness of double locking plate. We have the longest 60-month follow-up, and the SF-36 scores showed that the patients got an improved functional status and were satisfied with therapeutic effect. We have the highest score in physical function which means that the patient could recover from disease and get back to life. The average score is about 92 that can prove this technique can meet the patients’ needs and have a satisfactory outcome. The average union time was 5.3 months (range, 4–7), shorter than 7.2 months plate augmentation [8] longer than the exchange nail 29.75 weeks [19].
The choice of bone grafting application is also an important consideration (i.e., onlay, dual onlay, cancellous inserts) [40–42]. In this study, we used 360° completely surrounding fracture site autogenous bone grafting, as its consistency allows us to manipulate it into the fracture site effectively. This can supply sufficient bone matrix, marrow cells, and relative cytokines to promote osteoblast proliferation (Fig. 3).
We considered that this technique can be well applied to femur nonunion, especially nonunion with medial defect or comminuted fragments. The contraindication of this technique we consider is bad soft tissue, infection, massive bone defect (more than 5 cm). The advantages include absolute stability for biomechanics and better blood supply and condition for osteoanagenesis and early functional exercise. The disadvantages are that there may be stress force shelter reaction in fixed bone segment. It needs more time to get the entire bone remodeling (Fig. 4).
There are some limitations to this study. It is a retrospective descriptive study, and with this, the ability to fully evaluate all forms and causes of nonunions are limited. Furthermore, locking implants are costly, and one can argue that nonlocking plates can work sufficiently in double-plate orientation. However, we felt that the use of locking plates is warranted, especially in nonunions with a significant fracture gap, as they are more resistant to deformation and failure. This may permit the patient to ambulate sooner, which can provide much needed stimulation for bone growth and proliferation.
Because of the low complication rates and the high union rates, we feel that dual locking plating with autogenous bone graft is a successful another technique for treating femoral shaft nonunions (particularly in those with significant bone gaps). The stability of our fixation construct can allow the patient to proceed with ambulation and functional activities sooner with good results.
References
Babhulkar S, Pande K, Babhulkas S (2005) Nonunion of the diaphysis of long bones. Clin Orthop Relat Res 431:50
Mast JW, Teitge RA, Gowda M (1990) Preoperative planning for the treatment of nonunions and the correction of malunions of the long bones. Orthop Clin North Am 21:693
Ebraheim NA, Martin A, Sochacki KR, Liu J (2013) Nonunion of distal femoral fractures: a systematic review. Orthop Surg 5(1):46–50
Patel VR, Menon DK, Pool RD, Simonis RB (2000) Nonunion of the humerus after failure of surgical treatment: management using the Ilizarov circular fixator. J Bone Joint Surg Br 82:977–983
Dujardyn J, Lammens J (2007) Treatment of delayed union or non-union of the tibial shaft with partial fibulectomy and an Ilizarov frame. Acta Orthop Belg 73(5):630–634
Webb LX, Winquist RA, Hansen ST (1986) Intramedullary nailing and reaming for delayed union or non-union of the femoral shaft: a report of 105 consecutive cases. Clin Orthop 212:133–141
Banaszkiewicz PA, Sabboubeh A, McLeod I, Maffulli N (2003) Femoral exchange nailing for aseptic non-union: not the end to all problems. Injury 34(5):349–356
Choi YS, Kim KS (2005) Plate augmentation leaving the nail in situ and bone grafting for non-union of femoral shaft fractures. Int Orthop 29(5):287–290
Finkemeier CG, Chapman MW (2002) Treatment of femoral diaphyseal nonunions. Clin Orthop Relat Res 398:223–234
Wu CC, Chen WJ (2002) Exchange nailing for aseptic nonunion of the femoral shaft. Int Orthop 26(2):80–84
Bellabarba C, Ricci WM, Bolhofner BR (2001) Results of indirect reduction and plating of femoral shaft nonunions after intramedullary nailing. J Orthop Trauma 15(4):254–263
Hak DJ, Lee SS, Goulet JA (2000) Success of exchange reamed intramedullary nailing for femoral shaft nonunion or delayed union. J Orthop Trauma 14(3):178–182
Ueng SW, Chao EK, Lee SS, Shih CH (1997) Augmentative plate fixation for the management of femoral nonunion after intramedullary nailing. J Trauma 43(4):640–644
Weresh MJ, Hakanson R, Stover MD, Sims SH, Kellam JF, Bosse MJ (2000) Failure of exchange reamed intramedullary nails for ununited femoral shaft fractures. J Orthop Trauma 14(5):335–338
Wu CC, Chen WJ (1997) Treatment of femoral shaft aseptic nonunions: comparison between closed and open bone-grafting techniques. J Trauma 43(1):112–116
Hailer YD, Hoffmann R (2006) Management of a nonunion of the distal femur in osteoporotic bone with the internal fixation system LISS (less invasive stabilization system). Arch Orthop Trauma Surg 126(5):350–353
Bungaro P, Pascarella R, Colozza A, Zinghi GF (1999) Rigid fixation with plate and bone graft in failures of intramedullary osteosynthesis for the treatment of diaphyseal nonunion of the femur. Chir Organi Mov 84(3):263–267
Webb LX, Winquist RA, Hansen ST (1986) Intramedullary nailing and reaming for delayed union or nonunion of the femoral shaft: a report of 105 consecutive cases. Clin Orthop Relat Res 212:133–141
Furlong AJ, Giannoudis PV, DeBoer P, Matthews SJ, MacDonald DA, Smith RM (1999) Exchange nailing for femoral shaft aseptic non-union. Injury 30(4):245–249
Yu CW, Wu CC, Chen WJ (2002) Aseptic nonunion of a femoral shaft treated using exchange nailing. Chang Gung Med J 25(9):591–598
Birjandinejad A, Ebrahimzadeh MH, Ahmadzadeh-Chabock H (2009) Augmentation plate fixation for the treatment of femoral and tibial nonunion after intramedullary nailing. Orthopedics 32(6):409
Shroeder JE, Mosheiff R, Khoury A, Liebergall M, Weil YA (2009) The outcome of closed, intramedullary exchange nailing with reamed insertion in the treatment of femoral shaft nonunions. J Orthop Trauma 23(9):653–657
Naeem-ur-Razaq M, Qasim M, Sultan S (2010) Exchange nailing for non-union of femoral shaft fractures. J Ayub Med Coll Abbottabad 22(3):106–109
Lin CJ, Chiang CC, Wu PK, Chen CF, Huang CK, Su AW, Chen WM, Liu CL, Chen TH (2012) Effectiveness of plate augmentation for femoral shaft nonunion after nailing. J Chin Med Assoc 75(8):396–401
Wang FD, Gao YZ, Yuan W, Du JQ, Wei XC (2014) Augmentative locking compression plate (LCP) combined with bone graft for the treatment of aseptic femoral shaft nonunion after intramedullary nailing. Zhongguo Gu Shang 27(10):815–818
Maimaitiyiming A, Amat A, Rehei A, Tusongjiang M, Li C (2015) Treatment of the femoral shaft nonunion with double plate fixation and bone grafting: a case series of 14 patients. Injury 46(6):1102–1107
Chiang JC, Johnson JE, Tarkin IS, Siska PA, Farrell DJ, Mormino MA (2016) Plate augmentation for femoral nonunion: more than just a salvage tool? Arch Orthop Trauma Surg 136(2):149–156
Murray WR, Lucas DB, Inman VT (1964) Treatment of non-union of fractures of the long bones by the two-plate method. J Bone Joint Surg Am 46:1027–1048
Parker B (1974) Two-plate fixation in the treatment of the tibial shaft fracture and non-union. Injury 5(4):291–297
Martinez AA, Cuenca J, Herrera A (2009) Two-plate fixation for humeral shaft non-unions. J Orthop Surg (Hong Kong) 17(2):135–138
Haverstock BD, Mandracchia VJ (1998) Cigarette smoking and bone healing: implications in foot and ankle surgery. J Foot Ankle Surg 37:69–74
Taylor JC (1992) Delayed union and nonunion of fractures. In: Crenshaw AH (ed) Campbell’s operative orthopaedics, 8th edn. St. Louis, Mosby, pp 1287–1345
Marsh JL, Slongo TF, Agel J et al (2007) Fracture and dislocation classification compendium-2007: orthopaedic trauma association classification, database and outcomes committee. J Orthop Trauma 21(Suppl 10):1–133
Keller SD, Bayliss MS, Ware JE Jr, Hsu MA, Damiano AM, Goss TF (1997) Comparison of responses to SF-36 health survey questions with one-week and four-week recall periods. Health Serv Res 32:367–384
Esterhai JL Jr, Brighton CT, Heppenstall RB, Alavi A, Mandell GA (1984) Technetium and gallium scintigraphic evaluation of patients with long bone fracture nonunion. Orthop Clin North Am 15:125
Lin SJ, Chen CL, Peng KT, Hsu WH (2014) Effect of fragmentary displacement and morphology in the treatment of comminuted femoral shaft fractures with an intramedullary nail. Injury 45(4):752–756
Boyd HB, Lipinski SW, Wiley JH (1961) Observations on nonunion of the shafts of the long bones, with a statistical analysis of 842 patients. J Bone Joint Surg 43:159–168
Crowley DJ, Kanakaris NK, Giannoudis PV (2007) Femoral diaphyseal aseptic non-unions: is there an ideal method of treatment? Injury 385:555–563
Court-Brown CM, Keating JF, Christie J, McQueen MM (1995) Exchange intramedullary nailing: its use in aseptic tibial non-union. J Bone Joint Surg Br 77B:407–411
Campbell WC (1939) The autogenous bone graft. J Bone Joint Surg 21:694
Johnson EE, Urist MR (2000) Human bone morphogenetic protein allografting for reconstruction of femoral nonunion. Clin Orthop Relat Res 371:61
Bucholz RW, Carlton A, Holmes R (1989) Interporous hydroxyapatite as a bone graft substitute in tibial plateau fractures. Clin Orthop Relat Res 240:53
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Ye Peng and Xinran Ji have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Peng, Y., Ji, X., Zhang, L. et al. Double locking plate fixation for femoral shaft nonunion. Eur J Orthop Surg Traumatol 26, 501–507 (2016). https://doi.org/10.1007/s00590-016-1765-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-016-1765-z