Abstract
Background
The aim of this retrospective review was to determine the incidence and severity of heterotrophic ossification (HO) following acute revision total hip arthroplasty (THA), and whether this represents a significant risk factor for HO that should be treated prophylactically.
Materials and methods
A total of seven patients (three men and four women) with a mean age of 55 years (39–70 years) who underwent a reoperation of their THA for any reason that required a hip arthrotomy within 3 weeks of their primary or revision THA were included, with a mean follow-up of 8.8 years (2–12 years). All patients were evaluated radiographically for any evidence of HO and clinically using the Harris Hip Score.
Results
All seven hips (100 %) developed HO, with 71 % being severe (Brooker III and IV HO). One hip (14 %) developed Brooker IV HO, four hips (57 %) developed Brooker III HO, and two hips (29 %) developed Brooker II HO. The patient’s range of motion varied, but was very limited in three patients. Three patients (42.8 %) were not satisfied with their surgery; one patient had Brooker IV HO, and two patients had Brooker III HO.
Conclusion
Acute reoperation after primary or revision THA is a significant risk factor for the development of extensive HO, which requires prophylactic treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Heterotopic ossification (HO) is a well-recognized complication following total hip arthroplasty (THA). The incidence of HO has been reported as low as 1–2 % in the general population, and up to 90 % in patients with multiple risk factors [1–7]. Although the majority of cases are clinically insignificant and asymptomatic, severe HO can significantly compromise the patient’s outcome following an otherwise successful THA. The formation of extensive HO can cause severe postoperative hip pain, significantly restrict hip motion and can cause impingement that results in instability [8, 9].
Radiotherapy and non-steroidal anti-inflammatories have been shown to be effective prophylactic measures to minimize the likelihood of ectopic bone formation, as well as increase the likelihood that any bone that does form, remains mild enough to not be of clinical concern following THA [10–15]. The prevention of postoperative HO can best be accomplished by the preoperative identification and subsequent treatment of those patients who are at high risk of its development. Known risk factors include a history of HO in either hip, ankylosing spondylitis, diffuse idiopathic skeletal hyperostosis, hypertrophic arthrosis, male gender, advanced age and ipsilateral acute displaced acetabular fracture [1, 7, 16–23]. Revision THA is not recognized as a risk factor per se, unless there is a history of HO in either hip [5, 7, 17, 24–27].
Due to population aging, the rate of revision THA surgery is on the rise with aseptic loosening being the most common cause [28]. On the other hand, acute reoperation after primary or revision THA is very uncommon and is usually related to technical errors, dislocation, periprosthetic fracture or infection. However, we have noted that early revision THA is frequently complicated by severe HO. The aim of this study was to determine the incidence and severity of HO following acute revision THA and determine whether this represents a significant risk factor for HO.
Materials and methods
Using prospectively collected data from our computerized database, we reviewed 963 consecutive primary THAs and 190 consecutive revision THAs performed by a single surgeon (MT) from August 1991 to August 2012. We identified all patients who underwent a reoperation of their hip arthroplasty for any reason that required a hip arthrotomy within 3 weeks of their primary or revision THA. None of the patients undergoing an acute revision surgery had any prophylactic treatment for HO, and all patients had at least a 2-year follow-up. Institutional review board approval for the study was obtained.
Seven patients (seven hips) were found to meet the inclusion criteria (Table 1). There were four women and three men, with an average age of 55 years (range 39–70 years). The average patient height was 1.68 m (range 1.58–1.8 m), and the average weight was 70 kg (range 50–95 kg). The right hip was involved in three patients and the left in four patients. The demographics of the patients undergoing an early revision are listed in Table 1. The initial surgery was a primary cementless THA in five cases and a revision THA in two cases (Table 1). The primary THA was done for osteoarthritis in three cases and avascular necrosis in two cases. A S-ROM femoral component (DePuy, Warsaw, IN) was used in two hips, a Versys Fiber Metal Taper stem (Zimmer, Warsaw, IN) was used in one hip, a Multilock femoral stem (Zimmer, Warsaw, IN) was used in one hip, and a Trilock stem (DePuy, Warsaw, IN) was used in one hip. The acetabular component was a Pinnacle cup (DePuy, Warsaw, IN) in three hips, and a Trilogy cup (Zimmer, Warsaw, IN) in two hips. Both revision arthroplasties were cementless revisions done for aseptic loosening of a cemented THA. In both cases, a Trilogy cup with screws (Zimmer, Warsaw, IN) was used. A S-ROM femoral component (DePuy, Warsaw, IN) was used in one case, and a Solution femoral stem (DePuy, Warsaw, IN) was used in the other case. Both index revision surgeries required bone grafting of the acetabulum and femur using morcellized, non-structural allograft bone. A posterolateral approach to the hip was used in all cases for the initial surgery and for the acute reoperation. The abductors were not released or partially detached in any of the primary cases. An extended trochanteric osteotomy was required in both index revision cases, but only one hip required a repeat trochanteric osteotomy for the acute reoperation.
All patients were prospectively evaluated clinically and radiographically preoperatively and postoperatively at 6 weeks, 3, 12 months, 2 years and every 1–2 years thereafter. Established preoperative risk factors for HO were specifically assessed for each patient, including clinical and/or radiographic evidence of HO in either hip, ankylosing spondylitis, diffuse idiopathic skeletal hyperostosis, hypertrophic arthritis or an acute acetabular fracture. All hips were evaluated radiographically with an anteroposterior (AP) pelvis, AP hip, and true and frog-leg lateral radiographs. Preoperatively, the radiographs were assessed in order to identify any risk factors for HO. Final radiographs were assessed for HO and, if present, quantified using the Brooker classification [29, 30]. Brooker Grade 0 indicated no ossification; Grade I indicated islands of bone within the soft tissues; Grade II indicated bone spurs arising from the pelvis or proximal end of femur, leaving at least 1 cm between opposing bone surfaces; Grade III indicated bone spurs arising from the pelvis or proximal end of femur, reducing the space between opposing bone surfaces to less than 1 cm; and Grade IV indicated apparent ankylosis of the hip. Clinical outcomes, including range of motion were evaluated using the Harris Hip Score (HHS) [4].
Results
Of the five hips (five patients) identified that required an acute reoperation after the primary THA, the reason for reoperation was recurrent anterior hip dislocation in three patients, postoperative subsidence of the femoral stem with fracture of the lateral femoral cortex in one patient, and incomplete seating of the acetabular component secondary to an interposed fractured osteophyte in one patient (Table 2). Two of the three hips that underwent acute reoperation for recurrent instability had revision of the modular S-ROM stem with retention of the modular sleeve in order to decrease the femoral anteversion and increase the offset. The third hip required revision of the acetabulum, with a Trilogy cup implanted in less anteversion. The hip with incomplete seating of the acetabular cup required revision of the acetabulum with a Trilogy cup, after removal of the interposed fractured osteophyte. The femoral component that subsided was revised to an S-ROM stem with a bulk strut allograft to cover the lateral cortical defect. Of the two patients who underwent a revision THA as their initial surgery, one patient required reoperation for recurrent anterior dislocation, and one had a fracture of the medial wall of the acetabulum with migration of the cup. The hip that dislocated had a revision arthrotomy and partial excision of the ischium to correct the impingement that was occurring and causing anterior levering of the hip. The hip with the medial wall fracture was revised to a Burch-Schneider cage (Zimmer, Warsaw, IN) with a cemented acetabular cup used with morcellized bone allograft to the anterior and medial walls of the acetabulum. The average time from the index THA and the acute reoperation was 10 days (range 1–19 days) (Table 2).
Only one out of these seven patients (14 %) had a predisposing risk factor for postoperative HO. This patient developed Brooker II HO following a primary THA on the contralateral side. After his acute reoperation, he developed Brooker III heterotopic ossification. The remaining six patients had no risk factors for developing postoperative HO after their hip arthroplasty.
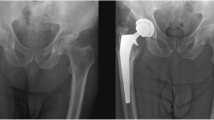
All seven hips (100 %) that underwent reoperation within 3 weeks of the initial hip arthroplasty developed HO (Table 2). The severity of HO varied, but the majority of the hips (71 %) developed severe HO (Brooker III and IV) (Table 3). One of the seven hips (14 %) developed Brooker IV HO, four hips (57 %) developed Brooker III HO (Fig. 1), and two hips (29 %) developed Brooker II HO. One patient with Brooker II and another patient with Brooker III HO received late irradiation (7 gray) at 6 and 12 weeks, respectively [31].
a Preoperative anteroposterior (AP) radiograph of the pelvis, showing degenerative changes of the right hip in a 44-year-old male (patient 3, Table 2) with no evidence of known risk factors for heterotrophic ossification (HO). b An AP radiograph of the hip 2 days post-primary total hip arthroplasty (THA), demonstrating femoral stem subsidence and fracture of the lateral femoral cortex. This required revision surgery 16 days following the primary THA. c An AP radiograph of the hip taken 2 days post-revision THA, showing a modular femoral stem with a strut allograft fixed with cables. d Seven years post-revision surgery; an AP radiograph of the hip demonstrates Grade III HO
The average clinical follow-up was 8.8 years (range 2–12 years). The final HHS was excellent (>89) in five patients (71 %), fair (70–79) in 1 patient (14 %) and poor (<70) in one patient (14 %) (Table 3). The patients with the fair and poor HHS had Grade IV and Grade II HO, respectively. The patient’s range of motion varied, but was very limited in three patients (Table 3). Three patients (42.8 %) were not satisfied with their surgery; one patient had Grade IV HO, and two patients had Grade III HO. The remaining four patients (57.2 %) were satisfied with their surgery (Table 3).
Discussion
The identification of risk factors in patients undergoing primary or revision THA is the mainstay in preventing the formation of postoperative heterotopic ossification. Once identified, patients at risk of HO can be effectively treated perioperatively. This study identifies an acute reoperation, following primary or revision THA, as a previously unrecognized risk factor for HO. In all our cases, revision hip arthroplasty done within 3 weeks of the initial hip arthroplasty resulted in the formation of HO.
Not only did all the patients in this study develop HO after their acute reoperation, in 71 % of the cases the patients formed significant HO, being Brooker Grade III or IV. Although one could postulate that the HO may have formed in these patients even in the absence of an acute reoperation, this is unlikely since the incidence of HO was 100 % in this series, with only one patient having a well-documented risk factor for HO. This patient developed Brooker II HO after a contralateral primary THA and developed Brooker III HO after his acute reoperation. Previously, Ritter and Vaughan reported that the quantity of HO developed in a cohort of 23 patients with a history of HO was similar to that developed after their original arthroplasty [17]. Although the patient in this study has a confounding risk factor, the increased severity of HO formed after the acute revision surgery indicates that an acute reoperation adds to the risk of developing HO.
Although HO following hip arthroplasty may at times be no more than a benign radiographic appearance, in some cases, there can be significant clinical compromise in long-term function. The grading of HO with the Brooker classification has been shown to correlate with hip range of motion, but not with the HHS [32]. Our results showed a similar correlation. Five of the six patients who did not develop ankylosis from their HO had an excellent HHS, while three of the five patients who developed Brooker III or IV HO had a limited range of motion.
In this study, two hips were treated with late irradiation, at 6 and 12 weeks postoperatively, in an attempt to prevent progression of the HO that had already developed. This technique has previously been shown to be effective by Kantor et al. [31]. Using a standard dose of 7 gray, eight patients who underwent a cementless THA were irradiated after their 6-week postoperative follow-up visit and none of the hips went on to progress from clinically insignificant grades of HO (Brooker I, II) to more advanced grades (Brooker III, IV). When compared to the untreated control group of nine patients, over the 2-year study period, the treated group had only a 32 % progression in the quantity of bone formed compared with 86 % in the control group. On the contrary, other authors reported a higher rate of heterotopic ossification if radiotherapy was given after the 4th postoperative day [33, 34]. Therefore, although it is possible that if the two patients in our study did not have late irradiation treatment they may have developed a higher grade of HO with clinical symptoms, but this remains unclear.
One can only speculate on why an acute reoperation following hip arthroplasty results in such a significant risk of developing HO. The cause may be similar to HO forming following blast injuries or burns. Although the molecular mechanisms of HO have not been fully elucidated in experimental models [35], inflammatory signaling pathways are speculated to play critical roles in HO formation. Forsberg et al. [36] have found an association between a patient’s systemic and local inflammatory responses and HO. It is conceivable that reoperating on a patient so soon after their initial surgery results in significant trauma to tissues already going through the inflammatory phase of wound healing. This may result in a significant increase in the local inflammatory response, which then predisposes to developing HO.
It is not clear from this small series whether the timing of the reoperation is correlated with the degree of HO that forms. However, the only Brooker Grade IV HO case occurred when the patient underwent a revision surgery within 24 h of her index procedure. The longest duration between the index surgery and the acute reoperation in this series was 19 days, and in this case, the patient only developed a small amount of HO (Brooker II). A larger number of patients are necessary to definitively correlate the severity of the HO that occurs after an acute reoperation and the time between surgeries.
There are some limitations to this study, none of which significantly affect the findings. Although the study is retrospective, the clinical data were collected prospectively and reviewed with the radiographs retrospectively. One might consider that the small number of patients in this study may not reflect a larger cohort of patients. However, the incidence of significant HO in patients without risk factors is low. In this study, 100 % of the patients developed HO and the majority of the hips developed severe Brooker Grade III or IV HO. Given that acute reoperation after primary or revision THA is very uncommon, recruiting a large number of patients in such a study would require a multicenter collaboration.
This study clearly identifies acute reoperation after primary or revision THA as a significant risk for the development of HO. Furthermore, the HO that develops is usually more extensive and can adversely affect the outcome of the surgery. As a result, we strongly recommend prophylactically treating all patients undergoing a revision surgery within 3 weeks of the index arthroplasty with any of the effective methods described in the literature to prevent the formation of HO.
References
Rosendahl S, Christoffersen JK, Norgaard M (1977) Para-articular ossification following hip replacement: 70 arthroplasties ad modum Moore using McFarland’s approach. Acta Orthop Scand 48(4):400
Evarts CM, Ayers DC, Puzas JE (1987) Prevention of heterotopic bone formation in high risk patients by postoperative irradiation. In: Hip: proceedings of the hip society. J.B. Lippincott, Philadelphia, pp 70–83
Neal B, Gray H, MacMahon S, Dunn L (2002) Incidence of heterotopic bone formation after major hip surgery. ANZ J Surg 72(11):808
Soballe K, Christensen F, Kristensen SS (1988) Ectopic bone formation after total hip arthroplasty. Clin Orthop Relat Res 228:57
Sodemann B, Persson PE, Nilsson O (1988) Etiology and treatment of periarticular heterotopic ossification after total hip replacement. Rev Chir Orthop Reparatrice Appar Mot 74(Suppl 2):329
Ahrengart L (1991) Periarticular heterotopic ossification after total hip arthroplasty. Risk factors and consequences. Clin Orthop Relat Res 263:49
DeLee J, Ferrari A, Charnley J (1976) Ectopic bone formation following low friction arthroplasty of the hip. Clin Orthop Relat Res 121:53
Fransen M, Neal B (2004) Non-steroidal anti-inflammatory drugs for preventing heterotopic bone formation after hip arthroplasty. Cochrane Database Syst Rev 3:CD001160
Neal B (2003) Effects of heterotopic bone formation on outcome after hip arthroplasty. ANZ J Surg 73(6):422
Vavken P, Castellani L, Sculco TP (2009) Prophylaxis of heterotopic ossification of the hip: systematic review and meta-analysis. Clin Orthop Relat Res 467(12):3283
Birrell F, Lohmander S (2006) Non-steroidal anti-inflammatory drugs after hip replacement. BMJ 333(7567):507
Burd TA, Lowry KJ, Anglen JO (2001) Indomethacin compared with localized irradiation for the prevention of heterotopic ossification following surgical treatment of acetabular fractures. J Bone Joint Surg Am 83(12):1783
Knelles D, Barthel T, Karrer A, Kraus U, Eulert J, Kolbl O (1997) Prevention of heterotopic ossification after total hip replacement. A prospective, randomised study using acetylsalicylic acid, indomethacin and fractional or single-dose irradiation. J Bone Joint Surg Br 79(4):596
Pakos EE, Ioannidis JP (2004) Radiotherapy vs. nonsteroidal anti-inflammatory drugs for the prevention of heterotopic ossification after major hip procedures: a meta-analysis of randomized trials. Int J Radiat Oncol Biol Phys 60(3):888
Sell S, Willms R, Jany R, Esenwein S, Gaissmaier C, Martini F, Bruhn G, Burkhardsmaier F, Bamberg M, Kusswetter W (1998) The suppression of heterotopic ossifications: radiation versus NSAID therapy: a prospective study. J Arthroplasty 13(8):854
Chemaly O, Hebert-Davies J, Rouleau DM, Benoit B, Laflamme GY (2013) Heterotopic ossification following total hip replacement for acetabular fractures. Bone Joint J 95(1):95
Ritter MA, Vaughan RB (1977) Ectopic ossification after total hip arthroplasty. Predisposing factors, frequency, and effect on results. J Bone Joint Surg Am 59(3):345
Kjaersgaard-Andersen P, Sletgard J, Gjerloff C, Lund F (1990) Heterotopic bone formation after noncemented total hip arthroplasty. Location of ectopic bone and the influence of postoperative antiinflammatory treatment. Clin Orthop Relat Res 252:156
Ahrengart L, Lindgren U (1993) Heterotopic bone after hip arthroplasty. Defining the patient at risk. Clin Orthop Relat Res 293:153
Lazansky MG (1973) Complications revisited. The debit side of total hip replacement. Clin Orthop Relat Res 95:96
Hierton C, Blomgren G, Lindgren U (1983) Factors associated with heterotopic bone formation in cemented total hip prostheses. Acta Orthop Scand 54(5):698
Walker LG, Sledge CB (1991) Total hip arthroplasty in ankylosing spondylitis. Clin Orthop Relat Res 262:198
Blasingame JP, Resnick D, Coutts RD, Danzig LA (1981) Extensive spinal osteophytosis as a risk factor for heterotopic bone formation after total hip arthroplasty. Clin Orthop Relat Res 161:191
Nollen JG, van Douveren FQ (1993) Ectopic ossification in hip arthroplasty. A retrospective study of predisposing factors in 637 cases. Acta Orthop Scand 64(2):185
Nollen AJ, Slooff TJ (1973) Para-articular ossifications after total hip replacement. Acta Orthop Scand 44(2):230
Kjaersgaard-Andersen P, Schmidt SA (1991) Total hip arthroplasty. The role of antiinflammatory medications in the prevention of heterotopic ossification. Clin Orthop Relat Res 263:78
Sodemann B, Persson PE, Nilsson OS (1988) Periarticular heterotopic ossification after total hip arthroplasty for primary coxarthrosis. Clin Orthop Relat Res 237:150
Lui DF, Bandorf N, Riordan P, Jaweesh O, Duru B, Bennett D (2013) Preoperative comorbidity and modes of failure in revision hip arthroplasty: a single-surgeon series in a tertiary referral centre. Eur J Orthop Surg Traumatol 23(3):329–333
Kjaersgaard-Andersen P, Ritter MA (1991) Prevention of formation of heterotopic bone after total hip arthroplasty. J Bone Joint Surg Am 73(6):942
Brooker AF, Bowerman JW, Robinson RA, Riley LH Jr (1973) Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg Am 55(8):1629
Kantor SR, Cummins J, Tanzer M (2005) Complications after Total Hip Arthroplasty: Heterotopic Ossification. Semin Arthroplasty 16(2):105
Wright JG, Moran E, Bogoch E (1994) Reliability and validity of the grading of heterotopic ossification. J Arthroplasty 9(5):549
Sylvester JE, Blount LH, Selch MT (1992) Technical considerations in the use of prophylactic radiation therapy to prevent heterotopic bone formation. Semin Arthroplasty 3:167–171
Coventry MB, Scanlon PW (1981) The use of radiation to discourage ectopic bone. A nine-year study in surgery about the hip. J Bone Joint Surg Am 63(2):201–208
Zhang K, Wang L, Zhang S, Yu B, Liu F, Cui Z, Jin D, Bai X (2013) Celecoxib inhibits the heterotopic ossification in the rat model with Achilles tenotomy. Eur J Orthop Surg Traumatol 23(2):145–148
Forsberg JA, Potter BK, Polfer EM, Safford SD, Elster EE (2014) Do inflammatory markers portend heterotopic ossification and wound failure in combat wounds? Clin Orthop Relat Res 472:2845–2854
Acknowledgments
The authors would like to thank Karen Smith for her contribution in collecting the data.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Aljurayyan has nothing to disclose. D. Tanzer has nothing to disclose. Dr. M.Tanzer reports grants and personal fees from Zimmer, and grants from DePuy, outside the submitted work.
Ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Aljurayyan, A., Tanzer, D. & Tanzer, M. Acute revision hip arthroplasty: a previously unrecognized risk factor for heterotopic ossification. Eur J Orthop Surg Traumatol 26, 183–188 (2016). https://doi.org/10.1007/s00590-015-1733-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-015-1733-z