Abstract
Objective
Whether external or plating fixation is more appropriate for high-energy tibial plateau fractures is still being disputed, our aim was to test the hypothesis whether external fixation can provide a fair outcome with fewer complications, when compared to the results with previously reported data of plating fixation for high-energy tibial plateau fractures.
Methods
An Ovid of Medline, Embase, and Cochrane Library search was conducted for the relevant English orthopedic journals, and eligible studies, including twenty-four case series and one comparative study containing 885 patients associated with 892 fractures, were enrolled.
Results
The results showed there were a higher proportion of men, open fractures, malunion, knee instability, and posttraumatic arthritis occurred in external fixation group than those in plating group (P = 0.007, P = 0.000, P = 0.024, P = 0.006, P = 0.000, respectively), while valgus deformity happened at a significantly higher rate in plate group (P = 0.014). No significant differences were found between the two groups in terms of age, Schatzker type, follow-up, mean time to union, mean range of knee motion, and rate of reoperation. With regard to the functional and radiological outcome assessment, despite what assessment tools were used, most of these studies presented less than 90 % good/excellent results in their high-energy fracture series. Besides, there was a trend for patients in plating group to have a higher risk than those in external fixation group in terms of heterotopic ossification and local irritation (1.23 vs 0.17 %, 4 vs 1.94 %, accordingly).
Conclusions
Although lack of good quality randomized control trials, there are rather enough samples supporting the current available results. Meanwhile, future multicentered, randomized, controlled studies should be implemented to test these outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
High-energy tibial plateau fractures (types V and VI, according to the system of Schatzker [1], and types C1, C2, and C3, according to the system of the Orthopaedic Trauma Association [2]) are severe injuries frequently associated with multisystem trauma, ipsilateral skeletal trauma, and multiligamentous injuries. The results of treatment of these injuries have often been poor, with loss of motion, instability, posttraumatic osteoarthritis, wound breakdown, and infection as final outcomes [3–8]. External fixation (EF) is an established method for the treatment of certain types of high-energy tibial plateau fractures because of its ease of application and minimal surgical exposure. Conversely, there has been an increasing trend toward the use of open reduction and internal fixation (ORIF) with plates owing to the potential for direct fracture reduction and earlier postoperative mobilization. Nonetheless, recent systematic reviews of the literature have failed to provide substantial evidence supporting the use of one of the above-mentioned techniques over the other for the management of tibial plateau fractures [9]. We performed case analysis using non-randomized controlled trials that compare EF to ORIF with plating for the treatment of high-energy tibial plateau fractures. The purpose of this study was to determine whether the clinical outcomes of patients with bicondylar tibial plateau fractures treated with open reduction and plate fixation (PF) are better than those achieved with external fixation.
Materials and methods
An Ovid of Medline (1946–2013), Embase (1974–2013), and Cochrane Library search was conducted for relevant publications up to August 2013. The following phrases, respectively, acted as keywords and title through advanced search: High energy/complex/comminuted/severe/Schatzker IV/V tibial plateau fractures, and bibliographies of all retrieved studies were reviewed for relevant articles. This search strategy was performed independently by two co-authors. Inclusive and exclusive criteria are outlined in Table 1. All relevant data from papers that met the initial inclusion criteria were extracted independently by two of the authors. Then, each eligible study was independently reviewed by authors for methodological quality to decrease bias due to the variation in the quality of the published observational studies. Although there are scoring systems available for assessing the methodological quality of randomized controlled trials, we were unable to find any published methodological quality scoring systems to assess non-randomized controlled studies such as case series. Therefore, a methodological scoring system adapted from that of Detsky et al. [10] was used. The scoring system used consisted of answering to the following questions:
-
1.
Were patient characteristics adequately described including at least four details of admission provided? (e.g., age, sex, mobility, fracture type, etc.)
-
2.
Were the treatment methods adequately described?
-
3.
Were inclusion/exclusion criteria well defined?
-
4.
Were the number of patients excluded and reasons for exclusion provided?
-
5.
Were all the outcome measures adequately defined in the text with clarification of any ambiguous terms encountered?
-
6.
Was the timing of outcome measures appropriate? (A minimum of 12 months follow-up for all surviving patients available.
A clear affirmative answer scored two points, an affirmative answer with incomplete information scored one point, and no information scored zero points. The highest possible score is 12 points; studies with less than 8 points were excluded. Any disagreement in between the 2 reviewers was resolved by means of discussion to achieve consensus. We sought the following summary data from each study: (1) information on general characteristics of participants; (2) clinical and radiological outcomes assessment; (3) postoperative complications (pin-track infection, abnormal union, instability, knee stiffness, etc.); (4) the average range of motion for knee flexion; (5) mean union time; (6) rate of reoperation.
Data analysis
Statistical analysis was performed with use of the SPSS 18 software. The weighted means of continuous parameters of interest were compared across groups using a two-tailed independent sample t test, such as age, knee range of motion, etc. A chi-square test was used for categorical variables between the two groups, such as gender, fracture pattern, etc. A traditional Pearson chi-square test was used when statistical conditions were met. The Fisher exact test was used in case when one or more of the expected variables were less than five. A P value of <0.05 was considered to be significant (Tables 2, 3).
Results
The above methodology identified 263 studies of which 25 studies met the inclusion criteria. One study was a comparative study between locked plating and external fixation [6]; therefore, 16 studies were external fixations and 10 studies were plate fixations. The total number of cases in the included studies was 885 (561 external fixations and 331 plate fixations) associated with 892 tibial plateau fractures. The assessment of study quality was conducted by two authors of this review. The mean study quality score was 9.69 ± 1.04 in the study (Fig. 1).
Demographic variables
The mean age of the patients in these studies included was 42.38 ± 4.46 years (range 17–90 years). Specifically, the mean age of the patients for external fixators was 41.57 ± 4.90 years (range 17–90 years) and for plate fixators was 43.79 ± 3.10 years (range 17–88 years). There was no significant difference between the groups with regard to the ages (t = 0.065, P = 0.949, Fig. 2). These studies included, except gender was not available in two studies [11, 12], reported on 611 males and 222 females. To be specific, there were 390 males and 119 females in the external fixator group and 221 males and 103 females in the plating group; significant difference was detected between the groups with respect to gender (χ 2 = 7.165, P = 0.007, Fig. 3). In other words, there was a higher male ratio in the external fixator group than plating group.
Injury characteristics
There were 883 patients who had sustained 890 tibial plateau fractures; the other two were unclassified [13]. Twenty-two studies reported fracture pattern using Schatzker’s classification [4–8, 11–27], the other three using the AO/OTA classification [28–30]. From the studies using Schatzker’s classification, there were 641 fractures distributed as 28.39 %(182) Type V, and 71.61 %(459) Type VI. For Schatzker type, there was no significant difference between the groups (χ 2 = 1.184, P = 0.277, Fig. 4). Of the 892 tibial plateau fractures, 214 were open using Gustilo-Anderson’s classification, 171(30.15 %) fractures in the external fixator group while 43 (13.23 %) fractures in the plating group. In terms of open fractures, significant difference was demonstrated between external fixator group and plating group (χ 2 = 32.464, P = 0.000, Fig. 4).
Follow-up
Except one study [8], the follow-up was not available. The mean follow-up of the patients in these studies included was 32.52 ± 14.30 months (range 3–112 months). To be specific, the mean follow-up was 35.42 ± 15.48 months (range, 6–112 months) for the external fixation group and 27.21 ± 9.85 months (range, 3–104.2 months) for the plating group. With respect to follow-up, the difference was not as significant between the groups (t = 0.358, P = 0.724, Fig. 5).
Functional and radiological assessment
With regards to functional and radiological assessment, there existed a significant heterogeneity in intra- and inter-group.
All but four [6–8, 17] of the studies report the functional outcome following plateau reconstruction. Four studies [11, 20, 21, 27] used Rasmussen’s score [31], three of the studies [11, 20, 21] in the external fixation group and the remaining one [27] in plating group, the former reporting on 86 tibial plateau fractures and have recorded good-to-excellent results in over 87 % of their cases at over 16 months of follow-up and the latter recording on 18 tibial plateau fractures. Of the cases, 88 % have scored good-to-excellent results at over 36 months of follow-up. Eight studies [4, 12–14, 16, 18, 19, 23] were evaluated according to the Knee Society Clinical Rating System criteria [32], one study [23] in plating group reported 54 tibial plateau fractures, and the mean Knee Society Clinical Rating Score was 70.3 at over a year of follow-up. The remaining seven studies in external fixator group recorded 173 tibial plateau fractures, 80.9 % of the cases have achieved good-to-excellent results at over 6 months of follow-up. For external fixator group, one study [15] using ASAMI’s (Association for the Study and Application of the Method of Ilizarov) scoring system, 96 % of the cases have achieved good-to-excellent results at over 11 months of follow-up; three studies [5, 22, 28], using the Honkonen–Jarvinen functional criteria [33], attained good-to-excellent results in 66 % of their cases at over 24 months of follow-up. For plating group, SF-36 (Short Form-36) patient health assessments were implemented in two studies [24, 30], the mean physical component scores and mental component scores were, respectively, 40 and 52 in one study [30], and the others were 89 with regard to the mean SF-36 health assessments. Four studies [23–26] used the Hospital for Special Surgery (HSS) knee score; the mean of HSS score was 82.87 ± 6.10. Lysholm knee scores were obtained in three studies [23, 25, 30], the average value of which was 84.35 ± 5.35.
Fifteen studies [4, 6, 7, 12, 14–17, 19–21, 23–25, 27] reporting the average range of knee flexion. Therefore, the average value of knee flexion was 109.4° ± 12.6° (range, 0°–170°) in external fixation group [4, 6, 12, 14–17, 19–21] and 118.5° ± 11.2° (range, 60°–150°) in plating group [6, 7, 23–25, 27]; no significant difference was demonstrated between the groups (t = 1.453, P = 0.168, Fig. 6).
The radiological assessment of outcome was reported by twelve [4, 5, 11, 13, 16, 21–23, 26–29] of the twenty-five studies. Four studies [11, 16, 21, 27] used the Rasmussen’s score recording 106 tibial plateau fractures, to be specific, there were 88 tibial plateau fractures in the external fixation group [11, 16, 21] and 18 in plating group [27], the former have recorded good-to-excellent results in over 87 % of their cases at over 16 months of follow-up, the latter reporting good-to-excellent results in over 88 % of their cases at over 36 months of follow-up. Besides, three studies [5, 22, 28] were estimated according to Honkonen and Jarvinen radiological criteria; 69 % of the results achieved good-to-excellent results at over 2 years of follow-up. Six others [4, 13, 23, 26, 28, 29] reporting 313 fractures used the author’s own assessment tools and have recorded good-to-excellent results in over 65 % of their cases at over 3 months of follow-up.
Mean time to union
Fracture healing was recorded in 22 of the reviewed studies [4–8, 12–15, 17–28, 30] with 759 tibial plateau fractures. The average time to union in the external fixation group was 17.73 ± 4.87 weeks (range, 8.5–64.2 weeks) versus 15.64 ± 4.36 weeks (range, 6–60 weeks) with plating group. There was no difference between the groups with respect to the mean time to union (t = 1.041, P = 0.310, Fig. 7).
Complications
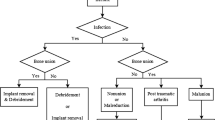
There were 567 tibial plateau fractures in external fixation group and 325 in plating group. One of the most common complications in the former was pin tract infection, eleven studies [4, 5, 11, 13–15, 17–21] reported on pin tract infection in 78 cases, the rate of pin tract infection was 13.75 %, while superficial infection in the latter was 5 (1.53 %) cases, and the other common complications are detailedly listed in Table 4. To make full use and analyze these data, knee stiffness, knee flexion <90°, flexion contracture, and extension lag were categorized into dyskinesia (Table 4). Likewise, deep wound infection, osteomyelitis, and septic arthritis were defined as deep infection. Besides, there existed rare complications in external fixator group, such as intraoperative popliteal vein injury 1 case [13] and pulmonary embolism four case [22]. When the data analysis focused on differences between the groups, it was evident that complications of malunion, knee instability, and posttraumatic arthritis occurred at a significantly higher rate in external fixator group (P = 0.024, P = 0.006, P = 0.000, respectively, Fig. 8) while valgus deformity in plating group (P = 0.014, Fig. 8). Nevertheless, with regards to heterotopic ossification and local irritation, there was a higher trend in plating group compared with external fixator group (1.23 vs 0.17 %, 4 vs 1.94 %, accordingly).
Reoperation
Procedures done secondary to the definitive intervention were considered a reoperation or a complication. 70 (12.3 %) fractures had external fixators required secondary surgeries, whereas 42 (12.9 %) fractures managed with plating fixations required additional surgeries (χ 2 = 0.063, P = 0.802, Fig. 9). Due to some information was not available, it was unclear that what complication leads to the most common secondary revisional surgery.
Discussion
High-energy tibial plateau fractures, which are notoriously difficult fractures associated with severe bone and soft tissue injury that lead to high complication rates and poor clinical outcomes [4, 13, 16, 22, 23, 26]. Different methods for treating these complex injuries have been proposed, including arthroscopic-assisted reduction with internal fixation [27], open reduction and internal fixation [7, 8, 23–26, 29, 30] and indirect reduction, and application of a hybrid [11, 14, 17, 19, 20] or a circular external fixation device [13, 15]. In the herein study, our aim was to test the hypothesis whether external fixation can provide a fair outcome with less complications, when compared to the results with previously reported data of plating fixation for types V and VI high-energy tibial plateau fractures.
In terms of demographic variables and injured features, Hall et al. [34] and Krupp et al. [6], in their compared clinical trial of high-energy tibial plateau fractures treated with internal or external fixation, reported no significant differences between external fixation and plating fixation. However, our study showed there were a higher proportion of men and open fractures in the external fixator group than those in plating group. Our findings were consistent with those of Bugler et al. [35] who found 69.1 % of open fractures occurred in males with an average age of 40.8 years and 30.9 % occurred in females with an average age of 56.0 years; it is the males who tend to sustain open fractures as a result of sport, falls from a height, road traffic accidents, and direct blows or assaults.
This paper initially planned to focus on the outcome of the clinical and radiological evaluation. However, such an analysis was not possible due to the amalgamation of the different clinical and radiological results in the papers. No matter what questionnaires were used, as far as the functional outcome be concerned, except one study [15] in the external fixation group, 96 % of the cases have achieved good-to-excellent results at over 11 months of follow-up, most of these studies presented less than 90 % good/excellent results in their type V and VI fracture series [4, 5, 11–14, 16, 18–21, 23, 25, 28, 30].
Our study was supported by the results of the previous work Hall et al. [34], who reported that the mean HSS score was 75 in the circular fixator group while 68 in the open reduction and internal fixation group 2 years after the injury. The same was to radiological outcome assessment. Besides, the mean knee flexion was 109° in the circular fixator group compared with 118° in plating group in this review, the difference was not significant, which was similar to previous reported results [6, 34].
Fracture healing, in theory, was superior in external fixation due to the principles of biological osteosynthesis and minimally invasive surgery for the treatment of comminuted tibial plateau fractures. Although Hall et al. [34] in their randomized, controlled clinical trial had reported that patients in the circular fixator group were more likely to have returned to the preinjury level of activity than those in the open reduction and internal fixation group at the 6-month evaluation, this paper demonstrated no significant difference between external fixation group and plating group (17 vs 15 weeks, respectively). What’s more, Krupp et al. [6] in their comparative study found that the average time to union was shorter in locked plating group than external fixator group (5.9 vs 7.4 months); the improved healing rate may potentially be related to the fixation characteristics of the locking plates, increased use of bone grafting, and/or a more adequate reduction.
The rate of complications, especially deep infection, is often a variable that orthopedic surgeons have cited in favor of external fixation over ORIF. The results of our study were different from this theory; the groups were not significantly different with respect to deep infection. On the contrary, there was a higher complication rate in the external fixation group, in particular, complications of malunion, posttraumatic arthritis, and knee instability as compared to plating group; these findings are supported in studies by Krupp et al. [6] and Hall et al. [34], and plates provide improved healing rates, restoration of the articular surface, a straight leg, a stable knee, and decreased complications. With regards to heterotopic ossification and local hardware irritation, there was a higher proportion in plating group. In addition, in term of reoperation, there was no difference between the groups in our study, but Hall et al. [34] recorded that there was a lower reoperation rate in the circular fixator group when compared to plating group.
Although the small population size, the lack of control groups, and the various functional assessment tools in the majority of these publications limited the strength of any recommendations that could be made regarding the optimal options of surgical method, the systematic analysis of the accumulated data contributed to increasing relatively high level of evidence.
Conclusion
Although lack of enough quality randomized control trials and there exists some bias in the study, this paper shows rather enough samples supporting the current available results, and our study could offer some useful information for orthopedists in the management of complex tibial plateau fractures to help patients with these severe injuries to obtain optimal outcomes. Meanwhile, future multicentered, randomized, controlled studies should be implemented to test these outcomes.
References
Schatzker J, McBroom R, Bruce D (1979) The tibial plateau fracture. The Toronto experience 1968–1975. Clin Orthop Relat Res 138:94–104
Fracture and dislocation compendium (1996) Orthopaedic trauma association committee for coding and classification. J Orthop Trauma 10(Suppl 1):1–154
Shah SN, Karunakar MA (2006) Early wound complications after operative treatment of high energy tibial plateau fractures through two incisions. Bull NYU Hosp Jt Dis 65(2):115–119
Chin TYP, Bardana D, Bailey M et al (2005) Functional outcome of tibial plateau fractures treated with the fine-wire fixator. Injury 36(12):1467–1475
Katsenis D, Vasilis A, Panayiotis M et al (2005) Minimal internal fixation augmented by small wire transfixion frames for high-energy tibial plateau fractures. J Orthop Trauma 19(4):241–248
Krupp RJ, Malkani AL, Roberts CS et al (2009) Treatment of bicondylar tibia plateau fractures using locked plating versus external fixation. Orthopedics 32(8):559
Egol KA, Su E, Tejwani NC et al (2004) Treatment of complex tibial plateau fractures using the less invasive stabilization system plate: clinical experience and a laboratory comparison with double plating. J Trauma 57(2):340–346
Spagnolo R, Pace F (2012) Management of the Schatzker VI fractures with lateral locked screw plating. Musculoskelet Surg 96(2):75–80
Mahadeva D, Costa ML, Gaffey A (2008) Open reduction and internal fixation versus hybrid fixation for bicondylar/severe tibial plateau fractures; a systematic review of the literature. Arch Orthop Trauma Surg 128(10):1169–1175
Detsky AS, Naylor CD, O’Rourke K et al (1992) Incorporating variations in the quality of individual randomized trials into meta-analysis. J Clin Epidemiol 45:225–265
Ali AM, Yang L, Hashmi M et al (2001) Bicondylar tibial plateau fractures managed with the Sheffield Hybrid Fixator: biomechanical study and operative technique. Injury 32:86–91
Faldini C, Manca M, Pagkrati S et al. (2005) Surgical treatment of complex tibial plateau fractures by closed reduction and external fixation. A review of 32 consecutive cases operated. J Orthopaed Traumatol 6(4):188–193
Subasi M, Kapukaya A, Arslan H et al (2007) Outcome of open comminuted tibial plateau fractures treated using an external fixator. J Orthop Sci 12(4):347–353
Babis GC, Evangelopoulos DS, Kontovazenitis P et al (2011) High energy tibial plateau fractures treated with hybrid external fixation. J Orthop Surg Res 6(1):1–7
Catagni MA, Ottaviani G, Maggioni M (2007) Treatment strategies for complex fractures of the tibial plateau with external circular fixation and limited internal fixation. J Trauma 63(5):1043–1053
El Barbary H, Ghani HA, Misbah H et al (2005) Complex tibial plateau fractures treated with Ilizarov external fixator with or without minimal internal fixation. Int Orthop 29(3):182–185
Gaudinez RF, Mallik AR, Szporn M (1996) Hybrid external fixation of comminuted tibial plateau fractures. Clin Orthop Relat Res 328:203–210
Mikulak SA, Gold SM, Zinar DM (1998) Small wire external fixation of high energy tibial plateau fractures. Clin Orthop Relat Res 356:230–238
Stamer DT, Schenk R, Staggers B et al (1994) Bicondylar tibial plateau fractures treated with a hybrid ring external fixator: a preliminary study. J Orthop Trauma 8(6):455–461
El-Alfy B, Othman A, Mansour E (2011) Indirect reduction and hybrid external fixation in management of comminuted tibial plateau fractures. Acta Orthop Belg 77(3):349–354
Kataria H, Sharma N, Kanojia RK (2007) Small wire external fixation for high-energy tibial plateau fractures. J Orthop Surg (Hong Kong) 15(2):137–143
Dendrinos GK, Kontos S, Katsenis D et al (1996) Treatment of high-energy tibial plateau fractures by the Ilizarov circular fixator. J Bone Joint Surg Br 78(5):710–717
Yu Z, Zheng L, Zhang Y et al (2009) Functional and radiological evaluations of high-energy tibial plateau fractures treated with double-buttress plate fixation. Eur J Med Res 14(5):200
Luo CF, Sun H, Zhang B et al (2010) Three-column fixation for complex tibial plateau fractures. J Orthop Trauma 24(11):683–692
Ehlinger M, Rahme M, Moor BK et al (2012) Reliability of locked plating in tibial plateau fractures with a medial component. Orthop Traumatol Surg Res 98(2):173–179
Benirschke SK, Agnew SG, Mayo KA et al (1992) Immediate internal fixation of open, complex tibial plateau fractures: treatment by a standard protocol. J Orthop Trauma 6(1):78
Chan YS, Yuan LJ, Hung SS et al (2003) Arthroscopic-assisted reduction with bilateral buttress plate fixation of complex tibial plateau fractures. Arthroscopy 19(9):974–984
Katsenis D, Dendrinos G, Kouris A et al (2009) Combination of fine wire fixation and limited internal fixation for high-energy tibial plateau fractures: functional results at minimum 5-year follow-up. J Orthop Trauma 23(7):493–501
Barei DP, Nork SE, Mills WJ et al (2004) Complications associated with internal fixation of high-energy bicondylar tibial plateau fractures utilizing a two-incision technique. J Orthop Trauma 18(10):649–657
Stannard JP, Wilson TC, Volgas DA et al (2004) The less invasive stabilization system in the treatment of complex fractures of the tibial plateau: short-term results. J Orthop Trauma 18(8):552–558
Rasmussen PS (1973) Tibial condylar fractures. Impairment of knee joint stability as an indication for surgical treatment. J Bone Joint Surg Am 55:1331–1350
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the knee Society clinical rating system. Clin Orthop Relat Res 248:13–14
Honkonen SE, Jarvinen MJ (1992) Classification of fractures of the tibial condyles. J Bone Jt Surg Br 74(6):840–847
Hall JA, Beuerlein MJ, McKee MD (2009) Open reduction and internal fixation compared with circular fixator application for bicondylar tibial plateau fractures surgical technique. J Bone Joint Surg Am 91(Supplement_2_Part_1):74–88
Bugler KE, Clement ND, Duckworth AD et al (2012) The epidemiology of open fractures in adults. A 15-year review. Injury 43(6):891–897
Conflict of interest
All the authors declared that there is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yu, L., Fenglin, Z. High-energy tibial plateau fractures: external fixation versus plate fixation. Eur J Orthop Surg Traumatol 25, 411–423 (2015). https://doi.org/10.1007/s00590-014-1528-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-014-1528-7