Abstract
Objective
The aim of this study was to identify risk factors for surgical site infections and to quantify the contribution of independent risk factors to the probability of developing infection after definitive fixation of tibial plateau fractures in adult patients.
Methods
A retrospective analysis was performed at a level I trauma center between January 2004 and December 2010. Data were collected from a review of the patient’s electronic medical records. A total of 251 consecutive patients (256 cases) were divided into two groups, those with surgical site infections and those without surgical site infections. Preoperative and perioperative variables were compared between these groups, and risk factors were determined by univariate analyses and multivariate logistic regression. Variables analyzed included age, gender, smoking history, diabetes, presence of an open fracture, presence of compartment syndrome, Schatzker classification, polytrauma status, ICU stay, time from injury to surgery, use of temporary external fixation, surgical approach, surgical fixation, operative time, and use of a drain.
Results
The overall rate of surgical site infection after ORIF of tibial plateau fractures during the 7 years of this study was 7.8 % (20 of 256). The most common causative pathogens was Staphylococcus aureus (n = 15, 75 %). Independent predictors of surgical site infection identified by multivariate analyses were open tibial plateau fracture (odds ratio = 3.9; 95 % CI = 1.3–11.6; p = 0.015) and operative time (odds ratio = 2.7; 95 % CI = 1.6–4.4; p < 0.001). The presence of compartment syndrome (odds ratio = 3.4; 95 % CI = 0.7–15.9; p = 0.119), use of temporary external fixation (odds ratio = 0.5; 95 % CI = 0.2–1.7; p = 0.298), and ICU stay (odds ratio = 1.0; 95 % CI = 1.0–1.1; p = 0.074) were not determined to be independent predictors of surgical site infection.
Conclusions
Both open fracture and operative time are independent risks factors for postoperative infection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The surgical management of tibial plateau fractures aims to restore mechanical alignment, reduce the articular surface, and provide stable fixation that permits an early range of motion of the knee. Potential complications of tibial plateau open reduction and internal fixation (ORIF) include surgical site infection, deep venous thrombosis, knee stiffness, post-traumatic arthritis, malunion, and non-union. Deep infections are the most prevalent complications [1]. The reported incidence of surgical site infection following ORIF of tibial plateau fractures ranges from 2 to 11 % and higher than the overall rate seen in all orthopedic surgical procedures (1–3 %) [2–6].
It is important to identify risk factors for postoperative infection following ORIF of tibial plateau fractures to reduce morbidity, prevent cartilage destruction, and improve functional status of the joint. The objectives of the study were to (1) analyze the prevalence of surgical site infections in tibial plateau fractures treated by ORIF; (2) determine whether common risk factors are associated with the development of surgical site infections; and (3) quantify the contribution of independent risk factors to the probability of developing a surgical site infection.
Materials and methods
After institutional review board approval, we retrospectively identified patients who had sustained an intra-articular fracture of the proximal tibia as well as received ORIF for treatment by querying the Hospital Medical Informatics database for admissions coded with International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) procedure codes. Eligible operations were restricted to those performed by an orthopedic surgeon in patients 18 years of age or older. Three hundred and twenty-seven consecutive patients with tibial plateau fractures (332 cases) who underwent ORIF between January 2004 and December 2010 were identified. The initial radiographs for the 332 fractures were reviewed and classified according to Schatzker et al. [7]. There were 22 type I, 86 type II, 28 type III, 49 type IV, 47 type V, and 100 type VI fractures. Using the AO/OTA classification system, there were 50 41B1, 32 41B2, 103 41B3, 51 41C1, 37 41C2, and 59 41C3 type fractures.
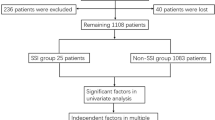
Seventy-six patients were excluded from the review. Sixty-nine cases had <6 months follow-up, two patients died of polytrauma after definitive fixation, and five patients had insufficient medical record data. The remaining 251 patients with 256 fractures formed the eligible study population for this retrospective review. Patients were divided into two groups, those who developed with surgical site infection and who did not. Preoperative and perioperative variables were compared between these groups.
This study population included 170 males (173 fractures) and 81 females (83 fractures) ranging in age from 18 to 78 years (mean, 43 years). The average follow-up was 18 months. The injury was predominantly due to high-energy mechanism. One hundred and forty-six were injured in motor vehicle accidents, 65 fell from a height, 26 were injured in sporting activity, eight had sustained direct blows, two had gunshot injuries, and nine were injured from other causes.
Thirty cases (11.7 %) were open injuries. Five cases were type I, 14 were type II, seven were type III-A, two were type III-B, and two were type III-C based on the Gustilo and Anderson classification [8, 9]. Two of these open injuries and two close tibial plateau fractures sustained disruption of the popliteal artery requiring urgent revascularization. Compartment syndrome was diagnosed and treated with fasciotomy in 11 cases (4.3 %). Six of these cases were able to undergo delayed primary wound closure, and the remaining five required split-thickness skin grafting for wound coverage. Sixty-two cases (24.2 %) stayed in the ICU during the initial admission. The mean length of ICU stay of all the patients was 2.9 days. Temporary spanning external fixation was performed in 96 cases (37.5 %) secondary to the severity of the local soft-tissue injury or associated life-threatening injuries. The average preoperative stay in patients treated with temporary external fixation was 9.5 days, compared to 5 days in those without temporary external fixation. One hundred and nine (42.6 %) cases with a bicondylar fracture of tibial plateau were identified. Of these fractures, only 59 cases (23 %) were treated with dual-plate fixation through two surgical exposures—an anterolateral exposure and a separate posteromedial exposure.
Surgical site infection was defined using standard Centers for Disease Control (CDC) definitions [10, 11]. Deep surgical site infections involved deep soft tissue, muscle, or fascia and had an onset within 1 year after the initial surgery. Superficial surgical site infection, defined as an infection involving only skin or subcutaneous tissue at the incision site and occurring within 30 days after operation, was also included in this study. Operative cultures were routinely grown for 5 days. No positive findings were discarded as contaminants. Swabs were most commonly sent rather than tissue samples.
Medical records from the initial procedure and any subsequent operative debridements were reviewed. Data collected included demographic characteristics, patient comorbidities (tobacco use, diabetes, HIV/AIDS, polytrauma), date of injury, mechanism of injury, side of injury, type of fracture (open or closed), length of ICU stay, preoperative stay, compartment syndrome, and temporary external fixation. The treatment regimen, including date of fixation, surgical approach, type of fixation (screw, plate, or dual plates), use of a drain, and operative time, was also recorded. Onset of infection, causative pathogens, times of irrigation and debridement, and the type and duration of antibiotics were recorded only for patients who developed a surgical site infection.
We defined polytrauma as trauma to more than one of the musculoskeletal, abdominal, cardiothoracic, urogenital, vascular, and central nervous systems. Multiple isolated orthopedic injuries were not classified as polytrauma unless they were associated with hemodynamic instability [2]. Owing to the anatomic characteristic, and to have a sufficient number to perform the analysis, we pooled patients with Schatzker types I, II, III, and IV fractures and as unicondylar injuries and Schatzker types V and IV fractures as bicondylar injuries. Patients who underwent combined anterolateral and posteromedial approaches for tibial plateau fracture were defined as dual incisions.
Statistical analyses were performed with use of SPSS software for Windows (version 20; SPSS Inc., Chicago, IL, USA). Univariate analysis of continuous variables was performed with use of the Student’s t-test for normally distributed variables, and the Mann–Whitney U-test for non-normally distributed variables. The Fisher’s exact test or Chi-square test was used for dichotomous variables. Multivariate analyses were performed with use of logistic regression to determine the independent predictors of surgical site infection. Variables for which the p value was ≤0.10 in the univariate analysis were included as candidate variables in the multivariate models. Variables were selected for inclusion in the final models with use of a back stepwise selection process. We controlled for the confounding effects of covariates on selected variables. Based on the final multivariable model, we achieved a prediction algorithm with reliable odds ratios and 95 % confidence intervals [12]. Only variables for which the p value was ≤0.05 in the final model were considered significantly. All p values were two-sided.
Results
Overall, there were 20 cases with a surgical site infection after ORIF of tibial plateau fractures, an incidence of 7.8 %. The mean interval between the operation and the diagnosis of the infection was 42.8 days, with a minimum of 3 days and a maximum of 189 days for a patient with osteomyelitis. Twelve of the 20 cases developed postoperative infection within the first 4 weeks.
Five cases had polymicrobial infection, and three cases had no positive culture regardless of apparent clinical signs of infection. Staphylococcus aureus was the most common causative pathogen in 15 cases, and approximately half of these pathogens were methicillin resistant. Pseudomonas aeruginosa was found in three cases followed by Enterobacter species in two cases. Acinetobacter baumannii, Enterococci species, Streptococci species, and Serratia species were each identified in one case, respectively (Table 1).
In the univariate analysis (Table 2), we found that three variables had significantly increased risk of surgical site infections. Preoperative predictors included open fracture (infection rate 20 %; p = 0.019) and compartment syndrome (infection rate 27.3 %; p = 0.019). Perioperative predictor was operative time (p < 0.001). However, the multivariate analysis eliminated compartment syndrome as an independent predictor for the outcome. We identified that operative time remained an independent predictor of surgical site infection (odds ratio = 2.7; 95 % CI = 1.6, 4.4; p < 0.001) (Table 3). Additional independent predictor of surgical site infection was open fracture (odds ratio = 3.9; 95 % CI = 1.3, 11.6; p = 0.015). The multivariable predictive model of SSI was reliable (Hosmer–Lemeshow statistic, p = 0.64) and accurate (c-index = 0.93).
Sixteen infections (6.2 %) were defined as deep and four (1.6 %) were defined as superficial.
All deep surgical site infections were treated with intravenous culture-specific antibiotics in the hospital and needed one or more additional surgical treatments in addition to locally implanted antibiotic-impregnated beads. The average number of irrigation and debridements was 2.1 (range 1–7). Hardware was removed in six cases that were unresponsive to suppressive therapy, whereas hardware was maintained in the other ten cases. Since three of these hardware-removed cases were delayed infections, they were treated with casts or splints and achieved fracture union. The remaining three cases that were acutely postoperative infections were revised to Ilizarov ring external fixation. In the group of 16 deep surgical site infections, 12 cases achieved a satisfactory union and one case received a plate revision to correct a previous articular collapse. The three remaining cases that had persistent non-union were treated by autogenous bone grafting once the wounds were clinically healed. One of these cases still had persistent non-union at the time of the most recent follow-up.
Of the four superficial wound infections, three cases responded well to local wound care and oral antibiotics. The remaining case underwent a single surgical procedure and primary closure followed by intravenous antibiotics. All these cases were suppressed with antibiotics and achieved successful union, although one patient was considered to have mild valgus deformity of the right knee.
Discussion
Numerous previous studies have analyzed the risk factors for surgical site infections following surgical treatment in patients with orthopedic trauma [2, 13–18]. Identified risk factors have included older age, diabetes, smoking, body mass index (BMI), ICU stay, Morel–Lavalle′e lesion, use of a drain, number of operations, congestive heart failure (CHF), contaminated surgery, inadequate chemoprophylaxis, longer preoperative stay, and steroid use. In the current study, we identified two independent predictors of surgical site infections after ORIF of tibial plateau fractures, namely operative time and open injury.
Our study had several limitations. As a retrospective study, the quality of the data relied on the accuracy and completeness of the electronic medical records. We also probably excluded many factors that may be associated with the development of surgical site infection due to incomplete records to draw a conclusion. Management of the soft tissues, fracture classification, immediate or delay ORIF, and preoperative plan relied on the clinical experience of the attending surgeons. Another important limitation is related to follow-up of patients. Since only patients who had been followed up at least 6 months were chosen for study, we made the assumption that a patient who did not return specifically for treatment of an infection within the next 6 months did not have an infection. It is possible that more surgical site infections may have developed in the non-infection group leading us to underestimate the incidence of wound infection and the association between a given risk factor and the risk of a failed outcome. Given that the majority of orthopedic SSIs are diagnosed within the first month, we believe the results of our study are reliable [13, 19]. Finally, in the current study, we included all types of Schatzker classification. However, because of the relatively low incidence of wound complication, the small numbers of subsets of patients would not permit us to identify a significant difference in individual fracture types. Therefore, the patients were divided into unicondylar plateau fractures and bicondylar plateau fractures, which is based on anatomic characteristic, surgical approach and application of implants.
We did not specifically examine the effect of estimated blood loss, which we felt was not accurately determined, or blood transfusions. Fifty-two patients received one or more blood transfusions, but only 5 of these patients had failure following debridement and primary wound closure. The blood transfusions occurred early following the trauma and were associated with other organ injuries. In contrast, the debridement and primary closure were commonly performed many weeks later.
For our polytrauma definition, we used the criteria of Bachoura et al. [2] rather than the injury severity score (ISS). The average ISS in our defined polytrauma group was 25.4 compared to 8.4 in our non-polytrauma group.
Bachoura et al. [2] studied 1,611 patients who underwent 1,783 trauma-related surgeries over a 3-year period. This study found that tibial plateau injuries increased the incidence of surgical site infections more than twofold compared with other sites of injury. This finding might be attributed to its subcutaneous location and tenuous soft-tissue coverage, which was similar to elbow or calcaneus [20, 21]. In addition, most tibial plateau fractures were often the result of high-energy blunt trauma that resulted in severe soft-tissue disruption. Therefore, the treating surgeon may be confronted with the dilemma of minimizing further soft-tissue injury and decreasing wound complications, particularly in high-energy comminuted fractures.
In the current study, we confirmed longer operative time to be associated with postoperative infection. In the univariate analysis, patients who developed postoperative infections had a significantly longer operative time (2.9 ± 1.0 h) than those without postoperative infections (2.1 ± 0.8 h; p < 0.001). We assume that high-energy comminuted articular fractures need more time to achieve a satisfactory reduction. While the infection rate was higher in bicondylar fracture (11 of 109, 10.1 %) compared to unicondylar fracture (9 of 147, 6.1 %), this difference was not statistically significant. Although dual plates were not performed in all bicondylar fractures, dual plates (7 of 59, 11.9 %) had a greater risk of infection than unilateral plate/screws (13 of 197, 6.6 %), and this difference also was not statistically significant. Complex fractures theoretically require larger incisions, more extensive exposure, more blood loss, and prolonged anesthesia duration, which are more likely to result in infection [22–25]. In order to achieve lower operative time and better results, the surgeon must have a thorough understanding of the local anatomy, a thorough understanding of the fracture pattern and location based on a CT scan, and a well-prepared preoperative plan to minimize preventable delays.
We also found an association between open fracture and surgical site infection, which was consistent with previous studies [25–28]. In this study, 27 of 30 open fractures (90 %) were involved in a motor vehicle accident or fell from a substantial height. In both cases, the surrounding soft tissues were disrupted to a variable degree. Thorough surgical debridement and irrigation were performed in the operating room within 8 h of injury, either at our institution or at an outside hospital prior to transfer. Only five cases (16.7 %) were treated with definitive stabilization at that time of initial debridement. One case was treated with a temporary splint, and the remaining 24 cases (80 %) were treated with temporary spanning external fixation. Patients returned to operating room for serial irrigation and debridements after 24–48 h, based on the degree of contamination and soft-tissue damage. Appropriate soft-tissue coverage was achieved with split-thickness skin graft, free muscle flaps, or rotational muscle flaps within 2 weeks. In addition, antibiotic prophylaxis was started promptly and provided for the first 24 h following injury. Unfortunately, surgical site infections after definitive fixation developed still in six cases (20 %). Higher-energy fractures, worse soft-tissue injuries, and comminution of the fracture site with the outside environment may be factors responsible for this association. Additionally, extensive dissection through the tenuous soft-tissue envelope to achieve accurate reduction and apply stabilizing implants probably contributes to the increased postoperative infection rates [1, 25, 28]. Stannard et al. [27] reported a 6.3 % incidence of deep infection developed in open tibial plateau fractures utilizing the less-invasive stabilization system (LISS) internal fixator and suggested LISS was an acceptable alternative for treatment of these fractures.
We did not find compartment syndrome to be independent predictor of surgical site infection, which was very similar to our previous study [29]. In this study, all 11 cases with an associated compartment syndrome were treated with formal four-compartment open releases. It is surprising that in the current study, diabetes was not found to be an independent risk factor for surgical site infection. This finding might be attributed to careful perioperative monitoring and control of blood glucose level in diabetes patients, or more likely, the relatively small number diabetes patients included in this study may have resulted in an underpowered statistical assessment [30, 31]. Several previous investigators have confirmed smoking places of patients at an increased risk for surgical site infection following orthopedic surgery [16, 17, 32]. However, our study also did not show tobacco use–effected infection rates. Although a wound drain was more likely to be applied in complex injuries or extensive dissection, drain use has been shown to provide no benefit on rates of infection, which may explain why we found wound drain use was not a significant risk factor for postoperative infection [33].
Prevention of wound complication after surgical management of tibial plateau fractures, particularly associated with serious soft-tissue injury, remains difficult and challenging. The results of this study identified that open fracture and operative time independently predicted surgical site infection following ORIF. Therefore, we recommend that extra vigilance be exercised when managing patients with open tibial plateau fractures. Additionally, our study indicated the need of close attention to operative techniques to limit operating time with an aim of lowering the risk of postoperative wound infection.
References
Moore TM, Patzakis MJ, Harvey JP (1987) Tibial plateau fractures, definition, demographics, treatment rationale and long term results of closed traction management or operative reduction. J Orthop Trauma 1(2):97–119
Bachoura A, Guitton TG, Smith RM, Vrahas MS, Zurakowski D, Ring D (2011) Infirmity and injury complexity are risk factors for surgical-site infection after operative fracture care. Clin Orthop Relat Res 469:2621–2630
Wadell AP, Johnston DWC, Meidre A (1981) Fractures of tibial plateau, a review of 95 patients and comparison of treatment methods. J Trauma 2:376–381
Papagelopoulos PJ, Partsinevelos AA, Themistocleous GS, Mavrogenis AF, Korres DS, Soucacos PN (2006) Complications after tibia plateau fracture surgery. Injury 37:475–484
Whitehouse JD, Friedman ND, Kirkland KB, Richardson WJ, Sexton DJ (2002) The impact of surgical-site infections following orthopedic surgery at a community hospital and a university hospital: adverse quality of life, excess length of stay, and extra cost. Infect Control Hosp Epidemiol 23:183–185
Centers for Disease Control and Prevention, National Center for Health Statistics (1997) Vital and Health Statistics, Detailed Diagnoses and Procedures, National Hospital Discharge Survey 1994. Department of Health and Human Services, Hyattsville, MD
Schatzker J, McBroom R, Bruce D (1979) The tibial plateau fracture. The Toronto experience 1968–1975. Clin Orthop 138:94–104
Gustilo RB, Anderson JT (1976) Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses. J Bone Joint Surg Am 58:453–458
Gustilo RB, Mendoza RM, Williams DN (1984) Problems in the management of type III (severe) open fractures: a new classification of type III open fractures. J Trauma 24:742–746
Garner JS, Jarvis WR, Emori TG, Horan TC, Hughes JM (1988) CDC definitions for nosocomial infections, 1988. Am J Infect Control 16:128–140
Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR (1999) Guideline for prevention of surgical site infection, 1999. Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol 20:250–278
Vittinghoff E, McCulloch CE (2007) Relaxing the rule of ten events per variable in logistic and Cox regression. Am J Epidemiol 165:710–718
Suzuki T, Morgan SJ, Smith WR, Stahel PF, Gillani SA, Hak DJ (2010) Postoperative surgical site infection following acetabular fracture fixation. Injury. 41(4):396–399
Herruzo-Cabrera R, López-Giménez R, Diez-Sebastian J, Lopez-Aciñero MJ, Banegas–Banegas JR (2004) Surgical site infection of 7301 traumatologic inpatients (divided in two subcohorts, study and validation): modifiable determinants and potential benefit. Eur J Epidemiol 19(2):163–169
SooHoo NF, Krenek L, Eagan MJ, Gurbani B, Ko CY, Zingmond DS (2009) Complication rates following open reduction and internal fixation of ankle fractures. J Bone Joint Surg Am 91:1042–1049
Nåsell H, Ottosson C, Törnqvist H, Lindé J, Ponzer S (2011) The impact of smoking on complications after operatively treated ankle fractures-A follow-up study of 906 patients. J Orthop Trauma 27:1–8
Castillo RC, Bosse MJ, MacKenzie EJ, Patterson BM, LEAP Study Group (2005) Impact of smoking on fracture healing and risk of complications in limb-threatening open tibia fractures. J Orthop Trauma 19(3):151–157
Koval KJ, Zhou W, Sparks MJ, Cantu RV, Hecht P, Lurie J (2007) Complications after ankle fracture in elderly patients. Foot Ankle Int 28:1249–1255
Ridgeway S, Wilson J, Charlet A, Kafatos G, Pearson A, Coello R (2005) Infection of the surgical site after arthroplasty of the hip. J Bone Joint Surg Br 87:844–850
Morrey BF, Bryan RS (1982) Complications of total elbow arthroplasty. Clin Orthop Relat Res 170:204–212
Heier KA, Infante AF, Walling AK, Sanders RW (2003) Open fractures of the calcaneus: soft-tissue injury determines outcome. J Bone Joint Surg Am 85-A(12):2276–2282
Fang A, Hu SS, Endres N, Bradford DS (2005) Risk factors for infection after spinal surgery. Spine 30(12):1460–1465
Olsen MA, Nepple JJ, Riew KD, Lenke LG, Bridwell KH, Mayfield J, Fraser VJ (2008) Risk factors for surgical site infection following orthopaedic spinal operations. J Bone Joint Surg Am 90(1):62–69
Lee J, Singletary R, Schmader K, Anderson DJ, Bolognesi M, Kaye KS (2006) Surgical site infection in the elderly following orthopaedic surgery. Risk factors and outcomes. J Bone Joint Surg Am 88:1705–1712
Young MJ, Barrack RL (1994) Complications of internal fixation of tibial plateau fractures. Orthop Rev 23:149–154
Zalavras CG, Patzakis MJ, Holtom PD, Sherman R (2005) Management of open fractures. Infect Dis Clin North Am 19(4):915–929
Stannard JP, Finkemeier CG, Lee J, Kregor PJ (2008) Utilization of the less-invasive stabilization system internal fixator for open fractures of the proximal tibia: a multi-center evaluation. Indian J Orthop 42(4):426–430
Mallik AR, Covall DJ, Whitelaw GP (1992) Internal versus external fixation of bicondylar tibial plateau fractures. Orthop Rev 21:1433–1436
Hak DJ, Lee M, Gotham DR (2010) Influence of prior fasciotomy on infection after open reduction and internal fixation of tibial plateau fractures. J Trauma 69(4):886–888
Furnary AP, Zerr KJ, Grunkemeier GL, Starr A (1999) Continuous intravenous insulin infusion reduces the incidence of deep sternal wound infection in diabetic patients after cardiac surgical procedures. Ann Thorac Surg 67:352–362
Sakamoto H, Fukuda I, Oosaka M, Nakata H (2003) Risk factors and treatment of deep sternal wound infection after cardiac operation. Ann Thorac Cardiovasc Surg 9(4):226–232
Folk JW, Starr AJ, Early JS (1999) Early wound complications of operative treatment of calcaneus fractures: analysis of 190 fractures. J Orthop Trauma 13:369–372
Tjeenk RM, Peeters MP, van den Ende E, Kastelein GW, Breslau PJ (2005) Wound drainage versus non-drainage for proximal femoral fractures: a prospective randomised study. Injury 36:100–104
Conflict of interest
All authors confirm that they have no financial and personal relationships with any commercial party, which could inappropriately influence this work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lin, S., Mauffrey, C., Hammerberg, E.M. et al. Surgical site infection after open reduction and internal fixation of tibial plateau fractures. Eur J Orthop Surg Traumatol 24, 797–803 (2014). https://doi.org/10.1007/s00590-013-1252-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-013-1252-8