Abstract
Backgrounds
Treatment for bone defect remains a challenge for orthopedists. Bone transport gives an effective alternative, which can be performed with an external fixator alone or combined with an intramedullary nail. Each has its advantages and disadvantages. We present a retrospective study to find out the optimal choice by evaluating the outcomes of treatment for femoral bone defect with two methods.
Methods
Two groups of patients, the monolateral external fixator alone (group A, n = 13) and the monolateral external fixator combined with intramedullary nail (group B, n = 15), were compared. Duration of the external fixator, external fixator index, radiographic consolidation index, complication, and total cost for treatment was also recorded. A modified classification of the Association for the Study and Application of the Method of Ilizarov (ASAMI) was used to assess results in two groups of patients; another SF-36 health survey questionnaire was used to assess the life qualities patients of two groups.
Results
Healing was achieved in 13/13 and 13/15 of the two groups, respectively. The rates of complications were significantly higher in the group A. Two patients performed amputations because of persistent deep infections in group B. Statistically significant difference was found when comparing ASAMI scores and categories of the SF-36 health survey.
Conclusions
Bone transport by monolateral external fixator with the use of intramedullary nail reduces the incidence of complication and the duration of external fixator time that give patients a better life quality in both physical and emotional. However, if chronic osteitis exists, bone transport should be treated with monolateral external fixator alone due to a lower rate of amputations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ilizarov technique has attached more and more attention in dealing with nonunion of long bone. Under the guidance of tension–stress rule, bone transport, one type of Ilizarov technique, sheds a new light on treatment for long bone defects, especially combined with limb shortening [1, 2]. Studies also show that regenerate bone formed by bone transport is mechanically superior to the bone formed by bone grafting. Compared with conventional circular frame style, bone transport using the monolateral external fixator has advantages of lighter, less soft-tissue damage, allowing early physical exercise and partial weight-bearing [3]. However, there are complications including malalignment, re-fractures, nonunion in the docking site, and the lengthy treatment time that adds patient discomfort and the possibility of pin track infection. Both patients and orthopedic surgeon are willing to remove the external fixator earlier to decrease the discomfort and complications.
Bone transport over an intramedullary nail can shorten the period of external fixator, guarantee the anatomical length and alignment of regenerated bone, improve the comfort of patients during the period of treatment, and allow early removal of external fixator and rehabilitation [4]. However, this procedure has no capability to correct associated deformities, slow consolidation, and add the risk of spreading infection of either bone defect site or pin track into intramedullary cavity [5]. Moreover, it seems to add additional costs to patients, which is also a major concern be taken into account in developing country. However, to date, there are no authoritative guidelines for choosing the two methods when dealing with femoral bone defects.
Our retrospective study was designed to evaluate the clinical results and related complications of bone transport with or without the use of intramedullary nail when dealing with femoral bone defects. In this single-department retrospective study, we propose to find out the optimal indication of two methods when dealing with femoral bone defects.
Patients and methods
Patients enrolled in the study were those who fulfilled the inclusion criteria for this study in our hospital between June 1994 and January 2008. Inclusion criteria were patients who suffered a >5 cm segmental femoral bone defect (combined with limb shortening or not) caused by high energy trauma or debridement for osteomyelitis. According to Paley et al. [6] classification of nonunion, all patients were either type B1 (bone defect more than 1 cm with no shortening of the limb) or type B3 (bone defect more than 1 cm combined with limb shortening). Exclusion criteria were patients who combined with neurologic or vascular defect in the fractured limb; patients with systemic illness that could affect immunologic status such as diabetes mellitus, liver cirrhosis, and AIDS. Bone transport by the use of monolateral external fixator used alone is regarded as group A, combined with an intramedullary nail as group B.
The recorded data of patients included the patient’s age, gender, smoking habits, the number of previous operations, and the presence of chronic infection before admitting into our department (defined by positive cultures for more than 2 months preoperatively). Preoperative radiographs were taken (anteroposterior and lateral) to assess the size of bone defect, to determine the planes of the osteotomies, and the length and diameter of the intramedullary nails in group B.
Operation technique
As described in our previous studies [7], under intraoperative C-arm guidance, two or three proximal pins, 4.5 mm diameter, were inserted at the level of the lesser trochanter at right angles to the anatomical axis of the femur, approximately 2–3 cm below the level, which had been selected for the osteotomy and the level of the superior pole of the patella, respectively. In group B, an intramedullary nail 1.5 mm larger than that of the selected one was firstly temporarily inserted and then pins inserted the same way as group A. All the pins were positioned beyond the nail. The intramedullary nail was then removed. In both group A and B, all pins should be inserted in the same plane. The femoral shaft was exposed subperiosteally and a transverse osteotomy was then made at the preselected level. In group B, the nail was re-inserted and secured distally with a locking screw. The excess length of the nail was left in the soft tissues proximally. The periosteum was sutured and the wound closed with drainage. The external fixator was attached with a 2-cm gap between it and the thigh to give space for possible postoperative swelling. In group B, attention should be paid to avoid contact between the pins and the intramedullary nail, and the distal locking screw should be placed 2–3 cm away from the pins.
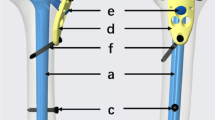
Monolateral external fixator
A three-segment monolateral external fixator (Third Medical Instrument Company, Wujin, China) (Fig. 1) was used for bone transport in all patients. It has two screw rods and two link rails and is a stable rectangular plane fixator, which is connected to the bone by the link rails and threaded pins. The three-segment fixator make the bone transport easily perform just by adjusting the middle segment of screws toward the lengthening direction: firstly, the press boards (used to make the fixator more stable) are removed; secondly, the offside locking bolt of middle segment of screws was rotated toward the lengthening direction; finally, the press boards were locked again to stabilize the external fixator.
A 3-day course of intravenous broad-spectrum antibiotics was given to all patients postoperatively. Partial weight-bearing and physical exercises for rehabilitation were encouraged the second day after operation. Distraction was started 7 days postoperatively at a rate of 1.0 mm/36 h, then reduced to 1.0 mm every 48 h when the regenerate bone length had reached approximately 6.0 cm [14].
All patients were followed up at the outpatient unit of our department. Radiological examination [both anteroposterior (AP) and lateral view of plain X-ray] was carried out every 15 days to assess new bone formation, the alignment of femoral shaft, and the situation of pin sites. When bone transport was finished, proximal locking screws were inserted into the nail and the external fixator removed to facilitate unrestricted rehabilitation in group B. Decision to remove the fixator (external in group A and intramedullary nail in group B) was made when sufficient consolidation was obtained (at least three cortices observed in plain X-ray examination).
A modified classification of the Association for the Study and Application of the Method of Ilizarov (ASAMI) was used to assess results in two groups of patients [8]. Results were evaluated according to bone and functional categories. Bone results were classified as four grades according to the described criteria: an excellent bone result was one with union (three cortices in AP and lateral view of plain X-ray), no infection, deformity of <7°, and length discrepancy of <2 cm in the femur; a good result was union plus any two of the others; a fair result was union plus one of the others; a poor result was nonunion or re-fracture or none of the others.
Functional results were based on five criteria: limited range of movement of the knee, pain, abnormal gait, soft-tissue injury, and inactive individual to perform daily life or work. Four grades were classified according to the described criteria: excellent, good, fair, and poor. An excellent result was an active individual with none of the other four criteria; good with one or two of the other four criteria, fair with three or four of the other criteria or amputation, and poor was an inactive individual regardless of the other criteria.
Another SF-36 health survey questionnaire was used to assess the life qualities patients of two groups that included physical functioning (PF), role-physical (RP), bodily pain (BP), general health (GH), vitality (VT), social functioning (SF), role-emotional (RE), and mental health (MH).
Duration of the external fixator, external fixator index (the duration of external fixator in days per centimeter of distraction), radiographic consolidation index (days until radiographic bone consolidation per centimeter of distraction), complication, and total cost for treatment were also recorded for statistical analysis.
Statistical analysis
Statistical significance was evaluated between the groups using Pearson’s χ2 for categorical values, and Student’s t test was used for continuous data. A P value ≤0.05 was regarded to be statistically significant. All statistical analyses were performed using SPSS 13.0. All values are presented in the form of mean ± SD (standard deviation).
Results
Total 32 patients were included in this study according to the criteria for inclusion. Three patients were lost in the follow-up (two in group A and one in group B). One patient in group B died for reasons unrelated to the treatment. A total of 28 patients were reassessed at follow-up, 13 of who were treated only with the monolateral external fixator (group A) and 15 combined with the intramedullary nail (group B). Nine patients were type B1 and 19 type B3. The average clinical follow-up was 81.4 ± 6.4 months and 77.7 ± 8.9 months. The mean age of the patients in group A was 32.2 ± 5.1 years and 33.2 ± 4.7 years in group B. 38.5 % of patients in group A and 40 % in group B were women. The duration of bone defect was 22.8 ± 5.9 months in group A and 24.1 ± 6.1 months in group B. 38.5 % of patients in group A and 40 % in group B were left side. The etiology of the bone defect was traumatic in 4 cases (30.8 %) in group A and 4 cases (26.7 %) in group B, debridement for osteomyelitis in 9 cases (69.2 %) in group A and 11 cases (73.3 %) in group B. Most of the patients were transferred from other hospitals, where they had previously undergone one or more surgical procedures (2.6 ± 1.3 in group A and 2.9 ± 1.5 in group B). Three patients (23.1 %) in the group A and four (26.7 %) in group B had chronic osteitis prior to bone transport. 30.8 % of the group A and 33.3 % of the group B patients were smokers. The defect length measured 8.9 ± 2.3 cm in the group A and 8.5 ± 3.1 cm in the group B. There was no statistic significant difference between the study groups in demographic data (Table 1).
In group A, bone healing was observed in all 13 patients both at the docking site and lengthening area (Fig. 2a–g); however, among them, there were 7 patients with residual deformity more than 7°. The average duration of external fixator was 14.8 ± 6.9 months. The average radiographic consolidation index of the distraction callus was 240.6 ± 2.7 days/cm. Meanwhile, the external fixator index was 132.1 ± 2.9 days/cm. In group B, 13 patients had completed bone healing both at the lengthening area and the docking site with no deformity and infection (Fig. 3a–g). The average duration of external fixator was 4.7 ± 1.9 months followed by intramedullary nail fixator alone whose average duration was 5.4 ± 4.6 months. The average radiographic consolidation index was 227.8 ± 2.4 days/cm, whereas the average external fixator index was 131.4 ± 2.3 days/cm. There is statistic significant difference regarding the duration of external fixator between two groups with no difference regarding the external fixator index and radiographic consolidation index (Table 2).
a Preoperative anteroposterior radiograph of a 24-year-old male with 13.5 cm of femoral bone defect after debridement for post-traumatic osteomyelitis. b After osteotomy and application of the monolateral external fixator, bone transport began with the middle group of pins move forward proximally. c Bone transport was finished. New bone formation can be observed in lengthening area and docking site. d Consolidation can be observed in the plain X-ray 26 months postoperatively. e 2 years after the removal of monolateral external fixator. f There is no presentation of limb discrepancy in the final follow-up. g The range of movement of knee was between 0° (extension) and 45° (flexion). The patient felt satisfactory with the clinical outcome
a A 19-year-old female presented with 10.5 cm of femoral bone defect after debridement for post-traumatic osteomyelitis in preoperative anteroposterior radiograph. b After osteotomy, application of the monolateral external fixator and an intramedullary nail, bone transport began with the monolateral external fixator over the intramedullary nail. c Bone transport process (2 months postoperatively). d Bone transport was finished. New bone formation can be observed in lengthening area and docking site (6 months postoperatively and eliminating the monolateral external fixator later). e Consolidation can be observed in the plain X-ray 8 months postoperatively (eliminating the intramedullary nail later). f 2 years after the removal of monolateral external fixator and intramedullary nail. g There is no presentation of limb discrepancy in the final follow-up
In group A, complications associated with the use of the fixator included aseptic pin loosening in three patients that required reinsertion of the screws; superficial pin track infection in 11 cases that responded to oral or intravenous antibiotics; re-fracture of the lengthening callus was observed in two cases following removal of the fixator, which required correction and stabilization with a plastic cast to healing; nonunion of the docking site in three cases, which required a second surgical operation of bone grafting. Healing was achieved in all patients undergoing these procedures. Six patients had residual knee limited range of movement on the final follow-up (40° <the opposite side), the rest achieved full range of knee movement on final follow-up after a longer duration of rehabilitation therapy (Table 2).
In group B, none of the aseptic pin loosening and re-fracture of the lengthening callus was observed. However, two patients had amputations due to persistent deep bone infections. The two amputated patients were also observed chronic osteitis in defect area preoperatively and the presentation of pin track infection postoperatively. The other 13 patients recover full range of knee joint movement 3 months after the removal of external fixator (Table 2).
The results of bone outcome were six excellent, two good, and five poor in group A compared with twelve excellent, one good, and two poor in group B. The results of functional outcome were seven excellent, four good, and two fair in group A compared with 13 excellent and two fair in group B. Although the two amputations were considered a poor bone outcome in the group B, these patients were functioning well without significant complaints and were able to perform all activities of daily living without significant pain. So we categorized the two cases as fair functional outcomes. There is statistically significant difference regarding the bone outcome on final follow-up but no difference regarding functional outcome between both groups (Table 3).
The results of the SF-36 health survey showed the following mean scores for the group A/group B, respectively: 59.7/78.2 for PF, 40.9/45.3 for RP, 57.9/75.2 for BP, 61.2/68.8 for GH, 51.9/58.7 for VT, 63.7/68.5 for SF, 57.6/78.5 for RE, and 68.2/72.4 for MH. There was statistically significant difference between the study groups in categories of PF, BP, and RE (Table 4). Due to the early removal of external fixator and rehabilitation, patients in group B feel more satisfaction and comfort because of the easier return to normal daily life and social activity.
The total costs for treatment include all expenses to treat bone defect and related complications if occurred till the end of treatment. The total cost for treatment was calculated as the price made by Chinese food and Drug Administration and Hunan Food and Drug Ministry in 2011. This aims to eliminate the inflation during the period of 14 years. There is no statistically significant difference between both groups (Table 2).
Discussion
Long bone defects remain a great challenge to the orthopedists all over the world. Many methods are used to deal with the dilemma such as transplantation of vascularized or vascularized autogenous bone [9, 10], allograft bone transplantation, reconstruction by cylindrical titanium mesh packed with cancellous bone [11] or other biomaterial composite, and bone transport [12]. At present, it is the vascularized autogenous bone grafting and bone transport that were regarded as golden standard when coping with femoral bone defect [13, 14].
Many donor sites can be candidate for vascularized bone grafting such as iliac crest, ribs, or fibula. Generally speaking, vascularized bone grafting is optimal choice for the cases of bone combined with soft-tissue defect. However, there are some drawbacks with vascularized bone grafting. Sophisticated microsurgical techniques are required to guarantee the success of vascularized bone grafting operation; a well-vascularized circumstance without infection was also mandatory; morbidity in donor site, long remodeling time, and high fracture rate are also issues be taken into account [9, 13]. Finally, it is not suitable for vascularized bone grafting using in cases with limb discrepancy (like femoral bone defect combined with shortening) [15].
Bone transport gives orthopedics surgeon the tool to achieve limb lengthening and filling of intercalary bone defects. Compared to circular style, monolateral style make patients feel more easily in daily life and a moderate range of joint motion was allowed postoperatively due to the low number of muscular transfixations; monolateral fixator is similar to the conventional external fixator, which is easy for orthopedics surgeon to master the technique for bone transport. In our department, good results were achieved in the fields of long bone nonunion and limb deformity using the monolateral external fixator [16–18]. Meanwhile, complications also occurred such as pin track infection and pin loosening due to the lengthy treatment time, malalignment, malunion, deformity, and long rehabilitation period. Many modified Ilizarov techniques have been tried to shorten the duration of external fixator to avoid the complications due to long time of external fixator.
Bone transport by monolateral external fixator with the use of intramedullary nail is one of the modified techniques [19]. This technique allows early removal of external fixator and rehabilitation, which can minimum the complication of long time external fixator. However, complications were also reported included slow consolidation and deep infection throughout whole intramedullary cavity [20]. Moreover, it seems that using additional intramedullary nail adds the cost to patients, which is also a concern during the treatment in developing country.
In our study, there were no significant statistical difference between two groups regarding the external fixator index and radiographic consolidation index; this indicated that bone transport with the use of intramedullary nail did not slow the rate of new bone consolidation compared with the use of external fixator alone. The effect of revascularization after reaming and earlier functional rehabilitation compensated for damage to the endosteal blood supply by intramedullary nailing. One study of Sun et al. [21] showed that callus progression in limb lengthen with intramedullary nail presented a more favorable way compared to without intramedullary nail. The same results were observed in our study (significant statistic difference regarding the bone outcomes of ASAMI scores between two groups). In this study, we employed slower distraction rates than other studies (a rate of approximately 1.0 mm every 36 h was used initially, then reduced to 1.0 mm every 48 h when the length reached 6.0 cm). However, the frequency of distraction was higher than some other studies (4 times/36 h before the length reached 6.0 cm and 4 times/48 h when the length reached 6.0 cm). Studies showed that high frequency of distraction can produce better new bone consolidation [22–24]. High-frequency distraction resulted in fewer microtraumas in the distraction area due to relative small distraction distance and lower distraction force than low frequency mode. In our study, the modified frequency of distraction produced satisfactory new bone consolidation in two groups.
The average duration of external fixator in group B was significantly lower than in group A, which allowed patients to achieve earlier rehabilitation and recovery. Meanwhile, it is presented that there were no statistical difference on external fixator index in two groups. The increasing duration of external fixator was just for guarantee the healing process in group A. Although there was no statistical difference regarding the functional outcomes of ASAMI scores between two groups, there were significant statistical differences in categories of PF, BP, and RE between two groups. The study of Mekhail et al. [2] showed that bone transport procedures mainly affect the physical and emotional status of the patients of post-traumatic bone defects. The general, mental, or social healths of patients were not usually affected. In our study, we think the early removal of external fixator gives patients benefit not only physical but emotional. Abandoning from the “ugly looking” of external fixator makes patients feel normal like others. Early rehabilitation activities give patients confidence to be a normal person. At present, more and more attention was paid on the biological–social status of patients during the treatment. The final results of treatment was not only a healing bone but also an active individual both physically and emotional.
Complications were presented in both groups of patients. In the group A, we had 11 cases of superficially pin tract infection and three cases of aseptic pin loosening. Residual knee stiffness was presented in six cases at the end of follow-up. There was none of pin loosening and residual knee stiffness in group B. Early removal of external fixator reduced the incidence of external fixator-related complications and allows better rehabilitation [25]. However, two amputations were performed in 15 patients in the group B compared with none in group A. There was chronic osteitis presented in these two patients. We believe that the risk of expanding an infection into intramedullary cavity increased with the insertion of the intramedullary nail. Furthermore, pin tract infections may spread more easily along intramedullary nail. We think bone defect with preoperative chronic osteitis should be treated with external fixator alone.
Beyond our expectation, there was no statistical significant difference regarding the total costs between two groups. Additional intramedullary nailing did not add the total cost of treatment compared with external fixator alone. We think the reason was that bone transport with the use of external fixator alone had a higher rate of complication, which adds a lot into the total cost of treatment. The major complication in group B was two cases of amputations, which added less in the total cost of treatment. We think, it is not necessary to take the intramedullary nailing cost into account when making the choice of two methods.
In conclusion, bone transport with the use of intramedullary nail reduced the incidence of complication due to the declined duration of external fixator time that gave patients a better life quality in both physical and emotional. Compared with using monolateral one alone, bone transport with the use of intramedullary nail received better results in bone healing. Moreover, additional use of intramedullary nail did not add a lot in the total cost of treatment. However, if chronic osteitis exists, bone transport should be treated with the use of monolateral external fixator alone due to a lower rate of amputations.
References
Sangkaew C (2005) Distraction osteogenesis for the treatment of post traumatic complications using a conventional external fixator: a novel technique. Injury 36:185–193
Mekhail AO, Abraham E, Gruber B, Gonzalez M (2004) Bone transport in the management of posttraumatic bone defects in the lower extremity. J Trauma 56(2):368–378
Caja V, Kim W, Larsson S, E YC (1995) Comparison of the mechanical performance of three types of external fixators: linear, circular and hybrid. Clin Biomech (Bristol, Avon) 10(8):401–406
Paley D, Herzenberg JE, Paremain G et al (1997) Femoral lengthening over an intramedullary nail: a matched-case comparison with Ilizarov femoral lengthening. J Bone Jt Surg Am 79(10):1464–1480
Paley D (1990) Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop 250:81–104
Paley D, Catagni MA, Argnani F et al (1989) Ilizarov treatment of tibial non-unions with bone loss. Clin Orthop 241:146–165
Zhang X, Liu T, Li Z, Peng W (2007) Reconstruction with callus distraction for nonunion with bone loss and leg shortening caused by suppurative osteomyelitis of the femur. J Bone Jt Surg Br 89B:1509–1514
Paley D, Herzenberg JE, Paremain G, Bhave A (1997) Femoral lengthening over an intramedullary nail: a matched-case comparison with Ilizarov femoral lengthening. J Bone Jt Surg Am 79A:1464–1480
Capanna J, Campanacci R, Belot DA et al (2007) A new reconstructive technique for intercalary defects of long bones: the association of massive allograft with vascularized fibular autograft. Long-term results and comparison with alternative techniques. Orthop Clin N Am 38:5–60
Lawal YZ, Garba ES, Ogirima MO et al (2011) Use of non-vascularized autologous fibula strut graft in the treatment of segmental bone loss. Ann Afr Med 10(1):25–28
Attias N, Lindsey RW (2006) Case reports: management of large segmental tibial defects using a cylindrical mesh cage. Clin Orthop Relat Res 450:259–266
Ilizarov GA (1990) Clinical application of the tension–stress effect for limb lengthening. Clin Orthop 250:8–26
Innocenti M, Delcroix L, Manfrini M et al (2004) Vascularized proximal fibular epiphyseal transfer for distal radial reconstruction. J Bone Jt Surg Am 86A(7):1504–1511
Tsuchiya H, Tomita K (2003) Distraction osteogenesis for treatment of bone loss in the lower extremity. J Orthop Sci 8:116–124
Green SA (1994) A comparison of bone grafting and bone transport for segmental skeletal defects. Clin Orthop Relat Res 301:111–117
Zhang X, Duan L, Li Z, Chen X (2007) Callus distraction for the treatment of acquired radial club-hand deformity after osteomyelitis. J Bone Jt Surg Br 89B:1515–1518
Liu T, Zhang X, Li Z et al (2008) Callus distraction for humeral nonunion with bone loss and limb shortening due to osteomyelitis. J Bone Jt Surg Br 90(6):795–800
Li Z, Zhang X, Duan L, Chen X (2009) Reconstruction with distraction osteogenesis technique over intramedullary nail combined with monolateral external fixator for massive postosteomyelitis skeletal defects of femur. Can J Surg 52(2):103–111
Raschke MJ, Mann JW, Oedekoven G, Claudi BF (1992) Segmental transport after unreamed intramedullary nailing. Preliminary report of a monorail system. Clin Orthop 282:233–240
Kristiansen LP, Steen H (1999) Lengthening of the tibia over an intramedullary nail, using the Ilizarov external fixator. Major complications and slow consolidation in nine lengthening. Acta Orthop Scand 70:271–274
Sun XT, Easwar TR, Stephen M et al (2011) Comparative study of callus progression in limb lengthening with or without intramedullary nail with reference to the pixel value ratio and the Ru Li’s classification. Arch Orthop Trauma Surg 131(10):1333–1340
Ilizarov G (1989) The tension–stress effect on the genesis and growth of tissues. Part II. The influence of the rate and frequency of distraction. Clin Orthop 239:263–285
Kessler P, Neukam FW, Wiltfang J (2005) Effects of distraction forces and frequency of distraction on bony regeneration. Br J Oral Maxillofac Surg 43:392–398
Isaksson H, Comas O, van Donkelaar CC et al (2007) Bone regeneration during distraction osteogenesis: mechano-regulation by shear strain and fluid velocity. J Biomech 40(9):2002–2011
Oh CW, Song HR, Roh JY et al (2008) Bone transport over an intramedullary nail for reconstruction of long bone defects in tibia. Arch Orthop Trauma Surg 128(8):801–808
Acknowledgments
We thank Miss Jing Wan for her editorial and secretarial assistance to this manuscript.
Conflict of interest
All authors declare no conflict of interest with this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Jun Wan and Lin Ling contribute equally to this manuscript.
Rights and permissions
About this article
Cite this article
Wan, J., Ling, L., Zhang, Xs. et al. Femoral bone transport by a monolateral external fixator with or without the use of intramedullary nail: a single-department retrospective study. Eur J Orthop Surg Traumatol 23, 457–464 (2013). https://doi.org/10.1007/s00590-012-1008-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-012-1008-x