Abstract
The Rapid Recovery Program (RRP) is an accelerated discharge programme aimed at reducing the length of stay (LOS) and improving patient satisfaction. Its principles are discussed, and our early experience of 847 hip and knee arthroplasty patients described. Three groups were identified: Pre-RRP implementation (Pre-RRP), Post-RRP implementation who did not attend our pre-operative educational Joint Replacement School (JRS) (RRP-JRS) and Post-RRP who did attend JRS (RRP + JRS). Mean LOS (days) for hip arthroplasty was 11 (Pre-RRP), 6.4 (RRP + JRS) and 8.7 (RRP-JRS) (P < 0.05). Mean LOS (days) for knee arthroplasty was 8.5 (Pre-RRP) (P < 0.05), 5.9 (RRP + JRS) and 5.8 (RRP-JRS). RRP reduced LOS and pre-operative education further reduced LOS in hip arthroplasty. We believe these effects are produced by streamlining perioperative processes, education and improving patient experience.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Accelerated discharge programmes for primary hip and knee arthroplasty are well documented [1–5]. They aim to reduce the length of hospital stay (LOS), improve patient satisfaction and save costs, whilst potentially reducing complications. These outcomes can be readily achieved by a change in the patient pathway from listing for surgery to outpatient discharge but require a significant change in practice. We present our experience of implementing the Rapid Recovery Program in a state run UK district general hospital, including some early results.
The Rapid Recovery Program (RRP) is a holistic perioperative accelerated discharge process aimed at improving efficiency and quality of care in hip and knee arthroplasty surgery. Its philosophy includes improving patient education and expectations, standardising protocols and pathways, and early mobilisation and rehabilitation. The RRP has been shown to decrease LOS [1, 6] and achieve higher range of knee motion and improved clinical and pain scores [6]. Importantly, no increase in complications has been shown [4]. No UK centre has yet reported results from such a programme for primary hip and knee arthroplasty.
The Rapid Recovery Program principles
The RRP philosophy is not new and has developed from the Joint Ventures programme which began the late 1980s in the USA [7]. Key principles (Table 1) underpin the RRP as an accelerated discharge programme, and these will be described with their evidence base. RRP values have more recently manifested under different titles, including Joint Recovery Program [8] Anorak-HH [3] and the Rapid Recovery Program [4].
Standardised protocols and pathways
Clinical care pathways are specified guidelines for care that describe patient treatment goals and define a sequence and timing of interventions to meet these goals efficiently [9]. In hip and knee arthroplasty, they have been shown to reduce costs and LOS, with no compromise in patient outcomes [10–12]. Once hospital personnel learn these pathways, a reduction in delays and errors can occur, promoting better, more efficient care.
Efficiency and quality management
With the development of care pathways, protocols and guidelines, with a robust audit loop, efficiency and quality can be maintained and improved. These help reduce care costs [8, 13, 14] and improve patient satisfaction [5, 13, 15] without increasing complication rates [1, 4, 9–11].
Patient education and expectation setting
A Cochrane review of pre-operative education for hip and knee arthroplasty, which analysed nine studies involving 782 patients [16], concluded that there was little evidence to support pre-operative education. Anxiety was shown to be reduced but pain, patient satisfaction, time to mobility milestones and LOS were not affected. However, the timing and methods of delivery varied considerably. Some authors sent a booklet by post [17], others showed participants a video after admission [18]. Three studies provided teaching sessions delivered by physiotherapists [19, 20] or nurses [19].
Pre-operative education must be timed appropriately before surgery and involve both the patient and the relative or friend. All members of the multidisciplinary team should deliver knowledge, which should be reinforced during admission. The RRP has a strong pre-operative educational component, presented to patients in a Joint Replacement School (JRS) and a detailed patient guide.
Patient expectations are important in recovery in arthroplasty surgery [21]. Patients fear the anaesthesia, the operation and post-operative pain and nausea [22]. During the JRS, the expectations of the patient are set by discussing a range of inpatient issues. The anaesthetic choices available, pain management, daily post-operative rehabilitation goals and the components of other treatments are explained. There is a strong reinforcement that they are not ill, despite being in hospital for treatment. Any reinforcers of the sickness role are removed e.g. changing into normal day clothes post-operatively rather than remaining in a hospital gown.
Patient as a care partner
The emphasis is placed on the patient to share the responsibility for his/her care. Patients are given the skills to help achieve this through pre-operative education. By taking part ownership of their treatment, patients can feel empowered, determined to recover more quickly and feel in greater control of their rehabilitation.
Early mobilisation and rehabilitation
Combining pre-operative education, specific anaesthetic and pain management protocols with a change in multidisciplinary mindset, patients can ambulate following total hip and knee arthroplasty, on the day of surgery. One important aspect in achieving this goal is pre-operative physiotherapy and rehabilitation education. This has been shown to reduce length of stay [23, 24], enabling patients to need less inpatient classes [25] and increasing patient satisfaction [26].
Personal coach
Patients are encouraged to nominate a partner, relative or friend to act as their support ‘Coach’. They play an important role in the rehabilitation process by preparing the patient prior to admission through encouragement, motivation and sharing concerns, preparing the home for the patient’s safe return (arranging furniture, cooking meals) and encouraging and supporting post-operative exercises. Coaches attend the JRS and inpatient exercise classes and encourage the patient throughout their journey even once after discharge.
Patient group dynamics
A further psychological facet RRP brings to the process is promoting group dynamics. Patients who attend JRS should all be inpatients at a similar time, forming a group which experience the entire pathway together. By creating a light hearted competitive atmosphere, patients can inspire and support one another. This can be facilitated by a ‘day area’ for group physiotherapy exercises, communal meals and socialising, promoting an enjoyable hospital experience and a social network after discharge.
Planned discharge
As part of pre-operative assessment, patients are assessed by occupational therapists and home modifications made well before discharge. At JRS, patients are advised that it is likely they will be discharged on the third post-operative day, and this is reinforced throughout the admission.
Implementing the Rapid Recovery Program in a UK hospital
Our institution is a 450-bed, state run, acute care hospital, serving a population of 350,000, located in greater London, United Kingdom. Four hundred and fifty hip and knee arthroplasties were performed in 2008, across two sites, by eight consultant surgeons (four dedicated to lower limb). Following Trust board approval, in May 2006, a steering committee was created. This comprised of representatives from each clinical team (Pre-Assessment Clinic Sister, Ward Sister, Physiotherapist, Occupational Therapist, Pharmacist, Surgeon, Anaesthetist, Pain Nurse), administration personnel and a senior hospital manager. The committee met initially weekly, then fortnightly.
Over the course of 1 year, the existing patient process was analysed and modifications made in accordance with RRP principles. New protocols and guidelines were agreed covering every aspect of the patient journey and resources developed to support the care pathway (Table 2). An outline of the new RRP patient experience is described.
Pre-admission clinic
Following the decision to operate in clinic, patients are assessed for their fitness for surgery that day, in a nurse led clinic. Pre-operative investigations are performed, and anaesthetic concerns are referred to a consultant anaesthetist for review on a different day.
Joint replacement school
Two to four weeks before admission, primary hip and knee arthroplasty patients of all American Society of Anesthesiologists (ASA) grades attend with their chosen Coach in classes of 12 patients for half a day. Non-attendance leads to their removal from the waiting list. Multimedia are used including posters, models, booklets and oral presentations by an anaesthetist, acute pain nurse, occupational therapist, physiotherapist, pharmacist and a ward nurse. The atmosphere is informal, and questions are encouraged. An emphasis is made that patients are not ill, despite being in hospital Pharmacist, occupational therapy and physiotherapy assessments are performed. Patients are recruited for research studies, and data collected for our database.
Admission
Admission is on the day of surgery to a dedicated short-stay ward. Patients are reviewed, marked and consented by the surgeon, and the anaesthetist finalises anaesthetic choices. Patients are walked to theatre with a nurse.
Physiotherapy
At JRS, the patients’ expected post-operative daily progress and their rehabilitation goals are explained. Exercises are demonstrated, and patients are encouraged to commence these pre-operatively. Individual sessions at JRS demonstrate the correct use of mobility aids and advice on stair climbing. Hip arthroplasty patients are given elbow crutches to take home and practise with. Post-operatively in the recovery room, exercises are commenced by the recovery nurse, which are active or passive if motor blockage remains. This demonstrates to the patient it is safe to mobilise their new joint. Patients are seen a few hours post-operatively, and exercises commenced, including walking, then daily, with the emphasis being placed upon the patient to exercise independently and regularly with support from their Coach. Laminated instructions demonstrating exercises are provided by the bedside and duplicated in the patient information booklet.
Occupational therapy
The Occupational Therapist identifies potential barriers to resuming normal daily activities post-operatively. A home assessment questionnaire is sent by post to patients, which is then brought to JRS. At JRS, a presentation is given on preparing their home for the post-operative period, e.g. cooking additional meals. Individual assessments allow detailed discussion of post-operative needs and the scope for their coach to support them. If a deficit of care is identified, a care package is implemented. Equipment is ordered and delivered prior to admission. On the day of admission, checks are made to ensure all equipment is in place.
Pharmacy
At JRS, a thorough drug history is made at individual assessments by a pharmacist. Drug cessation advice is given, e.g. warfarin, and all inpatient drugs transcribed onto the inpatient drug chart. Patients are requested to ensure they have sufficient medication at home for the post-operative period and to bring to hospital enough of their usual medication for their inpatient stay. Only pre-prepared analgesia packs dispensed from the ward are given to patients on discharge, avoiding pharmacy related discharge delays.
Anaesthesia
Patients are given comprehensive information about anaesthetic and pain relief choices in the patient education booklets and at JRS. Regional anaesthesia is promoted through JRS presentations, and an opportunity to ask questions is given. Acceptance of a regional technique is high with 75% (pre-RRP 36%) of hip and 87% (pre-RRP 45%) of knee arthroplasties performed under spinal or combined spinal and epidural anaesthesia. A typical regime of spinal anaesthesia with 2.75 mls 0.5% bupivacaine and 0.1-mg preservative free morphine with a target controlled propofol infusion for light sedation is used. A room separate to the operating room is used for anaesthetic administration. A periarticular infiltration of up to 60 mls of 0.25% Levobupivacaine (AstraZeneca, UK) is administered prior to implant placement.
Operative care
All patients enter a waiting list pool and are told their surgeon may be different from the clinician seen in clinic. The implant and surgical technique is at the discretion of the surgeon and involves either a posterior or lateral approach without a mini incision. Implant inventory is kept to a minimum which increases the scrub teams’ familiarity with instruments and enhances operative efficiency. All patients receive the peri-articular local anaesthetic injection unless contraindicated. Patients may use personal audio devices while in theatre to aid relaxation should they wish to be awake. Sedation is short acting, so exercises can be commenced in the recovery unit assisted by the recovery nurse. Once fully recovered, patients are returned to a dedicated elective ward.
Acute Pain Nurse (APN)
All patients are seen post-operatively by an APN. The aim is a pain score of less than 4/10 on movement. The JRS presentations inform patients of the aims for their pain management, and pain scoring, the analgesic ladder and multi-modal therapy are explained. A post-operatively RRP Pain Standard protocol was developed to standardise prescribing (Fig. 1). Patient controlled analgesia and opiates are avoided.
Ward nursing
If the physiotherapist is unavailable, patients are mobilised by the ward nursing staff. Laminated cards of expected daily care and rehabilitation progress are by the bedside for patients to read. A wound care protocol recommends that dressings are not disturbed until the day of discharge, unless heavily soiled. Senior nurses have discharge authority, and only pre-prepared analgesia packs are given as take-home medication. A telephone call by a ward sister is made to all patients 48 h after discharge, where designated questions (documented in patient notes) aid in detecting post-operative morbidity.
The early impact of the Rapid Recovery Program on length of stay
The RRP was implemented in our hospital on the October 2007. Our aim was to determine the impact of the RRP on length of stay (LOS). A cohort of patients did not attend JRS, which enabled the comparison of patients experiencing RRP without pre-operative education, with those that did. Our hypothesis was that the RRP would reduce LOS significantly and that pre-operative education would reduce LOS compared with those who were not pre-operative educated.
Patients and methods
A retrospective cohort study of all patients admitted for primary hip and knee arthroplasty (of any type) was performed between May 2007 and February 2009. A total of 847 patients (mean age 71 years (27–98), 67% women) comprising of 447 knee and 400 hip arthroplasties were included in this study. Three cohorts were identified: Patients who had surgery before the RRP was implemented (Pre-RRP), patients who did not attend JRS but experienced the RRP (RRP-JRS) and patients who did attend JRS and experienced the RRP (RRP + JRS). The impact on LOS made by the RRP (Pre-RRP vs. RRP + JRS) and pre-operative education (at JRS) (RRP-JRS vs. RRP + JRS) was analysed.
Statistical analysis
LOS data were tested for normality using the Kolmogorov–Smirnov test and fitted the assumptions made for parametric testing. The mean LOS between cohorts was compared using Welch’s t test (assuming unequal variances) with P < 0.05 considered significant. Data were also examined for the number of patients staying 3 days or less and more than 5 days and the groups analysed using the chi square test. Analysis was performed with Excel (version 2007, Microsoft, USA) and Simple Interactive Statistical Analysis (www.quantitativeskills.com/sisa). ‘Day 0’ was defined as the day of operation; ‘Day 1’ as the first post-operative day and ‘Discharge’ defined as discharge to the patients’ home.
Results
The demographics of the three cohorts are presented in Table 3 and were similar. The mean LOS comparisons of the groups are shown in Table 4.
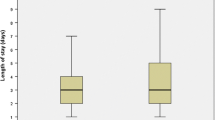
Rapid Recovery Program impact on length of stay
Comparing LOS of patients before RRP was implemented (Pre-RRP) with those patients who experienced RRP with JRS (RRP + JRS), the mean LOS for both hips and knees was reduced from 9.6 days (SD 8.1, range 1–56) to 6.3 days (SD 5.8, range 1–38) (P < 0.01) (Table 4). For hip arthroplasty, mean LOS was reduced from 11 days (SD 8.5, range 1–44) Pre-RRP to 6.4 days (SD 6.6, range 1–24) post-RRP (P < 0.01). For knee arthroplasty, mean LOS was reduced from 8.5 days (SD 7.5, range 2–56) Pre-RRP to 5.9 days (SD 5.1, range 2–38) post-RRP (P < 0.01).
The RRP had an impact on the percentage of patients discharged on day 3 or earlier and after day 5. For hip arthroplasty, more patients were discharged on day 3 (Pre-RRP 3% vs. RRP + JRS 24%; P < 0.001) and less patients stayed more than 5 days (Pre-RRP 75% vs. RRP + JRS RRP 41%; P < 0.001). For knee arthroplasty, more patients were discharged on day 3 (Pre-RRP 9% vs. RRP + JRS 30%; P < 0.001) and less patients stayed more than 5 days (Pre-RRP 60% vs. RRP + JRS 34%; P < 0.001).
Pre-operative education impact on length of stay
The mean LOS comparison of patients who attended JRS (RRP + JRS) with those who did not attend JRS but still experienced RRP (RRP-JRS) is presented in Table 4. This analysis allows the assessment of the impact of pre-operative education on LOS. For hip arthroplasty, the mean LOS was reduced from 8.7 days (SD 7.7, range 1–42) (RRP-JRS) to 6.4 days (SD 6.6, range 1–24) (RRP + JRS) (P < 0.05). For knee arthroplasty, the mean LOS was 5.8 days (SD 3.9, range 2–26) (RRP-JRS) and 5.9 days (SD 5.1, range 2–38) (RRP + JRS) (P > 0.05).
Pre-operative education had an impact on the percentage of patients discharged on day 3 or earlier and after day 5. For hip arthroplasty, no difference was found in the number of patients discharged on day 3 (21% RRP-JRS vs. 14% RRP + JRS (P > 0.05). However, less patients were discharged after day 5 (56% RRP-JRS vs. 41% RRP + JRS (P < 0.05). For knee arthroplasty, no difference was found in the number of patients discharged on day 3 or earlier (28% RRP-JRS vs. 30% RRP + JRS (P > 0.05) nor in the number of patients discharged after day 5 (33% RRP-JRS vs. 34% RRP + JRS (P > 0.05).
Discussion
The Rapid Recovery Program is a holistic approach to the arthroplasty patient care pathway, aimed at increasing efficiency, streamlining care and improving the patient experience. It benefits all groups involved in the process, in particular, the patient. By focusing care around the patient and using comprehensive pre-operative education with reinforcement that they are not ill, this can empower patients to take ownership of their care and improve motivation, essential for rapid discharge.
One indicator of RRP success was a reduced length of stay. The mean LOS in hip arthroplasty patients was reduced by 4.6 days (P < 0.001), a reduction of 40%, following implementation. For knee arthroplasty, the mean LOS reduction was 2.6 days (P < 0.001), a reduction of 30%. The number of hip and knee arthroplasty patients going home by day 3 increased (P < 0.001) and the number of patients staying longer than 5 days reduced (P < 0.001) compared with previously care in our Trust.
There are many reasons why a reduced LOS was achieved with this initiative. A large impact was the cultural change within the hospital. By creating an implementation team being fully inclusive of clinical and non-clinical staff, a focused drive to achieve high standards and early discharge was met in a coordinated fashion. Awareness that mobilisation on the day of surgery was safe and a new care pathway, clearly stating daily goals also contributed.
The greater reduction in hip compared with knee arthroplasty LOS may be related to the cultural change of staff. The fear of causing a hip dislocation is a specific concern related to post-operatively rehabilitation, whereas knee arthroplasty has no such risks. Through staff education, it was reinforced that it was safe to move the hip joint in recovery and mobilise the patient on the operative day without risking dislocation (so long as specific hip precautions were adhered to). This cultural change accelerated mobilisation rates and therefore reduced LOS.
Another important factor in reducing LOS was pre-operative education at the Joint Replacement School. We have shown our pre-operative education reduced LOS in hip arthroplasty by a mean of 2.3 days (P < 0.05). We believe this was achieved by reducing anxiety through education and reinforcing a 3 day in patient stay. However, other non-educational processes occurred at our JRS, including occupational therapy assessments. These allowed home modifications to be made well before discharge, preventing a delay in returning home. It is therefore not clear which part of our JRS had an impact on LOS. The JRS did not reduce LOS in knee arthroplasty patients however. This may be due the bigger impact of pre-operative physiotherapy (e.g. crutch training) on hip arthroplasty patients than the already more pre-operatively mobile, knee arthroplasty patients. Post-operatively, more home modifications are made for hip arthroplasty than for knee arthroplasty patients, potentially preventing discharge. The impact therefore of the JRS occupational therapy assessments on LOS was less for knee arthroplasty patients.
Despite no LOS effect in knee arthroplasty, we believe the JRS and its educational component, had a positive effect on patients, their coaches and hospital staff. By reducing patient anxiety, clearly defining daily post-operative goals and creating a friendly and positive atmosphere, patients were much better prepared for their surgery and post-operative period than previously. We strongly believe all arthroplasty patients should have access to a service of this kind.
Many benefits can be realised through processes like the Rapid Recovery Program. A change in hospital culture regarding the care of arthroplasty patients is possible if implemented in an inclusive and well-organised manner. By creating a team with common goals relating to improving patient care, staff motivation and morale can be lifted, especially when those involved see results. As bed days are saved with early discharge and efficiency and throughput increases, cost benefits can be realised, easily outweighing the set up costs of the initiative.
The RRP is a patient-centred programme which radically changes the arthroplasty experience compared with traditional methods. Through comprehensive education, patients take more ownership of their care, anxiety can be reduced, and more informed treatment decisions can be made. By streamlining care processes and creating an enjoyable experience, patients can be more satisfied. Hospital staff can work within more predictable standardised pathways, which reduces stress and increases in efficiency.
To successfully implement an initiative of this type requires a well-motivated multidisciplinary approach, with willingness of both clinical and non-clinical parties to change. We have demonstrated it is possible to implement far-reaching change which has a positive impact on patient care, within a state run healthcare system. However, an infrastructure conducive to process re-engineering, a well-motivated multidisciplinary team and support from hospital managers as well as industry, is essential. We recommend a Rapid Recovery Program to promote early discharge; however, further evaluation of patient outcomes such as complication rates must be considered.
References
Berend KR, Lombardi AV Jr, Mallory TH (2004) Rapid recovery protocol for peri-operative care of total hip and total knee arthroplasty patients. Surg Technol Int 13:239–247
Isaac D, Falode T, Liu P, I’Anson H, Dillow K, Gill P (2005) Accelerated rehabilitation after total knee replacement. Knee 12:346–350
Husted H, Holm G (2006) Fast track in total hip and knee arthroplasty—experiences from Hvidovre University Hospital, Denmark. Injury 37 Suppl 5:S31–S35
Pilot P, Bogie R, Draijer WF, Verburg AD, van Os JJ, Kuipers H (2006) Experience in the first four years of rapid recovery; is it safe? Injury 37(Suppl 5):S37–S40
Husted H, Holm G, Jacobsen S (2008) Predictors of length of stay and patient satisfaction after hip and knee replacement surgery: fast-track experience in 712 patients. Acta Orthop 79:168–173
Lombardi AV Jr, Viacava AJ, Berend KR (2006) Rapid recovery protocols and minimally invasive surgery help achieve high knee flexion. Clin Orthop Relat Res 452:117–122
Steele MK III, McLean MB, Gaunt R, Browning WA (2000) The joint ventures program: improving outcomes and satisfaction in joint surgery patients. J Clin Outcomes Manage 7:28–30
Brunenberg DE, van Steyn MJ, Sluimer JC, Bekebrede LL, Bulstra SK, Joore MA (2005) Joint recovery programme versus usual care: an economic evaluation of a clinical pathway for joint replacement surgery. Med Care 43:1018–1026
Pearson S, Moraw I, Maddern GJ (2000) Clinical pathway management of total knee arthroplasty: a retrospective comparative study. Aust N Z J Surg 70:351–354
Dowsey MM, Kilgour ML, Santamaria NM, Choong PF (1999) Clinical pathways in hip and knee arthroplasty: a prospective randomised controlled study. Med J Aust 170:59–62
Kim S, Losina E, Solomon DH, Wright J, Katz JN (2003) Effectiveness of clinical pathways for total knee and total hip arthroplasty: literature review. J Arthroplasty 18:69–74
Vanhaecht K, Sermeus W, Tuerlinckx G, Witters I, Vandenneucker H, Bellemans J (2005) Development of a clinical pathway for total knee arthroplasty and the effect on length of stay and in-hospital functional outcome. Acta Orthop Belg 71:439–444
Healy WL, Iorio R, Ko J, Appleby D, Lemos DW (2002) Impact of cost reduction programs on short-term patient outcome and hospital cost of total knee arthroplasty. J Bone Joint Surg Am 84-A:348–353
Scranton PE Jr (1999) The cost effectiveness of streamlined care pathways and product standardization in total knee arthroplasty. J Arthroplasty 14:182–186
Reilly KA, Beard DJ, Barker KL, Dodd CA, Price AJ, Murray DW (2005) Efficacy of an accelerated recovery protocol for Oxford unicompartmental knee arthroplasty—a randomised controlled trial. Knee 12:351–357
McDonald S, Hetrick S, Green S (2004) Pre-operative education for hip or knee replacement. Cochrane Database Syst RevCD003526
Butler GS, Hurley CA, Buchanan KL, Smith-VanHorne J (1996) Prehospital education: effectiveness with total hip replacement surgery patients. Patient Educ Couns 29:189–197
Daltroy LH, Morlino CI, Eaton HM, Poss R, Liang MH (1998) Preoperative education for total hip and knee replacement patients. Arthritis Care Res 11:469–478
Cooil J, Bithell C (1997) Pre-operative education for patients undergoing total hip replacement: a comparison of two methods. Physiother Theory Pract 13:163
Wijgman AJ, Dekkers GH, Waltje E, Krekels T, Arens HJ (1994) No positive effect of preoperative exercise therapy and teaching in patients to be subjected to hip arthroplasty. Ned Tijdschr Geneeskd 138:949–952
Liang MH, Katz JN, Phillips C, Sledge C, Cats-Baril W (1991) The total hip arthroplasty outcome evaluation form of the American Academy of Orthopaedic Surgeons. Results of a nominal group process. The American Academy of Orthopaedic Surgeons Task Force on Outcome Studies. J Bone Joint Surg Am 73:639–646
Mitchell M (2003) Patient anxiety and modern elective surgery: a literature review. J Clin Nurs 12:806–815
Crowe J, Henderson J (2003) Pre-arthroplasty rehabilitation is effective in reducing hospital stay. Can J Occup Ther 70:88–96
Coudeyre E, Jardin C, Givron P, Ribinik P, Revel M, Rannou F (2007) Could preoperative rehabilitation modify postoperative outcomes after total hip and knee arthroplasty? Elaboration of French clinical practice guidelines. Ann Readapt Med Phys 50:189–197
Vukomanovic A, Popovic Z, Durovic A, Krstic L (2008) The effects of short-term preoperative physical therapy and education on early functional recovery of patients younger than 70 undergoing total hip arthroplasty. Vojnosanit Pregl 65:291–297
McGregor AH, Rylands H, Owen A, Dore CJ, Hughes SP (2004) Does preoperative hip rehabilitation advice improve recovery and patient satisfaction? J Arthroplasty 19:464–468
Acknowledgments
The authors would like to thank the Rapid Recovery Team for their work in the implementation of the project and specifically Sheridan Hanson, Teresa Box and Sheridan Methuen.
Conflict of interest
No funds were received in support of this study. No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gordon, D., Malhas, A., Goubran, A. et al. Implementing the Rapid Recovery Program in primary hip and knee arthroplasty in a UK state run hospital. Eur J Orthop Surg Traumatol 21, 151–158 (2011). https://doi.org/10.1007/s00590-010-0690-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-010-0690-9