Abstract
Introduction
Tranexamic acid is an inhibitor of fibrinolysis and thereby decreases blood loss in patients undergoing surgery.
Materials and methods
Fifty patients were randomized to Tranexamic acid (15 mg/kg) given as a bolus intravenous injection or placebo (normal saline) given intravenously, 15 min before the incision. The intraoperative and postoperative blood loss and the number of blood transfusions required were recorded. The patients were screened for deep venous thrombosis with bilateral compression ultrasonography on the 10th postoperative day. The hemoglobin level was measured preoperatively and on the 3rd postoperative day. The D-dimer levels were measured preoperatively and 24-h postoperatively.
Results
Patients receiving Tranexamic acid had a mean intraoperative blood loss of 410 ml (range, 300–510 ml) vs. 615 ml (range, 515–750 ml) (P value < 0.05) in patients receiving placebo, a postoperative blood loss of 210 ml (range, 150–325 ml) vs. 490 ml (range, 370–540 ml) (P value < 0.05), and a total need for 8 blood transfusions versus 30. 6/25 patients in first group and 18/25 patients in the placebo group required transfusion. In placebo group, the mean fall in hemoglobin was 2.9 g/dl (range, 2.5–3.2) when compared to 1.6 g/dl (1.3–2) (P < 0.05) in the Tranexamic group. At 24-h postoperatively, mean plasma D-dimer concentration in the Tranexamic group was half of that in the control group. No patient in either group had any evidence of deep vein thrombosis.
Conclusion
Tranexamic acid given as a single preoperative bolus dose reduces intraoperative and postoperative and total blood loss and transfusion requirements in primary cementless total hip replacement surgery without any increased risk of thrombus formation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Several techniques like autologous blood transfusion, intraoperative blood saving, freezing saline, hypotensive anesthesia have been developed to decrease the surgical bleeding and perioperative allogenic blood transfusion requirement [1]. This requirement for blood transfusion carries with it the risk of well-recognized complications, including transfusion reactions and transmission of infectious agents.
Tranexamic acid is a synthetic antifibrinolytic drug used to prevent bleeding. It acts by blocking the lysine-binding site of plasminogen to fibrin. It also inhibits the activation of plasminogen by plasminogen activator [2].
We conducted a prospective, randomized, double-blinded study on 50 patients undergoing primary cementless total hip arthroplasty to determine the effect of ‘Tranexamic acid’ on intraoperative and postoperative blood losses and on the transfusion requirements.
Materials and methods
Fifty patients undergoing unilateral, cementless total hip arthroplasty were investigated in a prospective, randomized, double-blinded study. Patients with a history of severe ischemic heart disease, chronic renal failure, cirrhosis of the liver, and bleeding disorders, as well as those who were currently receiving anticoagulant therapy, were excluded from this study. The local hospital ethics committee approved the present study, and informed consent was obtained from each patient.
A cementless total hip system, Versys Trilogy (Zimmer, Warsaw, USA) was used in all patients. Spinal anesthesia followed by epidural analgesia until the next morning was used in all patients. The same surgeon (R.M.) performed all arthroplasties through a standard posterior approach with the patient in a lateral position. The posterior capsule was closed, and a closed suction drain was placed under the gluteal muscle. The same antithrombotic prophylaxis during hospitalization, low-molecular-weight heparin, and elastic leg dressing were used for all patients. Antibiotic prophylaxis was discontinued on the day after surgery.
Twenty-five patients received a bolus intravenous dose (15 mg/kg) of Tranexamic acid, 15 min before the incision. Other 25 patients received a corresponding dose of placebo (normal saline) intravenously. The basic characteristics of the patients did not differ between the groups (Table 1).
The primary outcome variables were blood loss during the operation and the amount of drainage after the operation. We determined the intraoperative blood loss by adding the measured suction volumes and changes in the weight of the used surgical sponges. Postoperative blood loss was measured at removal of drain, 24 h after the operation.
Secondary variables were the amount of transfused units of red cells, drop in hemoglobin levels, rise in D-dimers value, and possible complications. The blood transfusions were given in a standardized way. Hemoglobin (starting level) was measured on the day of surgery, in the recovery ward, and on the third postoperative day. The lowest value was used for the comparison. If a patient had a reduction in hemoglobin exceeding 25% of the starting level and had clinical symptoms, a blood transfusion(s) was given. We recorded the number of transfusions given on the recovery ward (until 6 h after surgery) and/or on the ward. No transfusions were administered after the second postoperative day. The D-dimer levels were measured preoperatively on the day of admission and 24-h postoperatively. Ultrasonic screening for deep vein thrombosis (DVT) in both legs was blinded and was performed for all patients on Day 10 postoperatively. All wounds were inspected on the third postoperative day and at discharge, and any signs of prolonged drainage or infection were noted.
Statistical analysis
Student t-test and the chi-squared test were used to analyze the data. A P value ≤ 0.05 was considered to be statistically significant. The analyses were made using SPSS statistical package (version 10.0).
Results
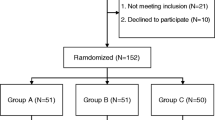
No significant differences between the groups were found in the demographic data (Table 1). Patients (Fig. 1) in Tranexamic acid group had a mean intraoperative blood loss of 410 ml (range, 300–510 ml.), which was significantly less (P value = <0.5) when compared to placebo group, 615 ml (range, 515–750 ml). Mean postoperative blood loss was also significantly less (P value = <0.5) in Tranexamic acid group, 210 ml (range, 150–325 ml) when compared to placebo group, 490 ml (range 370–540 ml.) (Fig. 2).
Six patients in Tranexamic acid group needed a total of 8 units of allogenic blood transfusion, while 18 patients in placebo group needed a total of 30 units of allogenic blood transfusion. The mean preoperative hemoglobin level was 10.58 g/dl (9.3–14) in Tranexamic acid group, while in placebo group mean preoperative hemoglobin level was 10.5 g/dl (9.2–14.2). Mean postoperative hemoglobin level was 8.98 g/dl (7.4–12.7) in Tranexamic acid group when compared to 7.6 g/dl (6.2–11) in placebo group. In placebo group, the mean fall in hemoglobin was 2.9 g/dl (range, 2.5–3.2) when compared to 1.6 g/dl (range, 1.3–2) in the Tranexamic acid group. This was found to be statistically significant. (P value = <0.5).
At 24-h postoperatively, mean plasma D-dimer concentration in the Tranexamic acid group was half of that of in the control group. No patient in either group had any evidence of deep vein thrombosis on bilateral compression ultrasonography using Colour Doppler imaging done on 10th postoperative day. No patient in any group had prolonged drainage, infection, clinical deep venous thrombosis or pulmonary embolism during hospitalization or at follow-up. We found no untoward reactions to Tranexamic acid.
Discussion
Total hip arthroplasty is associated with a significant amount of blood loss often requiring allogenic blood transfusions. In an attempt to reduce bleeding and the need for allogenic blood transfusion, antifibrinolytic drugs, such as Tranexamic acid, have been administered [3–5].
Tranexamic acid has been used in both total hip and knee arthroplasty with encouraging results. Several studies have investigated the result of Tranexamic acid administration on intraoperative and postoperative blood loss in patients undergoing cemented total hip arthroplasty [4, 6, 7], but few studies are available for cementless total hip arthroplasty [1, 5]. Postoperative blood loss tends to be higher in association with cementless total hip arthroplasty than in association with cemented total hip arthroplasty [5, 8].
In contrast to the study by Benoni et al. [6], who used late intraoperative Tranexamic acid administration and found no effect on postoperative blood loss, we estimated less bleeding with preincisional Tranexamic acid in our patients. There was significant reduction in both intraoperative and postoperative bleeding in Tranexamic acid group. This difference can be explained by the fact that Tranexamic acid inhibits fibrinolysis mainly by blocking the lysine-binding sites of plasminogen, the same sites, which plasminogen uses for its binding to fibrin. On the fibrin surface, plasminogen is activated to plasmin and starts to degrade the fibrin molecules [9]. To be effective, Tranexamic acid probably has to interact with the plasminogen-binding site before binding to fibrin occurs. In hip arthroplasty, fibrin plug formation occurs during the operation while blood vessels are severed, leaving ample time for plasminogen binding if Tranexamic acid is not present initially. If Tranexamic acid is given later, the drug is probably much less likely to affect the fibrinolytic process, since the plasminogen is already bound to fibrin [10]. Our results also showed the reduction in number of patients requiring transfusion as well as in number of units transfused. There was also significantly less mean hemoglobin drop in Tranexamic acid group.
Currently, Tranexamic acid is given as a single bolus and/or a bolus and constant infusion with the infusion stopping at the conclusion of surgery, although there are no set guidelines on the amount of the boluses for the agents or duration of the infusion [11]. The half-life of intravenously administered Tranexamic acid has been found to be 1.9 h [12]. As we have discussed, fibrin plug formation occurs only during the operation while blood vessels are severed and mean surgical time is quite less than the half-life of Tranexamic acid, we recommend only a single bolus dose of Tranexamic acid and this was found to reduce both intraoperative and postoperative blood loss.
A theoretical concern associated with the use of Tranexamic acid is its potential for inducing thromboembolic events [13–15]. The use of Tranexamic acid in hip arthroplasty does not appear to increase thrombosis. We had no thromboembolic complications as we also confirmed it by compression ultrasonography. Also, the D-dimer levels were similar in both groups.
In conclusion, the present study demonstrated that the administration of single intravenous dose of Tranexamic acid (15 mg/kg) just before surgery significantly reduces intraoperative as well as postoperative blood loss in patients undergoing primary cementless total hip arthroplasty, without increasing any risk of thromboembolic events.
References
Yamasaki S, Masuhara K, Fuji T (2004) Tranexamic acid reduces blood loss after cementless total hip arthroplasty—prospective randomized study in 40 cases. Int Orthop 28:69–73
Garneti N, Field J (2004) Bone bleeding during total hip arthroplasty after administration of tranexamic acid. J Arthroplasty 4:19
Ido K, Neo M, Asada Y, Kondo K, Morita T, Sakamoto T, Hayashi R, Kuriyama S (2000) Reduction of blood loss using tranexamic acid in total knee and hip arthroplasties. Arch Orthop Trauma Surg 120:518–520
Benoni G, Fredin H, Knebel R, Nilsson P (2001) Blood conservation with Tranexamic acid in total hip arthroplasty: a randomized, double-blind study in 40 primary operations. Acta Orthop Scand 72:442–448
Yamasaki S, Masuhara K, Fuji T (2005) Tranexamic acid reduces postoperative blood loss in cementless total hip arthroplasty. J Bone Joint Surg Am 87:766–770
Benoni G, Lethagen S, Nilsson P, Fredin H (2000) Tranexamic acid, given at the end of the operation, does not reduce postoperative blood loss in hip arthroplasty. Acta Orthop Scand 71:250–254
Ekbäck G, Axelsson K, Ryttberg L, Edlund B, Kjellberg J, Weckström J, Carlsson O, Schött U (2000) Tranexamic acid reduces blood loss in total hip replacement surgery. Anesth Analg 91:1124–1130
Clarke AM, Dorman T, Bell MJ (1992) Blood loss and transfusion requirements in total joint arthroplasty. Ann R Coll Surg Engl 74:360–363
Nilsson IM (1980) Clinical pharmacology of aminocaproic and tranexamic acids. J Clin Pathol (R Coll Pathol) Suppl 14: 41–7
Benoni G, Fredin H, Knebel R et al (2001) Blood conservation with tranexamic acid in total hip arthroplasty: a randomized, double-blind study in 40 primary operations. Acta Orthop Scand 72:5
Gill BJ, Rosenstein A (2006) The use of antifibrinolytic agents in total hip arthroplasty: a meta-analysis. J Arthroplasty 6:869–873
Sano M, Hakusui H, Kojima C, Akimoto T (1976) Absorption and excretion of Tranexamic following intravenous intramuscular and oral administrations in healthy volunteers. Clin Pharmacol Ther 7:375–382
Lindoff C, Rybo G, Astedt B (1993) Treatment with tranexamic acid during pregnancy, and the risk of thrombo-embolic complications. Thromb Haemost 70:238–240
Tanaka N, Sakahashi H, Sato E, Hirose K, Ishima T, Ishii S (2001) Timing of the administration of tranexamic acid for maximum reduction in blood loss in arthroplasty of the knee. J Bone Joint Surg Br 5:702–705
Ho KM, Ismail H (2003) Use of intravenous tranexamic acid to reduce allogeneic blood transfusion in total hip and knee arthroplasty: a meta-analysis. Anaesth Intensive Care 31:529–537
Acknowledgments
No funds were received in support of this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Malhotra, R., Kumar, V. & Garg, B. The use of tranexamic acid to reduce blood loss in primary cementless total hip arthroplasty. Eur J Orthop Surg Traumatol 21, 101–104 (2011). https://doi.org/10.1007/s00590-010-0671-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-010-0671-z