Abstract
Purpose
To define the relationship between 3D radiological features, psychological factors, and back pain prevalence and intensity in patients with adolescent idiopathic scoliosis (AIS).
Methods
Consecutive AIS patients answered self-reported questionnaires and underwent simultaneous posterior–anterior and lateral scans of the spine (EOS Imaging, Paris, France). 3D reconstructions of the spine and pelvis reported 18 parameters in the coronal, sagittal, and axial plane.
Results
Hundred and twenty-four patients with AIS were included in the study. Overall, 90% of AIS patients reported having some back pain over the last 6 months and 85.8% over the last 30 days. Pain intensity in the last month was reported to be mild in 37.5%, moderate in 31.8%, moderate to severe in 24.3%, and severe in 6.54% of cases. Location of back pain was associated with location of main curve (P = 0.036). Low back pain was associated with higher lumbar apical AVR and lower lumbar lordosis (P < 0.05). Independent risk factors for back pain in AIS were pain catastrophizing (B = 0.061, P = 0.035), poorer self-reported state of mental health (B = − 0.872, P = 0.023), decreased thoracic kyphosis (B = − 0.033, P = 0.044) and greater pelvic asymmetry (B = 0.146, P = 0.047). There was a significant association between self-reported pain intensity in the last 24 h and levels of catastrophizing. Pain catastrophizing level influenced the relationship between deformity severity and pain intensity. In low catastrophizers, there was a significant association between greater deformity severity and higher pain levels.
Conclusions
Back pain in AIS is multifactorial and associated with psychological and morphological parameters. Pain catastrophizing is an important construct in AIS-related pain and should be taken into consideration when evaluating these patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Back pain is a common complaint in patients with adolescent idiopathic scoliosis (AIS). We recently identified that a relatively high proportion of AIS patients with chronic back pain have functional disability, sleep disorders, and reduced quality of life [1]. However, pain is frequently underestimated by surgeons who treat these patients [2]. Indeed, AIS was considered to be a painless condition until a few decades ago [3]. Main reasons for skepticism towards an association between pain and deformity include the current controversy in the literature on the link between deformity severity and pain intensity [4,5,6,7,8], and the more convincing statistical association between other psychological variables (i.e., self-image or mental health state) and pain [2, 9]. In fact, it is common that patients with small curves present with intense pain and vice-versa, suggesting that morphology is not the only explanation for the association.
Despite the evolvement of pain research in recent years with demonstration of advanced cartilage deterioration in AIS as seen in osteoarthritis [10], and the evidence of impaired endogenous pain modulation in around 50% of AIS patients with chronic back pain [1], there is a lack of comprehensive data investigating the contribution of morphological and psychological factors for back pain in this population. For example, although recognized as a three-dimensional deformity, there are no studies investigating the relationship between vertebral axial rotation and pain in this population. In adults with scoliosis, vertebral axial rotation is significantly associated with pain [11, 12]. In AIS, there is growing evidence suggesting that similar curve types can have different axial plane patterns [13], and the axial plane pattern may predict outcomes of AIS [14].
Moreover, there is a lack of studies investigating the role of psychological and behavioral processes between pain and AIS. For example, the use of specific self-reported instruments to measure mood and pain catastrophizing has not been reported. Pain catastrophizing is defined as an exaggerated negative mindset toward actual or anticipated pain, characterized by magnification, rumination, and helplessness [15]. Pain catastrophizing is a strong predictor of self-reported pain intensity and disability in adults [16] and children [17,18,19,20,21]. In fact, there is evidence suggesting that pain catastrophizing in children is a significant predictor of persistent pain and central sensitization in adulthood [18, 22]. To date, there is no study assessing the effect of pain catastrophizing on pain in these patients.
In order to better understand the relationship between the morphological aspects of AIS and back pain, we designed a pain study incorporating three-dimensional radiological assessment and comprehensive psychological measures related to pain processing. We hypothesized that back pain reported by AIS patients is related to morphological factors, as well as psychological parameters.
Methods
A cross-sectional study was designed and comprised of 124 consecutive AIS patients aged between 10 and 21 years old prior to elective spinal surgery at the Shriners Hospitals for Children—Canada. Pain was not a primary indication for scoliosis surgery. Patients were approached by a research assistant during the preoperative consultation and prospectively enrolled in the study after signing an informed consent. Exclusion criteria were inability to speak English or French, a diagnosis of developmental delay that would interfere with completing the questionnaires (e.g., mental development delay), and previous spine surgery. A research assistant collected information on demographics, medical history, and self-reported questionnaires for each enrolled patient 7 to 10 days before surgery.
Ethics approval was obtained prior to the beginning of the recruitment from the Research Ethics Board of our Institution (A08-M71-17B).
Self-reported measures
Self-reported pain intensity in the last 24 h was assessed using the Numerical Rating Scale (NRS 0–10), where 0 indicated no pain and 10 indicated the worst pain imaginable. Patients were asked to give the worst pain (NRS-worst pain), average pain (NRS-average pain), and best pain (NRS-best pain) in the last 24 h. The NRS has been validated in the pediatric population and is recommended for use in clinical research [23, 24]. The location of pain was reported in a body outline diagram of the back divided into several segments completed by the patient [1].
The preoperative questions of the Scoliosis Research Society—30 (SRS30) were used to evaluate health-related quality of life [25]. The questionnaire is composed of 5 domains as follows: function/activity (SRS30 function), pain (SRS30 pain), self-image/appearance (SRS30 self-image), mental health (SRS30 mental health), and satisfaction with management (SRS30 satisfaction). Each domain is graded from 1 (worst) to 5 (best).
The Pain catastrophizing scale for children (PCS-C) evaluates rumination, magnification, and helplessness dimensions of pain catastrophizing [20, 26]. Based on levels of functional disability, depression and anxiety, different clinical reference points for PCS-C have been suggested: low catastrophizing, score between 0 and 4; moderate catastrophizing, score between 15 and 25; and high catastrophizing, score ≥ 26 [27].
The State and Trait Anxiety Inventory for children (STAI-c) was used to assess anxiety [28, 29]. This inventory is composed of 2 subscales: State Anxiety Scale (20 items), which evaluates the current state of anxiety, measuring subjective feelings of apprehension, tension, nervousness, worry, and activation/arousal of the autonomic nervous system; and the Trait Anxiety Scale (20 items), which assesses anxiety proneness, including general states of calmness, confidence, and security [30].
Radiological assessment
Each participant underwent simultaneous posterior–anterior and lateral scans of the spine, including cervical spine and femoral heads in standing position in the EOS apparatus (EOS Imaging, Paris, France). Stereoradiographs were performed in a standard protocol which included free-standing position with horizontal gaze, with their hands lifted and placed flat on the wall at chest height in order to clear the thoracic spine adequately. 3D reconstructions of the spine and pelvis were performed by experienced professionals trained at the EOS Imaging (Montreal, Canada) using SterEOS software version 1.6.4.7977 (EOS Imaging) and not involved with patient’s care or administration of questionnaires. All parameters were expressed in the patient’s reference plane based on a vertical plane passing through the center of the acetabulum, in order to correct the effects of a potential axial rotation of the pelvis during image acquisition [31].
From the 3D reconstructions, 18 parameters were assessed in the coronal, sagittal, and axial plane. From the coronal plane the following variables were extracted: Cobb angle of the proximal thoracic, main thoracic and thoracolumbar/lumbar, as well as the major Cobb angle (defined as the largest measure), thoracic apical translation, lumbar apical translation, pelvic asymmetry (i.e., functional leg length discrepancy [LLD], measured as the difference between both height of the femoral heads in mm) [32], and coronal balance (defined as the difference between the thoracic and lumbar apical translations). From the sagittal plane, we extracted sagittal vertical axis (SVA), T1-T12 kyphosis, L1-S1 lordosis, pelvic incidence (PI), sacral slope (SS), and pelvic tilt (PT). Axial plane parameters included the apical vertebral axial rotation (AVR), and the axial intervertebral rotation (AIR) of the upper and lower levels of the main curve, defined as the absolute sum of intervertebral rotations from the upper neutral vertebra to the apical vertebra, and from the apical vertebra to the lower neutral vertebra, respectively [33]. We also evaluated the torsion index of the main curve, defined as the absolute sum of the axial intervertebral rotation of the curve [33, 34]. SterEOS 3D software is currently the most precise and accurate method for measurement of vertebral axial rotation with an error of 2.4° on average [35]. Finally, Lenke classification was determined to describe the curve types [36].
Data analysis
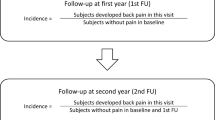
Statistical analyses were conducted with SPSS 20 (IBM Statistics). Sample size was calculated to detect a small correlation between radiological variables (i.e., Cobb angle) and pain intensity [37]. Thus, a sample of 124 individuals provided 92% of power to detect a correlation of 0.3 (moderate effect size) with 5% of level of significance. Categorical variables were presented as percentages. Continuous variables were submitted to the Kolmogorov–Smirnov test to evaluate normal distribution and were presented as mean ± standard deviation, median and interquartile range.
Similar to Djurasovic et al. [38], we divided the patient cohort into two groups based on the value of their preoperative SRS pain domain score. Patients with a preoperative pain domain score of 1 (severe), 2 (moderate to severe), or 3 (moderate) were categorized as painful scoliosis, whereas patients with a pain domain score of 4 (mild) or 5 (none) were categorized as the nonpainful scoliosis group. We compared the radiological and self-reported measures of patients reporting moderate to severe back pain over the last 30 days (pain group, N = 69) and those reporting minimal or no back pain (no pain group, N = 55) [38].
Comparisons between groups were conducted with chi-square tests for categorical variables, and Student t test or Mann–Whitney test for continuous variables, according to the distribution. Radiological parameters with P value less than 0.2 were included in the initial model of the logistic regression together with pain catastrophizing, trait anxiety, SRS30 self-image, and SRS30 mental health. Stepwise logistic regression using backward elimination method was applied to select the final model with independent variables associated with group membership (pain vs no pain group), which included only variables with P < 0.05.
In order to evaluate the overall contribution of radiological and psychological variables to the group membership, we conducted different multivariate logistic regressions. Discrimination ability was assessed using area under the ROC (receiver operating characteristic) curve for each model [39]. First, we assessed the discrimination ability of each radiological plane: axial plane model (AVR apical proximal thoracic, AVR main thoracic, AVR thoracolumbar/lumbar, torsion index), coronal plane model (Cobb proximal thoracic, Cobb main thoracic, Cobb thoracolumbar/lumbar, apical translation thoracic, apical translation lumbar, coronal balance, pelvic asymmetry), sagittal plane model (SVA, T1-T12 kyphosis, L1-S1 lordosis, PI, PT), and combinations. Finally, the discrimination ability of a biomechanical model with variables obtained by the SterEOS 3D reconstructions as well as a psychological model with pain catastrophizing and anxiety were tested.
Pearson correlation coefficient was used to assess the relationship between self-reported measures. Self-reported pain intensity according to the level of catastrophizing was evaluated using ANOVA with Bonferroni post-hoc tests. Preliminary analyses demonstrated significant association between catastrophizing and pain intensity. In order to assess the relationship between radiological parameters, catastrophizing and pain intensity, interaction terms between pain catastrophizing and the radiological variables were created. Multiple models of linear regressions were used to assess the association between radiographic parameters and pain intensity (NRS-average pain). First, we included in each model the interaction term and the main variables (pain catastrophizing and radiographic parameter). If the interaction was not statistically significant, it was then removed and the main effect of the variable was evaluated. Scatter plots with predicted values of pain intensity and the radiological variable according to different catastrophizing levels (PCS-C: low, 0–14; moderate, 15–25; and high, ≥ 26 [27]) were used to interpret the statistical interactions.
Results
Sample
A total of 124 patients with AIS were included in the study. Table 1 presents the demographic features of the sample. Radiographic parameters are summarized in Table 2. Curve types were most commonly Lenke 1 (main thoracic = 39.5%) or Lenke 2 (double thoracic = 26.6%) followed by Lenke 5 (thoracolumbar/lumbar = 12.9%), Lenke 6 (thoracolumbar/lumbar—main thoracic = 9.7%), Lenke 4 (triple major = 6.5%), and Lenke 3 (double major = 4.8%). From the 108 patients with a structural thoracic curve, only 4 (3.2%) had a left thoracic curve.
Back pain prevalence and associated factors
Overall, 90% of AIS patients reported having some back pain over the last 6 months and 85.8% over the last 30 days. Pain intensity in the last month was reported to be mild in 37.5%, moderate in 31.8%, moderate to severe in 24.3%, and severe in 6.54%. Overall, 20.8% reported not having pain at rest or rarely experiencing it (27.5%). Medication use for back pain was reported by 25% of the cohort, with 5.64% reporting opioid use.
Back pain was located in the upper or lower thoracic spine in 61.5%, lower back in 21.8% and both thoracic and lumbar region in 16.7% of patients. Location of back pain was associated with location of major curve (Fig. 1, P = 0.036). In addition, low back pain was associated with higher AVR in the lumbar apex (low back pain = 11.83 ± 11.91 degrees, thoracic pain = 10.05 ± 10.07 degrees, P = 0.02) and lower lumbar lordosis (low back pain = 46.22 ± 15.04 degrees, thoracic pain = 58.15 ± 15.32 degrees, P = 0.02).
Bivariate comparisons between the pain versus no pain groups demonstrated no differences in demographics (Table 1). Figure 2 shows the scores of self-reported measures according to the groups. AIS patients with pain presented greater scores in pain catastrophizing (mean difference = 7.36, CI95%: 3.61–11.12, P < 0.0001) and trait anxiety (mean difference = 4.04, CI95% 1.02–7.07, P = 0.009), and lower scores in level of function (mean difference = − 0.38, CI95% − 0.59–− 0.18, P < 0.0001), self-image perception (mean difference = − 0.35, CI95% − 0.58–− 0.12, P = 0.003), and self-reported state of mental health (mean difference = − 0.54, CI95% − 0.80–− 0.27, P < 0.0001). Bivariate analyses with biomechanical predictors of back pain are presented in Table 3. The initial model of multiple logistic regression contained the variables of body mass index, greatest Cobb angle, thoracolumbar Cobb angle, lumbar apical translation, AIR lower, thoracic kyphosis, pelvic asymmetry, PCS-C, trait anxiety, SRS30 self-image, and SRS30 mental-health. The final model of logistic regression is presented in Table 4. Independent risk factors for back pain in AIS were greater pain catastrophizing (B = 0.061, P = 0.035), poorer self-reported state of mental health (B = − 0.872, P = 0.023), decreased thoracic kyphosis (B = − 0.033, P = 0.044) and pelvic asymmetry (B = 0.146, P = 0.047).
Contribution of radiological and psychological factors to pain prevalence
Results of multivariate logistic regression models containing radiological variables from SterEOS 3D reconstructions demonstrated no discrimination ability of axial plane model (AUC: 0.56, P = 0.31. Good discrimination was observed with the sagittal plane (AUC: 0.66, P = 0.004) and coronal plane (AUC: 0.70, P = 0.002) models. Slight improvement was obtained with a model containing coronal and sagittal plane variables (AUC: 0.75, P < 0.0001). Overall, only a small improvement in model discrimination was obtained by adding axial plane variables (3 planes radiological model; AUC: 0.77, P < 0.0001).
Morphological and psychological models’ performances are demonstrated in Fig. 3. The morphological model’s ability to discriminate the presence of pain calculated by AUC was 0.78 (P < 0.0001) while the psychological presented an AUC of 0.74 (P < 0.0001). Performance of combined morphological and psychological models improved significantly the model performance (AUC: 0.91, P < 0.0001, Fig. 3).
Morphological and psychological models’ performances to predict pain versus no pain in adolescent idiopathic scoliosis. Note: Morphological model: area under the curve (AUC) = 0.78, P < 0.0001; Psychological model: AUC = 0.74, P < 0.0001; morphological and psychological models: AUC = 0.91, P < 0.0001
Association between pain intensity, psychological and radiographic parameters
There was a significant association between self-reported pain intensity in the last 24 h and levels of catastrophizing (Fig. 4). High level of catastrophizing was correlated with high levels of worst pain (r = 0.413, P < 0.0001), average pain (r = 0.314, P = 0.001), and best pain (r = 0.214, P = 0.034) experienced in the last 24 h. Greater level of catastrophizing was correlated with worse scores of pain (r = − 0.354, P < 0.0001), function (r = − 0.407, P < 0.0001), self-image (r = − 0.271, P = 0.006), and mental health (r = − 0.439, P < 0.0001) domains of SRS30. Trait anxiety was also correlated with pain intensity, function, self-image, and mental health (Table 5).
Association between radiographic parameters and pain intensity is demonstrated in Table 6. An interaction term between levels of pain catastrophizing and each one of radiographic variable was included in each linear regression model in order to evaluate the moderation effect of pain catastrophizing on the relationship between radiographic parameters and pain intensity. A statistically significant interaction PCS*Major Cobb angle (P = 0.031) and a main effect of Cobb angle (P = 0.045) on pain intensity were observed. A statistically significant interaction PCS*torsion index (P = 0.016) and a main effect of torsion (P = 0.025) on pain intensity were observed. In addition, a significant interaction between PCS*AIR upper major curve (P = 0.021) and main effect of AIR upper major curve (P = 0.043) were identified. The interactions between the radiographic variables and catastrophizing revealed that, in low catastrophizers, there is a significant association between greater spinal deformity (Cobb angle, torsion index, and AIR of the upper half of major curve) and higher pain levels (Fig. 5). For moderate and high catastrophizers, such positive correlation is absent.
Discussion
Despite being neglected for many years [2, 3], recent studies have highlighted that pain is an important issue in patients with AIS [1, 4, 37, 40]. Although the causal relationship is yet speculative given the cross-sectional designs, epidemiological studies have demonstrated that the prevalence of back pain is higher in AIS than in adolescents without scoliosis [41,42,43]. For example, in the study by Sato et al. [41], back pain in patients with AIS was reported as 27.5%, higher than adolescents without scoliosis (11.4%). Similarly, Kovacs et al. [43] observed an increased prevalence of back pain in schoolchildren reporting scoliosis (Odds-ratio = 2.87; CI95% 2.45–3.37). In a large database study with 1433 patients with AIS selected for surgery, Landman et al. [2] reported a prevalence of 73.6% of mild to severe back pain in the past month. Interestingly, mild to severe back pain was reported by 85.8% of patients in our study. To note, this study was designed specifically to evaluate pain in AIS, which could have contributed to this higher rate of pain complaint in our cohort.
There is growing evidence demonstrating that the spinal deformity is a pain generator in AIS. Recently, Bisson et al. [10] identified advanced deterioration in young facet joint cartilage tissue in AIS patients, comparable with individuals with osteoarthritis. In another study looking at pain neurophysiology of patients with AIS and chronic pain, our group demonstrated that deformity severity is associated with impaired pain processing and modulation [1]. The results of the current study provided further evidence for an association between deformity and back pain. First, decreased thoracic kyphosis and pelvic asymmetry were identified, while controlling for psychological variables, as independent predictors for having moderate to severe back pain. Decreased thoracic kyphosis is part of the tridimensional aspect of the AIS, thus its severity generally reflects the overall deformity severity. Reduced thoracic kyphosis is a well-known painful compensatory mechanism for loss of lumbar lordosis in adult spinal deformity [44]. Despite recognized in adults, this was the first study to show the association between thoracic hypokyphosis and back pain prevalence in AIS. In fact, there is convincing evidence demonstrating that facet joint loading causes spinal cord hyperexcitability contributing to pain chronification [45].
Pelvic asymmetry is very common in AIS and it is associated with deformity severity [32]. Radiographic measures of pelvic asymmetry include the pelvic obliquity angle and the difference in heights of femoral heads, also known as functional LLD (leg length discrepancy) [32, 46]. In patients with AIS, LLD can be functional (resulting from altered mechanics), or structural (associated with bony shortening) [47]. Functional is much more common than structural LLD in the AIS population [32]. In fact, the relative spinopelvic alignment is suggested as a compensatory mechanism to maintain trunk equilibrium [48]. In this sense, extension and flexion of the lower limbs compensate the lumbar curve. Difference in height of femoral heads is a reliable measure easily obtained from the StereoEOS reconstructions which is highly correlated with the pelvic obliquity angle [32]. In patients with neuromuscular scoliosis, this pelvic asymmetry is commonly associated with hip contractures and it is recognized as a pain generator [49]. To the best of our knowledge, this was the first study to identify an association between pelvic asymmetry (i.e., functional LLD) and back pain in AIS. The relationship between pelvic asymmetry and chronic back pain in the general population has been investigated [50,51,52,53]. In patients with AIS, pelvic asymmetry is known to be associated with unequal weight distribution, muscular imbalance of the trunk, and decreased postural stability, which may predispose patients to back pain [54,55,56]. In addition, pelvic asymmetry seems to alter the patterns of trunk movement and mechanics of the spine [51]. Our results suggest further exploration of pelvic measurements and LLD as a cause of back pain in AIS. Despite recognizing the exploratory nature of this study and the need for further validation of these findings, the identification of thoracic hypokyphosis and pelvic asymmetry as independent predictors for back pain highly suggests that the deformity itself has influence on back pain prevalence in this population. Furthermore, besides confirming the association between curve type and pain location [37], we observed that patients with pain located at the lower back region have greater axial rotation of the apical lumbar vertebrae.
Besides endorsing the link between morphology and pain, our results highlight the importance of investigating psychological aspects when evaluating chronic pain in AIS. For example, the regression model containing radiographic and psychological variables presented increased discrimination power in comparison with the model containing only radiological variables. In addition, pain catastrophizing was identified as a strong predictor for self-reported pain prevalence and intensity. In fact, pain catastrophizing is an important psychological construct in pediatric pain assessment [1, 27]. Despite being reported in other painful conditions [16,17,18,19,20,21], this was the first study to confirm this association in AIS. Our results show that pain catastrophizing moderates the association between deformity severity and pain intensity. Interestingly, the positive correlation between deformity severity and pain intensity was only seen in patients with low level of catastrophizing in our data. We recognize that further larger studies should better explore this topic, but our data suggest that the role of morphology for back pain in AIS is more evident in low catastrophizers. In other words, for moderate or higher catastrophizers, the deformity may not play a significant role for self-reported pain intensity. In light of the current biopsychosocial model of pain assessment [57], our study strikes the need for further exploration of psychosocial issues involved in AIS-related back pain. As the role of parental catastrophizing in children pain behavior is well-established [58, 59], this variable should be further explored in AIS-related pain.
Better characterization of pain mechanisms can potentially improve pain management [1, 60]. Even though pain research continues to advance, relatively little attention has been given to patients with AIS. For example, studies investigating the effect of bracing on back pain in AIS are usually retrospective and provide conflicting results [37, 61,62,63,64]. One might argue that a subset of patients have a higher component of mechanical pain that would benefit from bracing or even from more invasive procedures. On the other hand, certain psychological factors may predispose patients to pain chronification [65] despite the deformity management. In the same way, as adolescents are known to have different pain coping profiles [66, 67], the impact of different coping strategies should be explored in future studies. In summary, larger studies could better identify clusters of patients more likely to have pain driven by deformity or psychosocial components.
Using a standard 3D reconstruction technique [35] this was the first study to investigate the relationship between axial vertebral rotations and pain in this population. Results showed a main effect of torsion of the main curve and AIR of the upper half of the curve on self-reported pain intensity. In addition, higher axial vertebral rotation of the apical lumbar vertebra was associated with pain in the lower back. However, variables obtained with the axial plane reconstructions were not independent predictors of back pain and the model containing only axial plane variables had no discrimination for painful scoliosis. These results suggest that the axial rotation may have a lower effect on pain generation in comparison to coronal or sagittal loading. Another possible explanation is that, despite being the most accurate method, the average 2.4° measurement error [35] with sterEOS 3D reconstruction could impact the results. The reliability of EOS has been investigated by several authors [68,69,70,71].
This study presents several limitations that should be considered. First, as the study was designed specifically to assess pain in patients undergoing surgery and that pain is not considered an indication for surgery in AIS, it is possible that there was a bias towards patients with pain and their likelihood to participate in the study. As previously mentioned, we observed a high prevalence of self-reported pain. Moreover, the mean reported pain intensity in our study was 2.66 (± 2.18), slightly higher than the study by Théroux et al. [37] (1.63 ± 1.89). Second, in order to identify predictors for painful versus non-painful scoliosis, we used the same arbitrary criteria adopted by Djurasovic et al. [38]: no or mild pain representing the non-painful group versus moderate to severe pain representing the painful group. As pain is a subjective experience, future studies with larger sample sizes should further validate our findings including patients with mild pain. Third, these results may not be applicable for patients with mild scoliosis (i.e., Cobb angle from 10 to 25 degrees), frequently seen in spine clinics. Fourth, no positive psychological factors were assessed in this study (e.g., pain acceptance, self-efficacy, social supports). Fifth, one should recognize that there are multiple reasons for having catastrophizing thoughts about pain in this population that should be explored in further studies (e.g., knowledge of scoliosis, knowledge of pain pathways, untreated anxiety, etc.). It is important to highlight that pain catastrophizing is defined as a negative orientation or mental set about actual or anticipated pain [15]. This trait-based concept is assessed in PCS as the tendency toward engaging in magnification, rumination, and helplessness “when in pain”, with participants asked to reflect on an unspecified painful experience. The questionnaire, thus, evaluate pain catastrophizing as a trait, that is, a stable tendency or predisposition to catastrophize. The item content of the PCS magnification and rumination scales taps both cognitive content (i.e., what people think) as well as cognitive process (i.e., how people think), while the helplessness scale taps both of these coping domains as well as emotional coping. It was reported that scores on the PCS remain stable across time and that the PCS is appropriate for measuring trait pain catastrophizing in both clinical pain and nonclinical populations [15]. PCS scores have been found to correlate with measures of other stable traits, including personality traits [72]. This data support the validity of the trait-based conceptualization of catastrophizing of PCS, the major psychological instrument used in our study. Finally, similarly to the previous studies in the field, the cross-sectional design precludes absolute conclusions on the causality of radiographic factors and back pain prevalence and intensity.
Conclusions
Despite the limitations, this exploratory study demonstrated that morphological and psychological factors are related to pain in AIS. Pain is associated with worse quality of life measures. Moreover, pain catastrophizing is an important construct in AIS-related pain and should be taken into consideration when evaluating these patients.
References
Teles AR, Ocay DD, Bin Shebreen A, Tice A, Saran N, Ouellet JA, Ferland CE (2019) Evidence of impaired pain modulation in adolescents with idiopathic scoliosis and chronic back pain. Spine J 19:677–686. https://doi.org/10.1016/j.spinee.2018.10.009
Landman Z, Oswald T, Sanders J, Diab M, Spinal Deformity Study G (2011) Prevalence and predictors of pain in surgical treatment of adolescent idiopathic scoliosis. Spine 36:825–829. https://doi.org/10.1097/BRS.0b013e3181de8c2b
Ramirez N, Johnston CE, Browne RH (1997) The prevalence of back pain in children who have idiopathic scoliosis. J Bone Joint Surg Am 79:364–368
Theroux J, Le May S, Fortin C, Labelle H (2015) Prevalence and management of back pain in adolescent idiopathic scoliosis patients: a retrospective study. Pain Res Manag 20:153–157
Morse LJ, Kawakami N, Lenke LG, Sucato DJ, Sanders JO, Diab M (2012) Culture and ethnicity influence outcomes of the Scoliosis Research Society Instrument in adolescent idiopathic scoliosis. Spine 37:1072–1076. https://doi.org/10.1097/BRS.0b013e31823ed962
Pellegrino LN, Avanzi O (2014) Prospective evaluation of quality of life in adolescent idiopathic scoliosis before and after surgery. J Spinal Disord Tech 27:409–414. https://doi.org/10.1097/BSD.0b013e3182797a5e
Weiss HR (2008) Adolescent idiopathic scoliosis (AIS)—an indication for surgery? A systematic review of the literature. Disabil Rehabil 30:799–807. https://doi.org/10.1080/09638280801889717
Balague F, Pellise F (2016) Adolescent idiopathic scoliosis and back pain. Scoliosis Spinal Disord 11:27. https://doi.org/10.1186/s13013-016-0086-7
Matamalas A, Bago J, D'Agata E, Pellise F (2014) Body image in idiopathic scoliosis: a comparison study of psychometric properties between four patient-reported outcome instruments. Health Qual Life Outcomes 12:81. https://doi.org/10.1186/1477-7525-12-81
Bisson D, Lama D, Abduljabbar F, Rosenzweig DH, Saran N, Ouellet JA, Haglund L (2018) Facet joint degeneration in adolescent idiopathic scoliosis. JOR Spine. https://doi.org/10.1002/jsp2.1016
Ferrero E, Lafage R, Diebo BG, Challier V, Illharreborde B, Schwab F, Skalli W, Guigui P, Lafage V (2017) Tridimensional analysis of rotatory subluxation and sagittal spinopelvic alignment in the setting of adult spinal deformity. Spine Deform 5:255–264. https://doi.org/10.1016/j.jspd.2017.01.003
Trammell TR, Schroeder RD, Reed DB (1988) Rotatory olisthesis in idiopathic scoliosis. Spine 13:1378–1382
Shen J, Kadoury S, Labelle H, Roy-Beaudry M, Aubin CE, Parent S (2017) Geometric torsion in adolescent idiopathic scoliosis: a new method to differentiate between Lenke 1 subtypes. Spine 42:E532–E538. https://doi.org/10.1097/BRS.0000000000001866
Shen J, Kadoury S, Labelle H, Parent S (2016) Geometric torsion in adolescent idiopathic scoliosis: a surgical outcomes study of lenke type 1 patients. Spine 41:1903–1907. https://doi.org/10.1097/BRS.0000000000001651
Sullivan MJ, Thorn B, Haythornthwaite JA, Keefe F, Martin M, Bradley LA, Lefebvre JC (2001) Theoretical perspectives on the relation between catastrophizing and pain. Clin J Pain 17:52–64
Severeijns R, Vlaeyen JW, van den Hout MA, Weber WE (2001) Pain catastrophizing predicts pain intensity, disability, and psychological distress independent of the level of physical impairment. Clin J Pain 17:165–172
Wojtowicz AA, Greenley RN, Gumidyala AP, Rosen A, Williams SE (2014) Pain severity and pain catastrophizing predict functional disability in youth with inflammatory bowel disease. J Crohns Colitis 8:1118–1124. https://doi.org/10.1016/j.crohns.2014.02.011
Asmundson GJ, Noel M, Petter M, Parkerson HA (2012) Pediatric fear-avoidance model of chronic pain: foundation, application and future directions. Pain Res Manag 17:397–405
Vervoort T, Eccleston C, Goubert L, Buysse A, Crombez G (2010) Children's catastrophic thinking about their pain predicts pain and disability 6 months later. Eur J Pain 14:90–96. https://doi.org/10.1016/j.ejpain.2009.03.001
Crombez G, Bijttebier P, Eccleston C, Mascagni T, Mertens G, Goubert L, Verstraeten K (2003) The child version of the pain catastrophizing scale (PCS-C): a preliminary validation. Pain 104:639–646
Guite JW, McCue RL, Sherker JL, Sherry DD, Rose JB (2011) Relationships among pain, protective parental responses, and disability for adolescents with chronic musculoskeletal pain: the mediating role of pain catastrophizing. Clin J Pain 27:775–781. https://doi.org/10.1097/AJP.0b013e31821d8fb4
Walker LS, Sherman AL, Bruehl S, Garber J, Smith CA (2012) Functional abdominal pain patient subtypes in childhood predict functional gastrointestinal disorders with chronic pain and psychiatric comorbidities in adolescence and adulthood. Pain 153:1798–1806. https://doi.org/10.1016/j.pain.2012.03.026
Miro J, Castarlenas E, Huguet A (2009) Evidence for the use of a numerical rating scale to assess the intensity of pediatric pain. Eur J Pain 13:1089–1095. https://doi.org/10.1016/j.ejpain.2009.07.002
Ruskin D, Lalloo C, Amaria K, Stinson JN, Kewley E, Campbell F, Brown SC, Jeavons M, McGrath PA (2014) Assessing pain intensity in children with chronic pain: convergent and discriminant validity of the 0 to 10 numerical rating scale in clinical practice. Pain Res Manag 19:141–148
Beausejour M, Joncas J, Goulet L, Roy-Beaudry M, Parent S, Grimard G, Forcier M, Lauriault S, Labelle H (2009) Reliability and validity of adapted French Canadian version of Scoliosis Research Society Outcomes Questionnaire (SRS-22) in Quebec. Spine 34:623–628. https://doi.org/10.1097/BRS.0b013e3181973e58
Parkerson HA, Noel M, Page MG, Fuss S, Katz J, Asmundson GJ (2013) Factorial validity of the English-language version of the Pain Catastrophizing Scale–child version. J Pain 14:1383–1389. https://doi.org/10.1016/j.jpain.2013.06.004
Pielech M, Ryan M, Logan D, Kaczynski K, White MT, Simons LE (2014) Pain catastrophizing in children with chronic pain and their parents: proposed clinical reference points and reexamination of the Pain Catastrophizing Scale measure. Pain 155:2360–2367. https://doi.org/10.1016/j.pain.2014.08.035
Canals J, Marti-Henneberg C, Fernandez-Ballart J, Cliville R, Domenech E (1992) Scores on the State-Trait Anxiety Inventory for children in a longitudinal study of pubertal Spanish youth. Psychol Rep 71:503–512. https://doi.org/10.2466/pr0.1992.71.2.503
Schisler T, Lander J, Fowler-Kerry S (1998) Assessing children's state anxiety. J Pain Symptom Manag 16:80–86
Julian LJ (2011) Measures of anxiety: State-Trait Anxiety Inventory (STAI), Beck Anxiety Inventory (BAI), and Hospital Anxiety and Depression Scale-Anxiety (HADS-A). Arthritis Care Res (Hoboken) 63(Suppl 11):S467–472. https://doi.org/10.1002/acr.20561
Sangole A, Aubin CE, Labelle H, Lenke L, Jackson R, Newton P, Stokes IA, Scoliosis Research Society DSC (2010) The central hip vertical axis: a reference axis for the Scoliosis Research Society three-dimensional classification of idiopathic scoliosis. Spine 35:E530–534. https://doi.org/10.1097/BRS.0b013e3181da38b8
Sekiya T, Aota Y, Yamada K, Kaneko K, Ide M, Saito T (2018) Evaluation of functional and structural leg length discrepancy in patients with adolescent idiopathic scoliosis using the EOS imaging system: a prospective comparative study. Scoliosis Spinal Disord 13:7. https://doi.org/10.1186/s13013-018-0152-4
Ferrero E, Lafage R, Challier V, Diebo B, Guigui P, Mazda K, Schwab F, Skalli W, Lafage V (2015) Clinical and stereoradiographic analysis of adult spinal deformity with and without rotatory subluxation. Orthop Traumatol Surg Res 101:613–618. https://doi.org/10.1016/j.otsr.2015.04.008
Steib JP, Dumas R, Mitton D, Skalli W (2004) Surgical correction of scoliosis by in situ contouring: a detorsion analysis. Spine 29:193–199. https://doi.org/10.1097/01.BRS.0000107233.99835.A4
Boyer L, Shen J, Parent S, Kadoury S, Aubin CE (2018) Accuracy and precision of seven radiography-based measurement methods of vertebral axial rotation in adolescent idiopathic scoliosis. Spine Deform 6:351–357. https://doi.org/10.1016/j.jspd.2017.12.004
Lenke LG, Betz RR, Harms J, Bridwell KH, Clements DH, Lowe TG, Blanke K (2001) Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis. J Bone Joint Surg Am 83:1169–1181
Theroux J, Le May S, Hebert JJ, Labelle H (2017) Back pain prevalence is associated with curve-type and severity in adolescents with idiopathic scoliosis: a cross-sectional study. Spine 42:E914–E919. https://doi.org/10.1097/BRS.0000000000001986
Djurasovic M, Glassman SD, Sucato DJ, Lenke LG, Crawford CH 3rd, Carreon LY (2018) Improvement in scoliosis research society-22r pain scores after surgery for adolescent idiopathic scoliosis. Spine 43:127–132. https://doi.org/10.1097/BRS.0000000000001978
Steyerberg EW, Vickers AJ, Cook NR, Gerds T, Gonen M, Obuchowski N, Pencina MJ, Kattan MW (2010) Assessing the performance of prediction models: a framework for traditional and novel measures. Epidemiology 21:128–138. https://doi.org/10.1097/EDE.0b013e3181c30fb2
Topalis C, Grauers A, Diarbakerli E, Danielsson A, Gerdhem P (2017) Neck and back problems in adults with idiopathic scoliosis diagnosed in youth: an observational study of prevalence, change over a mean four year time period and comparison with a control group. Scoliosis Spinal Disord 12:20. https://doi.org/10.1186/s13013-017-0125-z
Sato T, Hirano T, Ito T, Morita O, Kikuchi R, Endo N, Tanabe N (2011) Back pain in adolescents with idiopathic scoliosis: epidemiological study for 43,630 pupils in Niigata City, Japan. Eur Spine J 20:274–279. https://doi.org/10.1007/s00586-010-1657-6
Calvo-Munoz I, Gomez-Conesa A, Sanchez-Meca J (2013) Prevalence of low back pain in children and adolescents: a meta-analysis. BMC Pediatr 13:14. https://doi.org/10.1186/1471-2431-13-14
Kovacs FM, Gestoso M, Gil del Real MT, Lopez J, Mufraggi N, Mendez JI (2003) Risk factors for non-specific low back pain in schoolchildren and their parents: a population based study. Pain 103:259–268
Barrey C, Roussouly P, Le Huec JC, D'Acunzi G, Perrin G (2013) Compensatory mechanisms contributing to keep the sagittal balance of the spine. Eur Spine J 22(Suppl 6):S834–841. https://doi.org/10.1007/s00586-013-3030-z
Quinn KP, Dong L, Golder FJ, Winkelstein BA (2010) Neuronal hyperexcitability in the dorsal horn after painful facet joint injury. Pain 151:414–421. https://doi.org/10.1016/j.pain.2010.07.034
Sabharwal S, Zhao C, McKeon JJ, McClemens E, Edgar M, Behrens F (2006) Computed radiographic measurement of limb-length discrepancy. Full-length standing anteroposterior radiograph compared with scanogram. J Bone Joint Surg Am 88:2243–2251. https://doi.org/10.2106/JBJS.E.01179
Gurney B (2002) Leg length discrepancy. Gait Posture 15:195–206
Pasha S, Aubin CE, Sangole AP, Labelle H, Parent S, Mac-Thiong JM (2014) Three-dimensional spinopelvic relative alignment in adolescent idiopathic scoliosis. Spine 39:564–570. https://doi.org/10.1097/BRS.0000000000000193
Winter RB, Pinto WC (1986) Pelvic obliquity. Its causes and its treatment. Spine 11:225–234
Levangie PK (1999) The association between static pelvic asymmetry and low back pain. Spine 24:1234–1242
Al-Eisa E, Egan D, Deluzio K, Wassersug R (2006) Effects of pelvic skeletal asymmetry on trunk movement: three-dimensional analysis in healthy individuals versus patients with mechanical low back pain. Spine 31:E71–79. https://doi.org/10.1097/01.brs.0000197665.93559.04
Havran M, Scholten JD, Breuer P, Lundberg J, Kochersberger G, Newman D, Weiner DK (2016) Deconstructing chronic low back pain in the older adult-step-by-step evidence and expert-based recommendations for evaluation and treatment: part XII: leg length discrepancy. Pain Med 17:2230–2237. https://doi.org/10.1093/pm/pnw270
Rannisto S, Okuloff A, Uitti J, Paananen M, Rannisto PH, Malmivaara A, Karppinen J (2015) Leg-length discrepancy is associated with low back pain among those who must stand while working. BMC Musculoskelet Disord 16:110. https://doi.org/10.1186/s12891-015-0571-9
Nault ML, Allard P, Hinse S, Le Blanc R, Caron O, Labelle H, Sadeghi H (2002) Relations between standing stability and body posture parameters in adolescent idiopathic scoliosis. Spine 27:1911–1917
Sahli S, Rebai H, Ghroubi S, Yahia A, Guermazi M, Elleuch MH (2013) The effects of backpack load and carrying method on the balance of adolescent idiopathic scoliosis subjects. Spine J 13:1835–1842. https://doi.org/10.1016/j.spinee.2013.06.023
Jung JY, Cha EJ, Kim KA, Won Y, Bok SK, Kim BO, Kim JJ (2015) Influence of pelvic asymmetry and idiopathic scoliosis in adolescents on postural balance during sitting. Biomed Mater Eng 26(Suppl 1):S601–610. https://doi.org/10.3233/BME-151351
Lumley MA, Cohen JL, Borszcz GS, Cano A, Radcliffe AM, Porter LS, Schubiner H, Keefe FJ (2011) Pain and emotion: a biopsychosocial review of recent research. J Clin Psychol 67:942–968. https://doi.org/10.1002/jclp.20816
Caes L, Vervoort T, Eccleston C, Goubert L (2012) Parents who catastrophize about their child's pain prioritize attempts to control pain. Pain 153:1695–1701. https://doi.org/10.1016/j.pain.2012.04.028
Caes L, Vervoort T, Eccleston C, Vandenhende M, Goubert L (2011) Parental catastrophizing about child's pain and its relationship with activity restriction: the mediating role of parental distress. Pain 152:212–222. https://doi.org/10.1016/j.pain.2010.10.037
Vardeh D, Mannion RJ, Woolf CJ (2016) Toward a mechanism-based approach to pain diagnosis. J Pain 17:T50–69. https://doi.org/10.1016/j.jpain.2016.03.001
Misterska E, Glowacki J, Okret A, Laurentowska M, Glowacki M (2017) Back and neck pain and function in females with adolescent idiopathic scoliosis: a follow-up at least 23 years after conservative treatment with a Milwaukee brace. PLoS ONE 12:e0189358. https://doi.org/10.1371/journal.pone.0189358
Smorgick Y, Mirovsky Y, Baker KC, Gelfer Y, Avisar E, Anekstein Y (2013) Predictors of back pain in adolescent idiopathic scoliosis surgical candidates. J Pediatr Orthop 33:289–292. https://doi.org/10.1097/BPO.0b013e31827d0b43
Joncas J, Labelle H, Poitras B, Duhaime M, Rivard CH, Le Blanc R (1996) Dorso-lumbal pain and idiopathic scoliosis in adolescence. Ann Chir 50:637–640
Deceuninck J, Bernard JC (2012) Quality of life and brace-treated idiopathic scoliosis: a cross-sectional study performed at the Centre des Massues on a population of 120 children and adolescents. Ann Phys Rehabil Med 55:93–102. https://doi.org/10.1016/j.rehab.2011.12.003
Holley AL, Wilson AC, Palermo TM (2017) Predictors of the transition from acute to persistent musculoskeletal pain in children and adolescents: a prospective study. Pain 158:794–801. https://doi.org/10.1097/j.pain.0000000000000817
Simons LE, Claar RL, Logan DL (2008) Chronic pain in adolescence: parental responses, adolescent coping, and their impact on adolescent's pain behaviors. J Pediatr Psychol 33:894–904. https://doi.org/10.1093/jpepsy/jsn029
Claar RL, Baber KF, Simons LE, Logan DE, Walker LS (2008) Pain coping profiles in adolescents with chronic pain. Pain 140:368–375. https://doi.org/10.1016/j.pain.2008.09.007
Al-Aubaidi Z, Lebel D, Oudjhane K, Zeller R (2013) Three-dimensional imaging of the spine using the EOS system: is it reliable? A comparative study using computed tomography imaging. J Pediatr Orthop B 22:409–412. https://doi.org/10.1097/BPB.0b013e328361ae5b
Gille O, Champain N, Benchikh-El-Fegoun A, Vital JM, Skalli W (2007) Reliability of 3D reconstruction of the spine of mild scoliotic patients. Spine 32:568–573. https://doi.org/10.1097/01.brs.0000256866.25747.b3
Ilharreborde B, Steffen JS, Nectoux E, Vital JM, Mazda K, Skalli W, Obeid I (2011) Angle measurement reproducibility using EOS three-dimensional reconstructions in adolescent idiopathic scoliosis treated by posterior instrumentation. Spine 36:E1306–1313. https://doi.org/10.1097/BRS.0b013e3182293548
Glaser DA, Doan J, Newton PO (2012) Comparison of 3-dimensional spinal reconstruction accuracy: biplanar radiographs with EOS versus computed tomography. Spine 37:1391–1397. https://doi.org/10.1097/BRS.0b013e3182518a15
Quartana PJ, Campbell CM, Edwards RR (2009) Pain catastrophizing: a critical review. Expert Rev Neurother 9:745–758. https://doi.org/10.1586/ern.09.34
Acknowledgements
The study was financially supported by AOTK (CEF, JAO and MSG) and the Shriners Hospitals (CEF and JAO).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest related to this work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Teles, A.R., St-Georges, M., Abduljabbar, F. et al. Back pain in adolescents with idiopathic scoliosis: the contribution of morphological and psychological factors. Eur Spine J 29, 1959–1971 (2020). https://doi.org/10.1007/s00586-020-06489-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-020-06489-2