Abstract
Purpose
The objective of this study was to test the correlation between the apex of lumbar lordosis (LLA) and pelvic incidence (PI) in asymptomatic adults, and to establish predictive formulae based on the PI to obtain the reference values of lumbar sagittal parameters.
Methods
A cohort of 183 asymptomatic volunteers older than 18 years was enrolled in this study between April 2017 and May 2019. A full-spine, standing X-ray was taken for each subject. The following parameters in the sagittal plane were measured: the LLA, the distance between the plumb line of the lumbar apex (LAPL) and gravity plumb line, lumbar lordosis (LL), the upper arc of lumbar lordosis (LLUA), the lower arc of lumbar lordosis (LLLA) and the PI. The correlations between lumbar parameters and PI were analysed, and simple linear regressions were simultaneously constructed. The statistical significance level was P < 0.05.
Results
The PI was statistically correlated with the LLA (rs = − 0.595, P < 0.001), LAPL (rs = 0.503, P < 0.001), LL (rs = 0.605, P < 0.001), LLUA (r = 0.354, P < 0.001) and the LLLA (r = 0.658, P < 0.001). The corresponding regression formulae were as follows: LLA = − 0.042*PI + 6.134 (R2 = 0.306), LAPL = 0.448*PI + 26.570 (R2 = 0.279), LL = 0.888*PI − 2.667 (R2 = 0.370), LLUA = 0.272*PI − 2.297 (R2 = 0.126) and LLLA = 0.607*PI + 0.177 (R2 = 0.433).
Conclusion
The PI has strong correlations with the LLA, LAPL, LL, LLUA and LLLA, which demonstrates that the specific lumbar shape can be affected by the pelvic morphology. Moreover, predictive models for ideal lumbar sagittal parameters based on the PI have been developed, contributing to the design of precise and individualized preoperative plans.
Graphic abstract
These slides can be retrieved under Electronic Supplementary Material.

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Spino-pelvic sagittal alignment is considered to have a large influence on the health-related quality of life of adults [1, 2]. The human pelvis plays a key role in regulating spinal alignment and maintaining an erect posture by the interactions of the spine and pelvis [3,4,5,6]. Duval-Beaupere et al. [3, 6] introduced three common parameters to systematically define the geometry and position of the pelvis. Among the parameters, there are two positional parameters (pelvic tilt, PT and sacral slope, SS) and one morphological parameter (pelvic incidence, PI) [5]. In contrast to the positional parameters, PI is unaffected by positions, and it is widely regarded as an anatomical parameter that remains constant over the lifetime of an adult [3, 4, 7]. PI has a direct effect on the lumbar curvature of a specific individual [3, 8]. Several data sets have been reported, suggesting there is a strong correlation between lumbar lordosis (LL) and PI in both normal and pathologic situations [9,10,11,12,13,14].
The apex of lumbar lordosis (LLA) can affect the shape of the lumbar spine; additionally, LLA is also a significant parameter to evaluate lumbar alignment [5, 11, 12]. Especially in corrective surgeries for lumbar deformities, the identification of the proper position of the LLA is of prime importance for surgeons to better reconstruct the lumbar alignment. However, to the best of our knowledge, the relationship between the LLA and PI remains unclear.
The present study mainly aimed to explore the correlations between LLA and PI in asymptomatic adults. By virtue of the predictive formulae, the authors attempted to obtain the reference values of lumbar sagittal parameters to tailor a more accurate surgical correction strategy for patients.
Materials and methods
Patient population
A cohort of 183 asymptomatic volunteers older than 18 years was recruited from our institution between April 2017 and May 2019 and enrolled in this retrospective study. The exclusion criteria were (1) a lumbar or thoracic disease, (2) a hip joint or pelvic disease, (3) a history of spinal surgery and (4) a neurological or neuromuscular disease. Written informed consent was obtained from all subjects who participated in this study, and ethical approval was provided by the local relevant committee.
Radiographic measurements
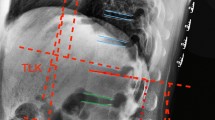
Posterior–anterior and lateral radiographic films of the full spine were obtained as the subjects stood in a standardized erect posture [15]. A number of distance and angular parameters were all measured twice by the same trained spine surgeon, and the average value was used as the final result. First, the location of the LLA, defined as the most anterior lumbar vertebra or disc in the sagittal plane [9], was measured. Vertebrae from L1 to L5 were assigned numbers ranging from 1 to 5 to simplify data collection as well as to facilitate correlation analysis. When the apex was located at a disc between two vertebrae, a value of 0.5 was added to the superior vertebra number. For instance, when the apex was located at the disc between L4 and L5, the value of the LLA was recorded as 4.5. The distance parameter of the sagittal vertical axis was measured between the plumb line of the lumbar apex (LAPL) and that of the posterosuperior corner of the sacrum [14]. The LLA divides the LL into two separate arcs of a circle: the upper arc of lumbar lordosis (LLUA) and the lower arc of lumbar lordosis (LLLA); the LLLA is geometrically equal to the SS (Fig. 1) [12]. Furthermore, the following parameters were measured in the sagittal plane: LL, LLUA, LLLP or SS and PI.
Statistical analysis
The data were analysed using SPSS 17.0 statistical software (SPSS Inc., Chicago, IL). All parameters were expressed as means and standard deviations (SDs). Distribution normality of data was tested by a Shapiro–Wilk test. The correlations between lumbar sagittal parameters and PI were analysed using the Pearson or Spearman correlation coefficient, and simple linear regressions were simultaneously conducted. The statistical significance threshold was P < 0.05.
Results
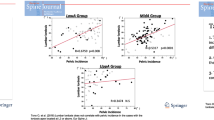
A total of 183 adults (91 females and 92 males) with a mean age of 48.4 ± 14.9 years (range 18–72 years) participated in the present study. The distribution of volunteers according to the age was as follows: age ≤ 30 years, 30 years < age ≤ 40 years, 40 years < age ≤ 50 years, 50 years < age ≤ 60 years and age > 60 years were 31 (16.9%), 30 (16.4%), 33 (18.0%), 46 (25.1%) and 43 (23.5%), respectively. The descriptive statistics and a spectrum of the normal variations in the spino-pelvic sagittal parameters are detailed in Table 1. In this cohort, the LLA was approximately located at the L4 vertebral body (4.2 ± 0.8) on average, with a range from T12/L1 proximally to L5/S1 distally; the average value of the LAPL was 47.7 ± 9.1 mm, with a range from 31.3 to 86.4 mm. The range of values indicated that spino-pelvic sagittal parameters were highly variable in asymptomatic individuals. It was found that the data of LLA, LAPL and LL were not normally distributed. Additionally, the correlations between the lumbar sagittal parameters and PI are summarized in Table 2, and the regression models employed are displayed in Fig. 2. The authors found that PI was statistically correlated with the LLA (rs = − 0.595, P < 0.001, LLA = − 0.042*PI + 6.134, R2 = 0.306), LAPL (rs = 0.503, P < 0.001, LAPL = 0.448*PI + 26.570, R2 = 0.279), LL (rs = 0.605, P < 0.001, LL = 0.888*PI − 2.667, R2 = 0.370), the LLUA (r = 0.354, P < 0.001, LLUA = 0.272*PI − 2.297, R2 = 0.126) and the LLLA or SS (r = 0.658, P < 0.001, LLLA or SS = 0.607*PI + 0.177, R2 = 0.433). The representative cases are shown in Figs. 3, 4, 5.
Discussion
Spino-pelvic sagittal alignment has been confirmed to play a more important role in pain and functional disability than coronal alignment in adults [16,17,18]. The pelvis, which couples the lumbar spine with the lower extremities, is capable of modulating the spinal sagittal alignment and, in particular, the lumbar alignment [3,4,5]. A thorough understanding of the reciprocal associations between lumbar alignment and the pelvis is helpful to comprehend the reasons for the specific shapes of the spine in various individuals. Simultaneously, a restoration of an appropriate sagittal alignment by surgery, especially for an individual with lumbar lordosis superior to the pelvis, is crucial for enhancing the quality of life of the individual and improving postoperative outcomes [19, 20].
Prior studies have commonly reported correlations between spinal alignment and the pelvis [9,10,11,12,13,14]. One of these studies is a seminal study on the Roussouly classification, which takes into consideration the SS, PI, LLA, inflection point, lordosis tilt angle and global sagittal balance [12]. According to the SS orientation, the authors introduced four types of lumbar lordosis in a normal adult population, and each type possessed a distinct spino-pelvic morphological characteristic. However, the primary limitation of this classification criterion is the use of a positional parameter, SS, rather than a morphological parameter. SS, representing the tilt degree of the superior endplate of S1 at a certain position of the pelvis, can change with the rotation of the pelvis. The use of a posture-dependent parameter could have a negative impact on the reliability and accuracy of this evaluation system. Concurrently, a preoperative spinal deformity can cause pelvic compensatory retroversion, resulting in a smaller SS than the original SS. If surgeons carry out a spinal reconstructive surgery simply by relying on the SS, a spino-pelvic mismatch may occur.
Relevant studies are still in development. PI, an approximately stable intrinsic parameter during adulthood, is usually characterized as pelvic morphology and unaffected by different postures of the trunk and extremities [3, 4, 7]; therefore, it is more important to test its relationship with lumbar alignment. Many previously published papers have highlighted that the PI is able to predict the ideal sagittal profile of the lumbar spine [3, 8,9,10,11,12,13,14]. On the basis of the strong correlation between LL and PI identified in such investigations, regression analyses were also applied to predict LL given certain pelvic parameters, especially PI. Vialle et al. [16] and Legaye et al. [21] were the groups to first report formulae that determined LL solely from PI. Later, using the predictive formula for LL in a cohort of 75 patients without an identified spino-pelvic pathology, Schwab et al. [4] proposed an approximation equation to simplify the strategy of treatment: LL = PI ± 9°. Kim et al. [22] continued to improve the predictive model, and they determined that the criterion to maintain sagittal balance was TK + LL + PI < 45°.
The above formulae provide valid models for the optimal LL when conducting a surgical correction for an adult spinal deformity. Nonetheless, LL is an angular value between the superior endplates of L1 and S1, and subjects with identical LL values are likely to exhibit different lumbar profiles. Surgeons may have difficulty completing lumbar fixation with a well-balanced shape when they solely know the value of the overall LL instead of the accurate lumbar contour. Roussouly et al. [12] and Hyun et al. [14] analysed and characterized lumbar geometry on the basis of a variety of specific sagittal parameters, such as the LLA, LLUA, LLLA and LAPL. However, there are few studies on the correlations between these parameters and PI in asymptomatic adult populations. Hence, the authors tried to design this study to advance the field of research on this topic.
In this study, the authors established a data set that describes spino-pelvic sagittal alignment in healthy volunteers, and the preliminary observations revealed that a high degree of variability existed in spino-pelvic sagittal parameters. Next, the authors performed a correlation analysis and simple linear regressions for every sagittal parameter. The LLA correlated significantly with the PI (rs = − 0.595, P < 0.001). In other words, the normal position of the LLA could vary along with the pelvic morphology, which is in accordance with the essential principles of the Roussouly classification. It can be assumed that the PI increases as the LLA becomes located more cranially. In an effort to provide a reference value for an ideal LLA, the following formula was additionally presented in this paper: LLA = − 0.042*PI + 6.134 (R2 = 0.306). Consequently, surgeons need to construct a suitable position of the LLA by relying on the PI value when implementing spinal corrections in diverse individuals.
In addition, a very strong correlation was observed between the LAPL and PI (rs = 0.503, P < 0.001). Because the gravity line of humans passes through the posterosuperior corner of S1 [5], the LAPL indicates the horizontal distance of the LLA from the axis of gravity. To some extent, the LAPL also reflects the degree of lumbar curvature. The predictive algorithm for the LAPL that requires PI is listed in this paper, as LAPL = 0.448*PI + 26.570 (R2 = 0.279), which could provide a reference for the correction target. It can be speculated that both the LAPL and the degree of lumbar curvature should be augmented associated with a high PI. In general, it is irrational for surgeons to focus only on the value of LL and ignore the importance of the LLA and LAPL in setting goals for treatment; focusing only on the LL may result in an unreasonable gravity line, lumbar–pelvic mismatch and eventual postoperative implant failure.
Prior studies have shown a very strong association of LL with PI [9,10,11,12,13,14], but the authors further expanded the investigations of the relationship between other lumbar parameters and PI. The majority of the previous studies measured the entire LL instead of the segmental angle in the lumbar spine. The characteristics of a lumbar curvature can be evaluated better by two segments, above and below the apex of curvature (LLUA and LLLA), than as a whole; this evaluation is not only feasible but also effective to guide surgical interventions. It should be noted that the LLLA from the superior endplate of S1 to a horizontal line located at the LLA identifies the SS in a geometrical relationship [12].
By means of correlation analysis, PI was verified to correlate significantly with the LL (rs = 0.605, P < 0.001), LLUA (r = 0.354, P < 0.001) and LLLA or SS (r = 0.658, P < 0.001). Moreover, the corresponding regression equations that depend exclusively on PI are listed as follows: LL = 0.888*PI − 2.667 (R2 = 0.370), LLUA = 0.272*PI − 2.297 (R2 = 0.126) and LLLA or SS = 0.607*PI + 0.177 (R2 = 0.433). In the case of a large PI, the tilt level of the superior endplate of S1 with respect to the horizontal axis or the SS will increase proportionally. As the superior endplate of S1 becomes more oblique, the LLLA has to be augmented even more in terms of the magnitude and number of vertebrae to match the pelvic morphology. As previously mentioned, for a subject with a large PI, the LLA should be located superiorly, and the curvature of the LL should be large. In contrast, when the PI decreases, the LL accordingly decreases, and the LLA moves inferiorly. In other words, a large PI is associated with a curved and long lumbar lordosis; conversely, a low PI is accompanied by a relatively flat and short lumbar lordosis. Figures 3, 4, 5 can contribute to understanding better the concept of LLA moving up and down with changes in PI. Furthermore, the achieved LL target, particularly the LLLA, should match the pelvic parameters, since the lower lumbar spine is considered the most crucial determinant of global lordosis and the most important treatment area for degenerative lumbar diseases [12, 23, 24].
In this paper, the authors explored the relationships between lumbar sagittal parameters and PI, especially LLA and LAPL, which filled some gaps in the research on the spino-pelvic sagittal balance. The above positive results can facilitate a better understanding of the mechanisms of specific spino-pelvic profiles corresponding to diverse pelvic morphology. After gaining an understanding of the original anatomical relationships within the spino-pelvic unit, it is easier to recognize its symptomatic adaptations or painful changes in spino-pelvic sagittal alignment under pathological conditions. Moreover, the effectiveness of such models for predicting lumbar parameters based on the PI contributes to precise and individualized treatment to restore satisfactory spino-pelvic alignment.
Although there are many significant results in this study, some limitations must be discussed. First, an inherent limitation of this study is the sample size, which might lead to selection bias. Therefore, ongoing large-scale and multicentre studies are required to confirm our conclusions. In addition, age is another factor that can influence spino-pelvic alignment, and it has been reported that lumbar alignment changes, such as the loss of LL, can occur with age [25]. It is relatively hard to apply our conclusions to elderly patients, since the average age in the present paper is 48.4 ± 14.9 years. Thus, different conclusions may be drawn for different age groups. Furthermore, authors only research the impacts of PI on lumbar alignment, but sagittal alignment of thoracic or cervical spine may also have influence on the lumbar alignment, which can impact the correlation between LLA and PI. Consequently, sagittal alignment of thoracic or cervical spine is another important factor to be investigated in future studies.
Conclusion
In the present research, the PI had strong correlations with the LLA, LAPL, LL, LLUA and LLLA or SS, which demonstrated that specific lumbar shapes could be determined by the pelvic morphology in asymptomatic adults. Moreover, predictive models for lumbar sagittal parameters on the basis of PI have been provided, which are necessary for surgeons in designing a precise preoperative plan.
References
Blondel B, Schwab F, Ungar B et al (2012) Impact of magnitude and percentage of global sagittal plane correction on health-related quality of life at 2-years follow-up. Neurosurgery 71(2):341–348
Lafage V, Schwab F, Patel A et al (2009) Pelvic tilt and truncal inclination: two key radiographic parameters in the setting of adults with spinal deformity. Spine 34(17):E599–E606
Boulay C, Tardieu C, Hecquet J et al (2006) Sagittal alignment of spine and pelvis regulated by pelvic incidence: standard values and prediction of lordosis. Eur Spine J 15(4):415–422
Schwab F, Lafage V, Patel A et al (2009) Sagittal plane considerations and the pelvis in the adult patient. Spine 34(17):1828–1833
Roussouly P, Pinheiro-Franco JL (2011) Biomechanical analysis of the spino-pelvic organization and adaptation in pathology. Eur Spine J 20(5 Supplement):609–618
Duval-Beaupère G, Schmidt C, Cosson P (1992) A barycentremetric study of the sagittal shape of spine and pelvis: the conditions required for an economic standing position. Ann Biomed Eng 20(4):451–462
Mac-Thiong JM, Berthonnaud E, Dimar JRI et al (2004) Sagittal alignment of the spine and pelvis during growth. Spine 29(15):1642–1647
Rose PS, Bridwell KH, Lenke LG et al (2009) Role of pelvic incidence, thoracic kyphosis, and patient factors on sagittal plane correction following pedicle subtraction osteotomy. Spine 34(8):785–791
Osamu T, Kazuhiro H, Masashi O et al (2018) Lumbar lordosis does not correlate with pelvic incidence in the cases with the lordosis apex located at L3 or above. Eur Spine J. https://doi.org/10.1007/s00586-018-5695-9
Pesenti S, Lafage R, Stein D et al (2018) The amount of proximal lumbar lordosis is related to pelvic incidence. Clin Orthop Relat Res 476(8):1603–1611
Berthonnaud E, Dimnet J, Roussouly P et al (2005) Analysis of the sagittal balance of the spine and pelvis using shape and orientation parameters. J Spinal Disord Tech 18(1):40–47
Roussouly P, Gollogly S, Berthonnaud E et al (2005) Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine 30(3):346–353
Barrett ST, Nikolas M, Reighard FG et al (2018) Relationship between lumbar lordosis and pelvic incidence in the adolescent patient: normal cohort analysis and literature comparison. Spine Deform 6(5):529–536
Hyun SJ, Han S, Kim YB et al (2019) Predictive formula of ideal lumbar lordosis and lower lumbar lordosis determined by individual pelvic incidence in asymptomatic elderly population. Eur Spine J. https://doi.org/10.1007/s00586-019-05955-w
Horton WC, Brown CW, Bridwell KH et al (2005) Is there an optimal patient stance for obtaining a lateral 36” radiograph? Spine 30(4):427–433
Vialle R, Levassor N, Rillardon L et al (2005) Radiographic analysis of the sagittal alignment and balance of the spine in asymptomatic subjects. J Bone Jt Surg 87(2):260
Glassman SD, Berven S, Bridwell K et al (2005) Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine 30(6):682–688
Schwab FJ, Blondel B, Bess S et al (2013) Radiographic spino-pelvic parameters and disability in the setting of adult spinal deformity: a prospective multicenter analysis. Spine 38(13):E803
Hui L, Sibei L, Jiranru W et al (2014) An analysis of spinopelvic sagittal alignment after lumbar lordosis reconstruction for degenerative spinal diseases: how much balance can be obtained? Spine 39(26 Spec No.):B52–B59
Glassman S, Bridwell K, Berven S et al (2005) The impact of positive sagittal balance in adult spinal deformity. Spine 30(18):2024–2029
Legaye J, Duval-Beaupère G (2005) Sagittal plane alignment of the spine and gravity: a radiological and clinical evaluation. Acta Orthop Belg 71(2):213–220
Kim YJ, Bridwell KH, Lenke LG et al (2006) An analysis of sagittal spinal alignment following long adult lumbar instrumentation and fusion to L5 or S1: can we predict ideal lumbar lordosis? Spine 31(20):2343–2352
Cho JH, Joo YS, Lim C et al (2017) Effect of one- or two-level posterior lumbar interbody fusion on global sagittal balance. Spine J 17(12):1794–1802
Lee CH, Chung CK, Jang JS et al (2017) Effectiveness of deformity-correction surgery for primary degenerative sagittal imbalance: a meta-analysis. J Neurosurg Spine 27(5):540–551
Hasegawa K, Okamoto M, Hatsushikano S et al (2016) Normative values of spino-pelvic sagittal alignment, balance, age, and health-related quality of life in a cohort of healthy adult subjects. Eur Spine J 25(11):1–12
Acknowledgements
The authors thank the Department of Imaging in Shandong Provincial Hospital for providing the image data of patients.
Funding
This article did not receive any funding and grants.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
All the authors were consent to the author sequence.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Pan, C., Wang, G. & Sun, J. Correlation between the apex of lumbar lordosis and pelvic incidence in asymptomatic adult. Eur Spine J 29, 420–427 (2020). https://doi.org/10.1007/s00586-019-06183-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-019-06183-y