Abstract
Purpose
The aim of this study is to evaluate the true incidence of all clinical negligence claims against spinal surgery performed by orthopaedic spinal surgeons and neurosurgeons in the National Health Service (NHS) in England, including both open and closed claims.
Methods
This study was a retrospective review of 978 clinical negligence claims held by NHS Resolution against spinal surgery cases identified from claims against ‘Neurosurgery’ and ‘Orthopaedic Surgery’. This category included all emergency, trauma and elective work and all open and closed cases without exclusion between April 2012 and April 2017.
Results
Clinical negligence claims in spinal surgery were estimated to cost £535.5 million over this five-year period. There is a trend of both increasing volume and estimated costs of claims. The most common causes for claims were ‘judgement/timing’ (512 claims, 52.35%), ‘interpretation of results/clinical picture’ (255 claims, 26.07%), ‘unsatisfactory outcome to surgery’ (192 claims, 19.63%), ‘fail to warn/informed consent’ (80 claims, 8.13%) and ‘never events’ including ‘wrong site surgery’ or ‘retained instrument post-operation’ (26 claims, 2.66%). A sub-analysis of 3 years including 574 claims revealed the most prevalent pathologies were iatrogenic nerve damage (132 claims, 23.00%), cauda equina syndrome (CES) (131 claims, 22.82%), inadequate decompression (91 claims, 15.85%), iatrogenic cord damage (72 claims, 12.54%), and infection (51 claims, 8.89%).
Conclusions
The volume and costs of clinical negligence claims is threatening the future of spinal surgery. If spinal surgery is to continue to serve the patients who need it, most thorough investigation, implementation and sharing of lessons learned from litigation claims must be systematically carried out.
Graphical abstract
These slides can be retrieved under Electronic Supplementary Material.

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Since 1995 NHS Resolution (the operating name of the NHS Litigation Authority) has provided schemes to indemnify all NHS hospitals in England. NHS Resolution’s role is to both enable patients who have suffered clinical negligence to be appropriately compensated and to defend claims which are without merit. Since 2002 all claims, without exception, made against NHS hospitals in England have been reported to and handled by NHS Resolution. This centralisation has allowed NHS Resolution to resolve 66% of the cases before court involvement with only 0.7% of all the claims going to a full trial in 2016–2017 [1]. Over a 10-year period (2006–2007 to 2016–2017), the National Audit Office reported the number of claims reported each year had doubled from 5300 to 10,600 and over the same period this had led to a quadrupling of cost from £0.4 to £1.6 billion. The rise in costs was not only related to an increase in claims volume but also a rise in the cost of damages and claimant’s legal costs. In addition recent change to the discount rate, an adjustment of the lump sum awarded to patients to take account of the annual income earned from investing this sum has added an estimated £500 million to the costs of claims against the NHS in 2016–2017 [1].
The increase in litigation sits in the context of a combination of factors including change in society’s perception of the clinician, the more active promotion of legal services and changes in accountability. Chester vs Ashfar (2004) raised the standard of acceptable care and confirmed the responsibilities of the surgeon to provide informed consent [2]. In this case a neurosurgeon, Ashfar failed to consent the claimant for the risk of worsening of her condition following spinal surgery. At trial the judge stated although the procedure had not been carried out negligently, the surgeon had breached his duty of care by failing to warn the patient of the risks. Given the risk profile of the procedures involved, it is unsurprising that surgical specialties are associated with higher rates of litigation [3].
Previous studies have suggested there is a fall in cost and volume of successful spinal surgery claims [4]. However, no study has been able to review the overall incidence of claims in spinal surgery. Given the rise of claims volume and cost seen across the health service, it seems unlikely for the cost and volume of claims against spinal surgery to have fallen. In fact, there is clear evidence to the contrary with the largest UK medical defence organisation making the strategic decision to withdraw cover for spinal surgeons in the private sector. It has estimated medical claims inflation as running at 10% a year and that damages will double in the next seven years [5, 6]. NHS Resolution continues to provide coverage to NHS hospital trusts in the public sector despite the significant costs.
One of the major limitations with previous studies is the difficulty in identifying claims related to spinal surgery. NHS Resolution does not directly code for spinal surgery as a specialty so it is difficult to quantify the accuracy with which claims have been identified. Attempts have been made to overcome this by searching for terms such as ‘spine surgery’ or ‘spine surgeon’. Unfortunately we believe this has led to an underestimation of the litigation burden related to spinal surgery [7]. Furthermore, a rise in volume and cost of claims have been documented in associated specialties such as trauma and orthopaedic surgery which had an increase in claims from 846 to 1474 claims and costs from £41 to £187 million over a 9-year period [8]. In this study, 480 claims were identified as relating to spinal surgery between 2007–2008 and 2011–2012 financial years. However, this does not account for the claims against spinal surgery that would have been attributed to neurosurgery.
This study presents for the first time a complete review of all clinical negligence claims against spinal surgery performed by both orthopaedic spinal surgeons and neurosurgeons in the NHS in England. This is the first study to reflect the true incidence of the problem.
Materials and methods
We made a formal request to obtain all data regarding claims against ‘neurosurgery’ and ‘orthopaedic surgery’ from the NHS Resolution database of NHS trusts in England. This category included all emergency, trauma and elective work and all open and closed cases without exclusion between April 2012 and 2017. The information supplied included: claim status (whether open or closed), incident date, date of notification to NHS Resolution, claim details, the cause of claim as coded by NHS Resolution, the costs incurred for both outstanding and paid damages (including defence costs, claimant costs and total).
Spinal surgery claims were identified from 457 claims against neurosurgery and 7250 claims against orthopaedic surgery by a team of clinicians. Global trends were reviewed for all financial years from 2012/2013 to 2016/2017. In recognition of the generic nature of the cause codes used by NHS Resolution provided under a freedom of information request, a more detailed claim by claim review was carried out for a 3-year period from April 2013 to 2016 using causes specific to spinal surgery. Causes of each claim were determined by the definitions in Table 1. Due to the multifactorial nature of the claims, often more than one cause was attributed to each claim. This has therefore resulted in more causes identified than claims listed. An estimated cost is calculated by the NHS Resolution based on the costs already paid and the outstanding or reserve costs for each claim. This is the most accurate method of estimating claim value for claims that are not closed.
Results
Data obtained from the NHS Resolution show that clinical negligence claims in spinal surgery were estimated to cost between £90.4 and £135.1 million per year over the last 5 years (Table 2). Of these claims 105 claims (10.74%) were closed and the remaining 623 claims (63.70%) were open. Of the closed claims 39 claims (37.14%) were successfully defended without incurring any cost. Legal costs and damages were paid in 66 claims (62.86%) with the mean cost being £3685.52 (£256.50–£38,544.34). It should be noted that as this data represent current claims in the system a minority are closed. In addition, reviewing the cost of claims which have closed sooner creates a bias towards lower value claims. Of the claims still open at the time of this study the cost estimates range from £0 to £7,174,000 per claim. The average estimated cost of claims including both open or closed claims in this data set was £547,645.
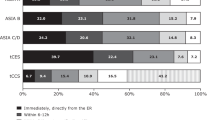
The most common causes for claims were ‘judgement/timing’ (512 claims, 52.35%), ‘interpretation of results/clinical picture’ (255 claims, 26.07%), ‘unsatisfactory outcome to surgery’ (192 claims, 19.63%), ‘fail to warn/informed consent’ (80 claims, 8.13%) and ‘never events’ including ‘wrong site surgery’ or ‘retained instrument post-operation’ (26 claims, 2.66%). The remaining causes are shown in Fig. 1.
A further, more detailed analysis was performed beyond the previous coding used routinely by NHS Resolution to define factors specific to spinal surgery claims for the three-year period (2013/2014–2015/2016). Seven claims were excluded from the initial data set due to re-classification by NHS Resolution leaving 574 claims for further analysis (Fig. 2).
The most prevalent pathologies involved in all claims were iatrogenic nerve damage (132 claims, 23.00%), cauda equina syndrome (CES) (131 claims, 22.82%), inadequate decompression (91 claims, 15.85%), and iatrogenic cord damage (72 claims, 12.54%) and infection (51 claims, 8.89%).
Dividing claims into acute and elective activity, we found there were similar numbers of claims relating to both. One hundred and forty-seven claims (26%) resulted from an acute presentation and 150 claims (26%) related to elective activity. There was insufficient information to classify the remaining claims. In the identified acute cases, the most common pathology was CES (57 claims, 38.00%). Inadequate decompression was alleged in 56 claims (37.33%), with 51 of these relating to CES. Missed fractures were also prevalent (38 claims, 25.33%). Infection, tumour or cancer, and iatrogenic cord injuries were each reported in less than 10% of acute cases. The projected value for all CES-related claims is £68 million in these 3 years, 23.60% the total projected cost for the period. Delay or failure of diagnosis was the most common factor cited (58 claims, 44.27%), followed by delay or failure in treatment (22 claims, 16.79%). Seventeen claims (12.98%) specifically refer to failures in obtaining an MRI scan, and 10 claims (7.63%) detail issues in referral or transfer. The standard of surgical procedures to treat CES was raised in 8 claims (6.11%).
The most common complaints in elective work were unsatisfactory outcome to surgery (105 claims, 71.43%), iatrogenic nerve damage (53 claims, 36.05%), accidental injury (47 claims, 31.97%), postoperative complications (46 claims, 31.29%) and inadequate decompression (26 claims, 17.69%). All cases involved a surgical procedure. Eighty-one claims were each projected to cost in excess of £1 million and accounted for £157 million (54.48%) of the total cost for these 3 years. Reduced mobility was the most common factor amongst these high value claims (45 claims, 56%). Iatrogenic nerve damage (25 claims, 30.86%), infection (15 claims, 18.52%) and CES (11 claims, 13.58%) were the most common underlying pathologies.
Discussion
When we review all spinal surgery claims the year-on-year data indicate that there is a trend of both increasing volume and estimated costs of claims over this 5-year period. The increasing cost is no surprise given the rise across the entire health service due to rising damages and claimant legal costs [9]. However, the continued increase in spinal surgery claims is concerning given context of claim volume plateauing or falling across the NHS as a whole [10]. Every effort must be made by spinal surgeons to learn from clinical negligence claims, to improve the safety and quality of patient care, and to reduce the costs of litigation. Effective learning from claims allows good practice to be shared and has the potential to reduce the number of claims and ensure that resources are not unnecessarily diverted from front line care. Most importantly, this learning means more patients receive the right care first time with fewer failed or ineffective treatments, decreased length of stay and less care packages needed by patients suffering complications.
The impact of informed consent on surgical claims is more significant than the 80 consent-related claims which were directly identified. Lack of fully informed consent has played a role in many of claims which were attributed to ‘unsatisfactory outcome of surgery’ [8]. Many of these claims are clearly avoidable through an adequate consenting process in which an informed patient is involved in a shared decision.
There is concern that in allowing clinicians time for consent clinics they would have less capacity to see newly referred patients and lose the hospital the income which could be achieved by seeing additional patients. The claims data related to consent demonstrates this approach to be a false economy as failure to demonstrate fully informed consent can lead to a more costly claim in the long-term as well as a worse patient experience. For this reason, we would recommend that in elective practice consent occurs 1–6 weeks in advance and not on the day of the day of surgery.
The British Association of Spine Surgeons (BASS) was one of the first national bodies to set out guidance as to how achieve satisfactory consent. The ‘three-legged stool’ model describes three components which are necessary to achieve fully informed consent. All three must be present; as in isolation they are not sufficient. The first leg is the provision of information booklets, written and illustrated at a level that a reasonable patient can comprehend. The second is the ‘patient-centred’ dialogue including the risks of the proposed treatment, about which a reasonable patient, in this patient’s position, would need and want to know. The third leg is specific procedure, and surgeon-guided consent form, along with the NHS or individual hospital form. The surgeon should also gain consent for surgical outcome data to be sent to the national registry [11].
CES remains a significant cause for litigation in spinal surgery, both in terms of cost and claim volume. BASS sets out clear guidelines covering the diagnosis of CES, as well as the provision for timely MRI scan locally and specialist transfer for emergency decompression [12]. This analysis highlights the importance of local adherence to these to avoid the potentially catastrophic permanent loss of function to a patient and the resulting litigation.
It is concerning to note that foreign bodies and instruments have been retained following surgery. In 2012 ‘The Never Events policy framework’ recognised both ‘foreign body left in situ’ and ‘retained instrument post-operation’ in one never-event category called ‘retained foreign object post-operation’ [13]. This re-defined never event includes retention of any items that should be subject to a formal counting/checking process at the commencement of the procedure and a counting/checking process before the procedure is completed (such as swabs, needles, instruments and guide wires). These events along with the other surgical never events of ‘wrong site surgery’ and ‘wrong implant/prosthesis’ represent system failure and are patient safety issues that can be eradicated by more diligent organisation and closer adherence to tools including the World Health Organisation checklist.
It is generally recognised that some of the more common causes of claims are avoidable. Issues around judgement, timing, accidental/iatrogenic injury, inadequate decompression could be deemed to relate to surgical experience and decision-making. There is potentially an opportunity to address these through training. Also, there is some evidence that claims may not be effectively defended because the provider lacks the documentary evidence to demonstrate correct processes have been followed and patient’s interests considered.
The cost estimation supplied by NHS Resolution has the following limitations. In order to make a consistent comparison between (notification) years, data were prepared as it stood on the last day of each financial year. This enabled each reviewed year to contain a similar proportion of estimated costs. This method was chosen as the analysis of claims for all years at one point in time can lead to an undervaluation of costs for recent years in which more claims are open. Total cost estimations for a claim are based on costs paid for claims and reserve or outstanding values calculated by NHS Resolution for open claims. This is the most accurate form of estimation of costs for individual claims in order to make a year-on-year comparison. The method allows us to accurately estimate the claim costs in recent years, but it maybe that the reserve or outstanding values change as more information becomes available about a claim or the claim is resolved.
As part of the ‘Getting It Right First Time’ (GIRFT) programme the senior author has visited every spinal surgical unit in England and found that many clinicians are unaware of the clinical negligence claims in their hospital despite the numbers involved [14]. As a consequence, very few lessons have been learnt from the claims to inform future practice. Further work is needed at both a local and national level to analyse claims to maximise this opportunity to improve patient care. GIRFT has produced a ‘Litigation in Surgical Specialties’ data pack including spinal surgery for each hospital trust in England to ensure clinical staff have the opportunity to learn from claims in conjunction with learning from complaints, severe untoward incidents (SUIs) and inquests. If spinal surgery is to continue to serve the patients who need it most thorough investigation, implementation and sharing of lessons learned from litigation claims must be systematically carried out. This will not only improve patient care but reduce costs both in terms of litigation itself and the management of the resulting complications of potential incidents.
Change history
15 October 2018
Unfortunately, the first author name was incorrectly published in the original publication. The complete correct name is given as below.
15 October 2018
Unfortunately, the first author name was incorrectly published in the original publication. The complete correct name is given as below.
References
House of Commons (2017) Managing the costs of clinical negligence in trusts. Rep Comptrol Audit Gen. https://doi.org/10.12968/bjon.2018.27.2.102
No author listed Opinions of The lords of appeal for judgement in the cause Chester (Respondent) v. Afshar (Apellant): Chester v Afshar. http://www.publications.parliament.uk/pa/ld200304/ldjudgmt/jd041014/cheste-1.htm. Accessed 2 Apr 2018
Taragin MI, Sonnenberg FA, Karns ME et al (1994) Does physician performance explain interspecialty differences in malpractice claim rates? Med Care 32:661–667
Quraishi NA, Hammett TC, Todd DB et al (2012) Malpractice litigation and the spine: the NHS perspective on 235 successful claims in England. Eur Spine J 21:196–199. https://doi.org/10.1007/s00586-012-2203-5
Hawkes N (2017) MDU ceases to cover private spinal surgery. BMJ 357:j2725. https://doi.org/10.1136/bmj.j2725
No author listed MDU—The Campaign. https://www.themdu.com/about-mdu/fair-compensation/the-campaign. Accessed 2 Apr 2018
Quraishi NA, Potter IR (2012) Litigation in spine surgery—analysis of 10 years data from the NHSLA. In: Orthopaedic proceedings. pp 94–B:SUPP_X, 039–039
Machin JT, Briggs TWR (2014) Litigation in trauma and orthopaedic surgery. J Trauma Orthop 02:32–38
Evans C, Labour MP, Flint C, et al (2017) House of commons committee of public accounts managing the costs of clinical negligence in hospital trusts
NHS Resolution (2016) Annual report and accounts 2016/17
Powell JM, Rai A, Foy M et al (2016) The “three-legged stool” a system for spinal informed consent. Bone Jt J 98-B:1427–1430. https://doi.org/10.1302/0301-620x.98b11.37965
Germon T, Ahuja S, Casey ATH et al (2015) British association of Spine surgeons standards of care for cauda equina syndrome. Spine J 15:2S–4S. https://doi.org/10.1016/j.spinee.2015.01.006
NHS England (2015) Revised never events policy and framework
Getting it Right First Time. http://gettingitrightfirsttime.co.uk. Accessed 2 Apr 2018
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Additional information
The original version of this article was revised to update first author name as John T. Machin.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Machin, J.T., Hardman, J., Harrison, W. et al. Can spinal surgery in England be saved from litigation: a review of 978 clinical negligence claims against the NHS. Eur Spine J 27, 2693–2699 (2018). https://doi.org/10.1007/s00586-018-5739-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-018-5739-1