Abstract
Purpose
The interrelations between age-related muscle deterioration (sarcopenia) and vertebral fractures have been suggested based on clinical observations, but the biomechanical relationships have not been explored. The study aim was to investigate the effects of muscle ageing and sarcopenia on muscle recruitment patterns and spinal loads, using musculoskeletal multi-body modelling.
Methods
A generic AnyBody model of the thoracolumbar spine, including > 600 fascicles representing trunk musculature, was used. Several stages of normal ageing and sarcopenia were modelled by reduced strength of erector spinae and multifidus muscles (ageing from 3rd to 6th life decade: ≥ 60% of normal strength; sarcopenia: mild 60%, moderate 48%, severe 36%, very severe 24%), reflecting the reported decrease in cross-sectional area and increased fat infiltration. All other model parameters were kept unchanged. Full-range flexion was simulated using inverse dynamics with muscle optimization to predict spinal loads and muscle recruitment patterns.
Results
The muscle changes due to normal ageing (≥ 60% strength) had a minor effect on predicted loads and provoked only slightly elevated muscle activities. Severe (36%) and very severe (24%) stages of sarcopenia, however, were associated with substantial increases in compression (by up to 36% or 318N) at the levels of the upper thoracic spine (T1T2–T5T6) and shear loading (by up to 75% or 176N) along the whole spine (T1T2–L4L5). The muscle activities increased for almost all muscles, up to 100% of their available strength.
Conclusions
The study highlights the distinct and detrimental consequences of sarcopenia, in contrast to normal ageing, on spinal loading and required muscular effort.
Graphical abstract
These slides can be retrieved under Electronic Supplementary Material.

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vertebral fractures are the most common fractures occurring at older ages [1]. They have a negative impact on the quality of life [2] and are associated with a substantial socioeconomic burden [1]. Furthermore, an initial vertebral fracture significantly increases the risk of future skeletal fractures, in particular in the spine—by a factor of 12.6 [3], which is referred to as “vertebral fracture cascade” [4]. Taking into account that the global population over the age of 60 years will double its 2015 size to reach nearly 2.1 billion by 2050 [5], vertebral fractures become a pressing problem.
The risk of vertebral fracture is in general determined by the mismatch between the load applied on a vertebra and vertebral bone strength, and both can be influenced by the health of trunk muscles [6]. Sarcopenia, an age-related progressive loss of muscle mass and function, affects around 30% of the population over the age of 60 [7] and up to 50% of those aged 80 and above [8]. It has been found to be a risk factor for osteoporotic vertebral fractures [9]. Due to the interrelations between muscle and bone tissues [10, 11], sarcopenia is often accompanied by a lower bone mineral density [12, 13], which correlates with decreased vertebral compressive strength [14]. Furthermore, vertebral loading greatly depends on the forces generated by the muscles; therefore, age-related changes in trunk muscle properties and function are likely to affect the load distribution and orientation in the spine. Stronger back muscles indeed are associated with reduced fracture risk [15], but they deteriorate with age faster than the extremity muscles [16]. The age-related changes include greater fatty infiltration [17, 18] and lower strength of the lumbar extensors [19] but higher levels of trunk muscle co-activation [20]. Finally, the detrimental effect of sarcopenia on trunk muscle endurance, leading to impaired balance [21] and increased risk of falls [22], further contributes to the risk of traumatic overload and fracture.
Despite demonstrated associations between the health of trunk muscles and vertebral fractures [6], the underlying biomechanical relationships have not been explored yet in detail. Trunk muscle deterioration might influence the whole spine biomechanics, leading to overload and fatigue of some muscle groups, as well as vertebral overload and increased risk of fracture. Having insight into these changes may elucidate the role of sarcopenia in the vertebral fracture cascade, which could support prevention and management of vertebral fractures in the elderly.
Therefore, the main objective of this work was to investigate the biomechanical effects of trunk muscle ageing and sarcopenia on muscle recruitment patterns and spinal segmental loads. For this purpose, musculoskeletal multi-body modelling was used, allowing to analyse whole spine biomechanics and the interplay of muscular activity and vertebral loading. This method has been successfully used previously for studying the effects of post-operative changes in paraspinal muscles [23, 24], as well as for the investigation of clinical problems, such as thoracic hyperkyphosis [25], or vertebral fractures [26], and in other contexts [27, 28]. In this study, several stages of normal ageing (from 3rd to 6th life decade) and more pronounced degeneration, regarded clinically as sarcopenia, were simulated by reducing the strength of the most relevant spine extensors: erector spinae and multifidus, assuming their function is critical for adequate spine loading distribution. The strength loss was modelled to reflect the decrease in cross-sectional area and increased fat infiltration reported in the literature. We hypothesized that deterioration of these major trunk muscles requires activation of other muscles with suboptimal lines of action, leading to higher muscle activities and a change in the load orientation and distribution in the spine.
Methods
Thoracolumbar spine model
A generic AnyBody musculoskeletal model of the thoracolumbar spine, representing male anatomy of body height 180 cm and weight 75 kg and validated for sagittal tasks, was used [29, 30]. The model comprises rigid bodies representing the bones of: sacrum and pelvis, 5 lumbar and 12 thoracic vertebrae, 10 pairs of ribs, a sternum and a segment, representing the cervical spine with the skull. The individual vertebrae articulate through spherical joints (joint rotation centres located at the mid-height of the intervertebral disc space and posterior at 38–43% of the discs’ anterior–posterior diameters [31]), with applied stiffness properties, linearly depending on joint rotation [29]. Also, elastic elements were defined to mimic ribcage structures [29] and an intra-abdominal pressure (IAP) model is included in the lumbar region [33, 34]. In this model, intra-abdominal pressure is created by an artificial muscle with a strength equivalent to max. value of 26.6 kPa, as found in the work of [32], that acts on the abdominal volume. This volume is approximated by a cylinder delimited by the transversus muscle and relative position of thorax and pelvis. Thus, IAP is affected by the activation of the transversus muscles and changes in the abdominal volume. (For more model details, please refer to the previous works describing its components: lumbar [33, 35], thoracic [29, 30], cervical [36].)
All major trunk muscle groups are included (i.e. erector spinae, multifidus, semispinalis, quadratus lumborum, psoas major, rectus abdominis, transversus, obliquus internus and externus, levator costarum, subcostalis, transversus thoracis, intercostalis, scalenus and hyoid), represented by over 600 individual fascicles. Each muscle fascicle is modelled as a simple force element, spanning over the shortest path between origin and insertion (approach applied to short muscles, such as semispinalis) or as a via-node type passing through several segments, to account for muscle wrapping (e.g. erector spinae or psoas major). Tendon properties, force-length and force-velocity relationships (thus also any age-related changes affecting them) are neglected, and only muscle strength defines the force-generating capacity of a muscle.
Muscle deterioration modelling
To investigate the influence of muscle ageing and sarcopenia on spinal segmental loads, the strength of the thoracic and lumbar erector spinae (ES) and multifidus (MF) muscles was reduced in the model. The strength of every muscle fascicle is defined by its physiological cross-sectional area (PCSA) multiplied by a coefficient of maximum muscle stress of 90 N/cm2. Various studies reported the force coefficient to be within the range of 34–100 N/cm2, as summarized in [37], but the higher value is preferred to ensure model robustness for simulating various tasks, especially as the sensitivity of spinal load predictions to this parameter was shown to be low [38]. As sarcopenia is manifested by fat infiltration and muscle atrophy, the corresponding PCSA was defined as follows:
To model the effects of ageing from the 2nd to 6th life decade, a detailed dataset regarding properties of both ES and MF assessed in various age groups and at different lumbar spinal levels, reported in a recent imaging-based study [17], was used. As the volume of the lumbar regions of ES and MF was observed not to change significantly with progressing age [17], the corresponding PCSA was reduced only by the reported fat infiltration. In order to account for differences between spinal levels, the path of each fascicle was evaluated and its PCSA reduction was based on the highest fat content observed at the spinal levels over which it spans (strength determined by the weakest region). The muscles of the thoracic region were scaled according to the fat content reported for the L1 level.
For modelling sarcopenia stages, general levels of muscle deterioration proposed in the literature were used to model the strength reduction of ES and MF, as detailed data regarding composition and volume of paraspinal muscles are lacking. The severity of fat infiltration has been typically considered as normal/mild below 10%, slight/moderate for 10–50% and severe for above 50% [39, 40]. Regarding PCSA reduction, a previously mentioned study observed no significant decrease in the volume of ES and MF with age [17], but a 40% decrease in muscle cross-sectional area is possible between 20 and 60 years of age [41]. Based on these data, we defined levels of fat infiltration as 40–60% and PCSA reduction levels as 0, 20 or 40%. From the resulting values of determined relative muscle strength (60%, 48%, 40%, 36%, 32%, 24%), four were selected to represent: mild (60%), moderate (48%), severe (36%) and very severe (24%) stages of sarcopenia. For each condition, all fascicles of the ES and MF were scaled homogenously by the same factor. The simulated degrees of natural ageing and sarcopenia are summarized in Table 1.
No age-related changes, except reduction in muscle cross-sectional area, were modelled. In other words, remaining model parameters such as body weight, height, mass distribution, posture, passive properties of the joints or kinematic patterns were the same for all simulated conditions.
Simulations
Simulated task
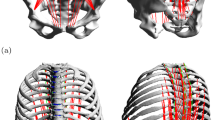
Inverse dynamics simulations of a forward flexion task to the end of range (Fig. 1) were performed, using the AnyBody modelling system [42]. The kinematics of the thoracic and lumbar spinal segments and pelvis flexion with respect to the global reference frame were the same for all simulated conditions. They were prescribed by joint rotation angles over task time, as based on the average spinal segmental motion profile recorded for healthy young subjects. (The measurement methodology and derived motion pattern are presented in detail in [43].)
Selected snapshots of the simulated forward flexion task with indicated corresponding trunk inclination angles (based on the reported measurement from which intervertebral angles and pelvis rotation were derived [43])
Inverse dynamics
Optimization-based inverse dynamics simulations allow to determine muscle and joint reaction forces, by solving a system of Newtonian equations of motion satisfying equilibrium between external and internal forces and moments acting on the represented body segments [44]. The redundancy problem is solved by muscle recruitment optimization scheme, based on some physiological clues [42, 45]. The cost function to be minimized in this problem is a sum of cubed muscle activities (ratios of generated fascicle force to the maximum allowed force that could be produced). Satisfying this criterion is thought to mimic the muscle recruitment by the central nervous system: it minimizes muscles fatigue (by recruiting stronger muscles to generate more force than weaker muscles) while improving muscle synergy (preferring force distribution over a larger number of muscle fascicles). Since the model contains muscles spanning over multiple joints, the muscle optimization can recruit muscles considered antagonists to satisfy equilibrium requirement at all joints [46]. Through the inverse dynamics simulations with the muscle optimization routine, the muscle forces as well as the resulting loads acting on the joints are determined.
Analysed simulation output
With the focus on the risk of vertebral fractures, the maximum compression and shear loads acting on thoracolumbar intervertebral joints (T1T2–L5S1) during the task were analysed for different stages of muscle ageing and sarcopenia. In order to analyse the changes in muscle recruitment, maximum muscle activities as well as task-averaged muscle forces were analysed. The activity of a muscle fascicle is the ratio of the force it generates to its absolute strength (maximum possible force). The activity of a given muscle is defined by the highest activity level of its individual fascicles, which in the context of musculoskeletal simulation predictions can be interpreted as a measure of muscle fatigue. In other words, the overall muscle fatigue is determined by the greatest effort among its fascicles. The total force produced by the muscle (understood as a sum of forces generated by the fascicles) also provides information regarding muscle effort, from an endurance perspective.
With the focus on the risk of vertebral fractures, the maximum compression and shear loads acting on thoracolumbar intervertebral joints (T1T2–L5S1) during the task were analysed for different stages of muscle ageing and sarcopenia. In order to analyse the changes in muscle recruitment, maximum muscle activities as well as task-averaged muscle forces were analysed. The activity of a muscle fascicle is the ratio of the force it generates to its absolute strength (maximum possible force). The activity of a given muscle is defined by the highest activity level of its individual fascicles, which in the context of musculoskeletal simulation predictions can be interpreted as a measure of muscle fatigue. In other words, the overall muscle fatigue is determined by the greatest effort among its fascicles. The total force produced by the muscle (understood as a sum of forces generated by the fascicles) also provides information regarding muscle effort, from an endurance perspective.
Results
Muscle recruitment
Normal ageing
Muscle recruitment patterns were similar to intervertebral joint loading variation for the different stages of normal muscle ageing (Supplementary Material 2, Section 1). A mild to moderate increase in activities of the ES and MF muscles was found, compared to the default model and between different age stages. At the same time, the average forces generated by the ES and thoracic MF were slightly reduced with age. A mild increase in activity and force was predicted for the semispinalis, quadratus lumborum as well as transversus and oblique muscles.
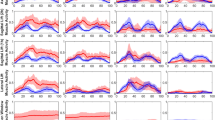
Sarcopenia
Considerable variation in muscle activation and force production were predicted for all sarcopenia stages (Fig. 2). With the weakening of the ES and MF muscles, their activities increased, while the generated forces decreased. Deterioration of these muscles leads to a substantially increased activity and forces of almost all other trunk muscles. For the severe and very severe sarcopenia stages, the simulations predicted several muscles performing at close to or at their maximum capacity.
Muscle activation pattern for the simulated levels of sarcopenia: maximum muscle activities during the analysed tasks and muscle forces averaged over its duration. For definition of these measures, please refer to Methods section: Analysed simulation output. (Note the increasing role of transversus abdominis in supporting the spine through the intra-abdominal pressure; its activation applies forces on the abdominal volume, which consequently applies extending forces on the lumbar spine, making this muscle to act indirectly as a spine extensor)
Spinal segmental loads
Normal ageing
Both the compression and shear loads acting on segments T1T2–L5S1 were almost unaffected by the changes in ES and MF representing ageing from the 3rd through the 6th decade of life (Fig. 3). Minor changes in maximum compression were observed (< 3% or < 35 N increase for the thoracic and < 7% or < 102 N decrease for the lumbar segments) when compared to the default “normal” model. The changes in shear magnitude were also small, below 33 N. (For reference, changes expressed as relative to normal condition are presented in the Supplementary Material 2, Section 2.)
Sarcopenia
Substantial differences in maximum segmental loads were found for the simulated degrees of sarcopenia (Fig. 4). In general, with progressive ES and MF muscle deterioration, there was an increase in maximum compression at thoracic levels (T1T2–T11T12), by up to 318N or 36%. Maximum shear at thoracic and upper lumbar levels (T1T2–L1L2) increased by up to 176N or 60%. The greatest differences were seen at the upper thorax (T1T2–T5T6) for severe and very severe stages of sarcopenia.
Discussion
The age-related deterioration of trunk musculature has been suggested to be an important factor in vertebral fracture formation and subsequent cascade. The back muscles support the spinal column to maintain optimal posture and provide mobility, generating most of the loading acting on the vertebra. Therefore, their loss of function may increase vertebral fracture risk directly by segmental overload or indirectly by affecting balance. Nevertheless, to date these effects have not been evaluated from a biomechanical perspective. In this work, we investigated the biomechanics of the entire thoracolumbar spine associated with stages of trunk muscle ageing and sarcopenia, simulated as the strength reduction, using an established musculoskeletal model [29]. The resulting estimates of spinal segmental loads and muscle activation patterns cast light on the biomechanical consequences of degenerated spine extensors, especially for the risk of vertebral fractures or spinal instability caused by muscular fatigue.
The simulations predicted similar loads and only slightly elevated muscle forces for various stages of healthy ageing up to 60 years of age. Decreased function of erector spinae and multifidus muscles due to age-related fat infiltration was efficiently compensated for by other muscles, without major changes in spinal load distribution. Simulations of sarcopenia, however, revealed that more severe reduction in ES and MF strength requires elevated activity of almost all other muscles—this expected result provides an intuitive explanation for muscular fatigue in sarcopenia patients. Increased muscle co-contraction was previously observed in the elderly subjects [47] and in the patients with vertebral fractures [48], and it has been suggested to compromise spinal balance as well as increase spinal loads. In agreement with previously reported measurements [47], our study did predict increased activity in both spine flexors and extensors (hence co-contraction), but it might be overestimated because the abdominal muscles were not affected by age-related changes in our model. Increased compression at the upper thoracic spine levels, predicted in this study, might contribute to compressive fractures in this area. Moreover, elevated shear along the whole spinal column profoundly alters the predicted load direction at thoracolumbar and lower thoracic levels (due to shear/compression imbalance), and the failure strength of the vertebrae is significantly reduced under off-axis loading [49].
The results of this study are limited by the shortcomings of the applied model. One of the limitations is that passive muscle properties and force-length relationships are disregarded. Modelling muscles as simple force actuators neglects the decreasing force generation capacity due to elongation, tendon contribution and the effects of flexion-relaxation phenomenon. Predicted muscle activation levels and forces are likely overestimated, especially at large degree flexion. The magnitude of this inaccuracy may differ between simulated conditions, as tendon mechanical properties change with older age and sarcopenia [41, 50]. This constitutes a major limitation to the study findings, which necessitates future experimental work focused on characterization of trunk muscle-tendon ageing, as the scarce data reported to date are somewhat conflicting and limited to lower limbs and selected age groups only [50].
Also, the predictions of high activities of the transverse abdominis muscles might be exaggerated due to the role of applied intra-abdominal pressure (IAP) model. The IAP is generated by the transversus muscles acting on the abdominal volume; in other words, the greater transversus activity–the greater IAP and extending forces applied to the spine. Since transversus effectively acts as a spine extensor, it is recruited by the optimization algorithm to support function of the deteriorated extensors. However, this might be an artefact related to applying normal IAP model in sarcopenia simulations. On the other hand, related IAP values reaching up to 8 kPa predicted for very severe sarcopenia, although greater than for normal condition (max. 3 kPa), are still within reported ranges for daily activities [51]. The IAP was shown to have stabilizing and unloading effect on the spine [34, 51] by relieving extensors [52, 53], but its role in the context of sarcopenia should be elucidated in the further research. Future experimental studies could also support evaluation of the model validity for simulating sarcopenia cases, which in this work has been inferred from prior validation performed for healthy spine biomechanics [29].
The simplifications assumed in representation of trunk muscle ageing are also a source of study limitations. As a preliminary model of sarcopenia, only the strength of major spine extensors, ES and MF, was scaled, although some studies suggest that also other trunk muscles might be affected by degenerative changes. While fat infiltration does not significantly change with age for the psoas major [18], it does seem to affect abdominal muscles, such as the rector abdominis or internus and externus oblique [54]. Trunk muscle size appears to in general decrease with progressing age [55], but the specific effects of ageing or sarcopenia on morphology of various trunk muscles have not been reported; therefore, they were neglected in this study. For the same reason (insufficient data), the properties of the thoracic ES and MF were assumed to be the same as in the upper lumbar spine, the modelling of sarcopenia stages was based on somewhat arbitrary definition of severity degrees and disregarded level-dependency and differences between the ES and MF muscles. As the ES and MF are the largest spine extensors, they play a major role in overall spine biomechanics. However, the effect of their deterioration on spinal loads might be enhanced or perhaps hindered by degeneration of other muscle groups. Recent advances in medical image segmentation and analysis methods [56, 57] should encourage further imaging studies of sarcopenia, providing more detailed characterization of trunk muscles properties in the future (including multiple muscle groups and spinal regions, assessed in patients presenting various severity levels of sarcopenia). Such comprehensive datasets are necessary for overcoming the limitations of the current study and pursuing more sophisticated investigations of biomechanical implications of sarcopenia.
Another important limitation of this study arises from modelling the muscle strength loss based solely on the reduction of PCSA and fatty infiltration and assuming a linear relationship between muscle size/composition and its force-generating capacity [58]. Besides muscle composition, sarcopenia induces changes in muscle contractile properties and tendon stiffness [41], metabolism and neural activation [59] as well as muscle fibre type [59] and angles [19]. All these changes might affect muscle force generation, reflex and latency, and consequently activation patterns but were not represented in our model due to insufficient data and technical restrictions of musculoskeletal modelling. In the future, cross-disciplinary projects should be pursued to collect complete data on various sarcopenia-related changes and to develop more complex multi-scale models, which would allow to capture these changes and predict their impact on spine biomechanics.
Also, the age-related changes in spinal posture and kinematics that affect spinal loads [25, 60, 61] and might coincide with sarcopenia have not been considered. As the increase in the upper thoracic loads simulated for sarcopenia began at a relatively high forward trunk lean angle of about 60° (Supplementary Material 2, Section 4), it is also debatable whether or not such a trunk flexion would be attempted by sarcopenia patients. The increase in muscle activation, on the other hand, occurred already very early during the execution of the task—(Supplementary Material 2, Section 5)—and lasted throughout the task, which implies a profound effect of sarcopenia on muscle fatigue, hence spinal stability and balance.
In conclusion, the effects of sarcopenia on spinal biomechanics have been evaluated, suggesting a possible role of age-related muscle deterioration on vertebral fracture risk. The weakening of major spine extensors, typical for changes until 60 years of age, was predicted to be compensated for by the action of other muscles, without a substantial effect on spinal loads. More substantial deterioration, associated with severe to very severe stages of sarcopenia, profoundly altered muscle activation levels and loading conditions of the spine.
References
Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A (2007) Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J Bone Miner Res 22(3):465–475. https://doi.org/10.1359/jbmr.061113
Ross PD (1997) Clinical consequences of vertebral fractures. Am J Med 103(2):S30–S43. https://doi.org/10.1016/S0002-9343(97)90025-5
Melton LJ III, Atkinson EJ, Cooper C, O’Fallon WM, Riggs BL (1999) Vertebral fractures predict subsequent fractures. Osteoporos Int 10(3):214–221. https://doi.org/10.1007/s001980050218
Briggs AM, Greig AM, Wark JD (2007) The vertebral fracture cascade in osteoporosis: a review of aetiopathogenesis. Osteoporos Int 18(5):575–584. https://doi.org/10.1007/s00198-006-0304-x
World Population Ageing (2015). United Nations. Department of Economic and Social Affairs / Population Division: New York
Mokhtarzadeh H, Anderson DE (2016) The role of trunk musculature in osteoporotic vertebral fractures: implications for prediction, prevention, and management. Curr Osteoporos Rep 14(3):67–76. https://doi.org/10.1007/s11914-016-0305-4
Doherty TJ (2003) Invited review: aging and sarcopenia. J Appl Physiol 95(4):1717–1727. https://doi.org/10.1152/japplphysiol.00347.2003
von Haehling S, Morley JE, Anker SD (2010) An overview of sarcopenia: facts and numbers on prevalence and clinical impact. J Cachexia, Sarcopenia Muscle 1(2):129–133. https://doi.org/10.1007/s13539-010-0014-2
Hida T, Shimokata H, Sakai Y, Ito S, Matsui Y, Takemura M, Kasai T, Ishiguro N, Harada A (2016) Sarcopenia and sarcopenic leg as potential risk factors for acute osteoporotic vertebral fracture among older women. Eur Spine J 25(11):3424–3431. https://doi.org/10.1007/s00586-015-3805-5
Tagliaferri C, Wittrant Y, Davicco MJ, Walrand S, Coxam V (2015) Muscle and bone, two interconnected tissues. Ageing Res Rev 21:55–70. https://doi.org/10.1016/j.arr.2015.03.002
Edwards MH, Dennison EM, Aihie Sayer A, Fielding R, Cooper C (2015) Osteoporosis and sarcopenia in older age. Bone 80:126–130. https://doi.org/10.1016/j.bone.2015.04.016
Verschueren S, Gielen E, O’Neill TW, Pye SR, Adams JE, Ward KA, Wu FC, Szulc P, Laurent M, Claessens F, Vanderschueren D, Boonen S (2013) Sarcopenia and its relationship with bone mineral density in middle-aged and elderly European men. Osteoporos Int 24(1):87–98. https://doi.org/10.1007/s00198-012-2057-z
Wu CH, Yang KC, Chang HH, Yen JF, Tsai KS, Huang KC (2013) Sarcopenia is related to increased risk for low bone mineral density. J Clin Densitom 16(1):98–103. https://doi.org/10.1016/j.jocd.2012.07.010
Singer K, Edmondston S, Day R, Breidahl P, Price R (1995) Prediction of thoracic and lumbar vertebral body compressive strength: correlations with bone mineral density and vertebral region. Bone 17(2):167–174. https://doi.org/10.1016/S8756-3282(95)00165-4
Sinaki M, Itoi E, Wahner HW, Wollan P, Gelzcer R, Mullan BP, Collins DA, Hodgson SF (2002) Stronger back muscles reduce the incidence of vertebral fractures: a prospective 10 year follow-up of postmenopausal women. Bone 30(6):836–841
Dahlqvist J, Vissing C, Hedermann G, Thomsen C, Vissing J (2015) Paraspinal fat infiltration in healthy adults with aging. Neuromuscul Disord 25:S273. https://doi.org/10.1016/j.nmd.2015.06.314
Crawford RJ, Filli L, Elliott JM, Nanz D, Fischer MA, Marcon M, Ulbrich EJ (2016) Age- and level-dependence of fatty infiltration in lumbar paravertebral muscles of healthy volunteers. AJNR Am J Neuroradiol 37(4):742–748. https://doi.org/10.3174/ajnr.A4596
Lee SH, Park SW, Kim YB, Nam TK, Lee YS (2016) The fatty degeneration of lumbar paraspinal muscles on computed tomography scan according to age and disc level. Spine J. https://doi.org/10.1016/j.spinee.2016.08.001
Singh DK, Bailey M, Lee RY (2011) Ageing modifies the fibre angle and biomechanical function of the lumbar extensor muscles. Clin Biomech (Bristol, Avon) 26(6):543–547. https://doi.org/10.1016/j.clinbiomech.2011.02.002
Quirk DA, Hubley-Kozey CL (2014) Age-related changes in trunk neuromuscular activation patterns during a controlled functional transfer task include amplitude and temporal synergies. Hum Mov Sci 38:262–280. https://doi.org/10.1016/j.humov.2014.08.013
Helbostad JL, Sturnieks DL, Menant J, Delbaere K, Lord SR, Pijnappels M (2010) Consequences of lower extremity and trunk muscle fatigue on balance and functional tasks in older people: a systematic literature review. BMC Geriatr 10:56. https://doi.org/10.1186/1471-2318-10-56
Landi F, Liperoti R, Russo A, Giovannini S, Tosato M, Capoluongo E, Bernabei R, Onder G (2012) Sarcopenia as a risk factor for falls in elderly individuals: results from the ilSIRENTE study. Clin Nutr 31(5):652–658. https://doi.org/10.1016/j.clnu.2012.02.007
Jamshidnejad S, Arjmand N (2015) Variations in trunk muscle activities and spinal loads following posterior lumbar surgery: a combined in vivo and modeling investigation. Clin Biomech (Bristol, Avon) 30(10):1036–1042. https://doi.org/10.1016/j.clinbiomech.2015.09.010
Malakoutian M, Street J, Wilke H-J, Stavness I, Dvorak M, Fels S, Oxland T (2016) Role of muscle damage on loading at the level adjacent to a lumbar spine fusion: a biomechanical analysis. Eur Spine J 25(9):2929–2937. https://doi.org/10.1007/s00586-016-4686-y
Briggs AM, van Dieen JH, Wrigley TV, Greig AM, Phillips B, Lo SK, Bennell KL (2007) Thoracic kyphosis affects spinal loads and trunk muscle force. Phys Ther 87(5):595–607. https://doi.org/10.2522/ptj.20060119
Briggs AM, Wrigley TV, van Dieen JH, Phillips B, Lo SK, Greig AM, Bennell KL (2006) The effect of osteoporotic vertebral fracture on predicted spinal loads in vivo. Eur Spine J 15(12):1785–1795. https://doi.org/10.1007/s00586-006-0158-0
Rasmussen J, Tørholm S, de Zee M (2009) Computational analysis of the influence of seat pan inclination and friction on muscle activity and spinal joint forces. Int J Ind Ergon 39(1):52–57. https://doi.org/10.1016/j.ergon.2008.07.008
Han KS, Rohlmann A, Zander T, Taylor WR (2013) Lumbar spinal loads vary with body height and weight. Med Eng Phys 35(7):969–977. https://doi.org/10.1016/j.medengphy.2012.09.009
Ignasiak D, Dendorfer S, Ferguson SJ (2016) Thoracolumbar spine model with articulated ribcage for the prediction of dynamic spinal loading. J Biomech 49(6):959–966. https://doi.org/10.1016/j.jbiomech.2015.10.010
Ignasiak D, Ferguson SJ, Arjmand N (2016) A rigid thorax assumption affects model loading predictions at the upper but not lower lumbar levels. J Biomech 49(13):3074–3078. https://doi.org/10.1016/j.jbiomech.2016.07.006
Pearcy MJ, Bogduk N (1988) Instantaneous axes of rotation of the lumbar intervertebral joints. Spine 13(9):1033–1041
Essendrop M (2003) Significance of intra-abdominal pressure in work related trunk loading. National Institute of Occupational Health, Denmark
Han KS, Zander T, Taylor WR, Rohlmann A (2012) An enhanced and validated generic thoraco-lumbar spine model for prediction of muscle forces. Med Eng Phys 34(6):709–716. https://doi.org/10.1016/j.medengphy.2011.09.014
Arshad R, Zander T, Dreischarf M, Schmidt H (2016) Influence of lumbar spine rhythms and intra-abdominal pressure on spinal loads and trunk muscle forces during upper body inclination. Med Eng Phys 38(4):333–338. https://doi.org/10.1016/j.medengphy.2016.01.013
de Zee M, Hansen L, Wong C, Rasmussen J, Simonsen EB (2007) A generic detailed rigid-body lumbar spine model. J Biomech 40(6):1219–1227. https://doi.org/10.1016/j.jbiomech.2006.05.030
de Zee M, Falla D, Farina D, Rasmussen J (2007) A detailed rigid-body cervical spine model based on inverse dynamics. J Biomech 40:S284. https://doi.org/10.1016/S0021-9290(07)70280-4
Christophy M, Faruk Senan NA, Lotz JC, O’Reilly OM (2012) A musculoskeletal model for the lumbar spine. Biomech Model Mechanobiol 11(1–2):19–34. https://doi.org/10.1007/s10237-011-0290-6
Bruno AG, Bouxsein ML, Anderson DE (2015) Development and validation of a musculoskeletal model of the fully articulated thoracolumbar spine and rib cage. J Biomech Eng 137(8):081003. https://doi.org/10.1115/1.4030408
Kang CH, Shin MJ, Kim SM, Lee SH, Lee CS (2007) MRI of paraspinal muscles in lumbar degenerative kyphosis patients and control patients with chronic low back pain. Clin Radiol 62(5):479–486. https://doi.org/10.1016/j.crad.2006.12.002
Kjaer P, Bendix T, Sorensen JS, Korsholm L, Leboeuf-Yde C (2007) Are MRI-defined fat infiltrations in the multifidus muscles associated with low back pain? BMC Med 5:2. https://doi.org/10.1186/1741-7015-5-2
Lang T, Streeper T, Cawthon P, Baldwin K, Taaffe DR, Harris TB (2010) Sarcopenia: etiology, clinical consequences, intervention, and assessment. Osteoporos Int 21(4):543–559. https://doi.org/10.1007/s00198-009-1059-y
Damsgaard M, Rasmussen J, Christensen ST, Surma E, de Zee M (2006) Analysis of musculoskeletal systems in the anybody modeling system. Simul Model Pract Theory 14(8):1100–1111. https://doi.org/10.1016/j.simpat.2006.09.001
Ignasiak D, Rueger A, Ferguson SJ (2017) Multi-segmental thoracic spine kinematics measured dynamically in the young and elderly during flexion. Hum Mov Sci 54:230–239. https://doi.org/10.1016/j.humov.2017.05.011
Erdemir A, McLean S, Herzog W, van den Bogert AJ (2007) Model-based estimation of muscle forces exerted during movements (Bristol, Avon). Clin Biomech 22(2):131–154. https://doi.org/10.1016/j.clinbiomech.2006.09.005
Rasmussen J, Damsgaard M, Voigt M (2001) Muscle recruitment by the min/max criterion—a comparative numerical study. J Biomech 34(3):409–415
Stokes IA, Gardner-Morse M (1995) Lumbar spine maximum efforts and muscle recruitment patterns predicted by a model with multijoint muscles and joints with stiffness. J Biomech 28(2):173–186
McGill SM, Yingling VR, Peach JP (1999) Three-dimensional kinematics and trunk muscle myoelectric activity in the elderly spine—a database compared to young people. Clin Biomech (Bristol, Avon) 14(6):389–395
Greig AM, Briggs AM, Bennell KL, Hodges PW (2014) Trunk muscle activity is modified in osteoporotic vertebral fracture and thoracic kyphosis with potential consequences for vertebral health. PLoS ONE 9(10):e109515. https://doi.org/10.1371/journal.pone.0109515
Aquarius R, Homminga J, Verdonschot N, Tanck E (2011) The fracture risk of adjacent vertebrae is increased by the changed loading direction after a wedge fracture. Spine 36(6):408–412. https://doi.org/10.1097/BRS.0b013e3181f0f726
Narici MV, Maffulli N, Maganaris CN (2008) Ageing of human muscles and tendons. Disabil Rehabil 30(20–22):1548–1554. https://doi.org/10.1080/09638280701831058
Arjmand N, Shirazi-Adl A (2006) Role of intra-abdominal pressure in the unloading and stabilization of the human spine during static lifting tasks. Eur Spine J 15(8):1265–1275. https://doi.org/10.1007/s00586-005-0012-9
Cholewicki J, Juluru K, McGill SM (1999) Intra-abdominal pressure mechanism for stabilizing the lumbar spine. J Biomech 32(1):13–17
Stokes IA, Gardner-Morse MG, Henry SM (2010) Intra-abdominal pressure and abdominal wall muscular function: spinal unloading mechanism. Clin Biomech (Bristol, Avon) 25(9):859–866. https://doi.org/10.1016/j.clinbiomech.2010.06.018
Cuellar WA, Wilson A, Blizzard CL, Otahal P, Callisaya ML, Jones G, Hides JA, Winzenberg TM (2016) The assessment of abdominal and multifidus muscles and their role in physical function in older adults: a systematic review. Physiotherapy. https://doi.org/10.1016/j.physio.2016.06.001
Anderson DE, D’Agostino JM, Bruno AG, Manoharan RK, Bouxsein ML (2012) Regressions for estimating muscle parameters in the thoracic and lumbar trunk for use in musculoskeletal modeling. J Biomech 45(1):66–75. https://doi.org/10.1016/j.jbiomech.2011.10.004
Valenzuela W, Ferguson SJ, Ignasiak D, Diserens G, Hani L, Wiest R, Vermathen P, Boesch C, Reyes M (2016) FISICO: fast image segmentation correction. PLoS ONE 11(5):1–17. https://doi.org/10.1371/journal.pone.0156035
Valenzuela W, Vermathen P, Boesch C, Nolte LP, Reyes M (2013) iSix - Image Segmentation in Osirix. In: Paper presented at the 30th Annual Scientific Meeting of the European Society for Magnetic Resonance in Medicine and Biology: Toulouse, October 3–5
Maughan RJ, Watson JS, Weir J (1983) Strength and cross-sectional area of human skeletal muscle. J Physiol 338:37–49
McGregor RA, Cameron-Smith D, Poppitt SD (2014) It is not just muscle mass: a review of muscle quality, composition and metabolism during ageing as determinants of muscle function and mobility in later life. Longev Healthspan 3:9. https://doi.org/10.1186/2046-2395-3-9
Bruno AG, Anderson DE, D’Agostino J, Bouxsein ML (2012) The effect of thoracic kyphosis and sagittal plane alignment on vertebral compressive loading. J Bone Miner Res 27(10):2144–2151. https://doi.org/10.1002/jbmr.1658
Ignasiak D, Rueger A, Sperr R, Ferguson SJ (2017) Thoracolumbar spine loading associated with kinematics of the young and the elderly during activities of daily living. J Biomech 70:175–184. https://doi.org/10.1016/j.jbiomech.2017.11.033
Acknowledgements
This study was funded by a research grant from AOSpine International, Switzerland (Project CPP FFOB_OC_14).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dominika Ignasiak, Waldo Valenzuela, Mauricio Reyes, and Stephen J. Ferguson declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ignasiak, D., Valenzuela, W., Reyes, M. et al. The effect of muscle ageing and sarcopenia on spinal segmental loads. Eur Spine J 27, 2650–2659 (2018). https://doi.org/10.1007/s00586-018-5729-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-018-5729-3