Abstract
Purpose
To test the reliability and validity of the multi-positional magnetic resonance imaging (MRI) in measuring cervical angular parameter using the standard dynamic cervical X-ray as a reference.
Methods
All patients who underwent both cervical dynamic plain radiograph and multi-positional MRI on the same day between 2010 and 2016 were included in this study. The C2–7 angle and the segmental angles of the C2–3 to C6–7 segments were measured in all three positions (neutral, flexion, and extension) using multi-positional MRI and dynamic radiograph. The Pearson’s correlation coefficients and linear regression analysis were used for statistical analysis.
Results
46 patients were enrolled in this study. All angular parameters showed significant positive correlation between multi-positional MRI and dynamic X-ray (p < 0.05). The angle of C2–7 showed significantly positive correlation between multi-positional MRI and X-ray (r = 0.552–0.756). All segmental angles from C2–3 to C6–7 showed moderate correlation (r = 0.401–0.636). The linear regression analysis showed that C2–7 angles and all angular parameters had significant correlation between multi-positional MRI and dynamic X-ray (p < 0.05, R 2 = 0.107–0.571).
Conclusions
The C2–7 angle and segmental cervical angles measured by multi-positional MRI were valid, and reliability substituted the dynamic X-ray measurement within the acceptable range of error. Multi-positional MRI can be used as a reliable tool for angular parameter measurement and detection of angular instability in the cervical spine.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Dynamic plain radiograph is one of the most important tools used to evaluate angular cervical instability in degenerative disease and following spinal trauma. Using this imaging modality, cervical spine instability can be diagnosed by identifying segmental rotation in the sagittal plain of more than 11° [1, 2]. Although dynamic cervical radiograph is the gold standard for angle measurement, it comes with inherent risks and limitations.
Plain radiographs are inexpensive, fast, and provide consistent, quality images of bony structures. However, they are limited by the fact that they are only two dimensional and cannot be used to analyze soft tissue structures. Furthermore, obtaining multiple plain radiographs of the head and cervical spine exposes patients to harmful ionizing radiation [3, 4]. While the risk associated with a single series of plain radiographs is low, the average annual rate of exposure to ionizing radiation has increased over the past 45 years and continues to climb. It is important to consider lifetime exposure, especially in high-risk populations such as children, pregnant women, and individuals with chronic diseases who require repeated radiographic evaluation, where ionizing radiation is potentially more harmful than in the general population [3]. While the assumed risk of exposure is often justified by the medical benefit of the study, it is important to reduce exposure by choosing safer, non-radiating imaging modalities whenever possible.
Magnetic resonance imaging (MRI) is an imaging modality frequently to evaluate cervical spine pathology, and does not expose the patient to any ionizing radiation [5, 6]. In addition to a lack of ionizing radiation, it offers multiple other advantages to plain radiograph including multi-planar capability and excellent soft tissue contrast. Multi-positional magnetic resonance imaging (multi-positional MRI) offers additional benefits including multi-positional evaluation and the ability to take weight-bearing images [7, 8]. Given these capabilities, multi-positional MRI has been shown to be a valuable imaging modality for the diagnosis, evaluation, and management of degenerative vertebral disease and spinal injury. Because multi-positional MRI can accurately identify bony and soft tissue structures in the spine as well as evaluate multiple types of spinal pathology, it is a powerful tool for investigating the relationship between pathological changes and cervical vertebral motion. Previous studies have used multi-positional MRI to successfully show decreased cervical vertebrae mobility to be correlated with disc degeneration, cord compression, and sagittal misalignment of the cervical spine [7,8,9]. While previous studies have shown multi-positional MRI to be a promising tool for evaluating cervical spine pathology, the use of multi-positional MRI is expensive relative to radiographs and there are limited spine or imaging center which are capable of performing multi-positional MRI studies. The limited access to multi-positional MRI leads us to conduct this study. We want to know if the angle measurement in cervical dynamic plain radiograph can be used as a reliable, valid substitute for the angle measurement in cervical multi-positional MRI. To do this, we measured angular parameters in cervical spine in neutral, flexion, and extension position using both multi-positional MRI dynamic plain radiograph and compared the measurements between two modalities. If the two measurements are shown to be equivalent, then the measured angle from dynamic plain radiograph can be used as a predictor for the significant findings which had been found in the previous multi-positional MRI studies. Furthermore, if measurements using both modalities are equivalent, then multi-positional MRI sagittal segmental rotation measurement values can be used to diagnose cervical spine radiographic instability for which plain radiographs are currently the gold standard. This will allow for the safe evaluation and diagnosis of cervical spine instability in populations at high risk for developing complications from ionized radiation.
Materials and methods
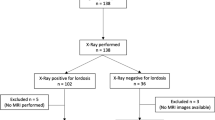
Patients who received both dynamic plain radiograph and multi-positional MRI of the cervical spine in the same setting (same day) from January 2010 to December 2016 were enrolled in the study. To be included in the study, the lower endplate of C7 had to be clearly identifiable in both plain radiograph and multi-positional MRI images in all three studied positions (flexion, neutral, and extension) and all images from a single patient had to have good image quality. Patients with cervical spine deformity (more than 10° in sagittal, coronal, and frontal plane), inflammatory diseases of the spine, congenital anomaly, cervical spine infection, cervical spine tumor, and previous cervical spine surgery were excluded from the study. We also excluded patients whose MR images had an artifact, which obscured the exact angle measurement on both dynamic plain radiograph and MRI. After all inclusion and exclusion criteria were met, 46 patients were included in this study. For all patients, measurements of the C2–7 angle, C2–3 angle, and subaxial segmental angles (C3–4, C4–5, C5–6, and C6–7) were taken using both dynamic plain radiograph and multi-positional MRI in all three positions (neutral, flexion, and extension).
Multi-positional magnetic resonance imaging (multi-positional MRI) and dynamic plain radiograph
Multi-positional MRI of the cervical spine was performed using a 0.6 Tesla MRI scanner (Upright Multi-Position, Fornar Corp., New York, NY, USA). The MR unit uses two electro magnets to produce a horizontal magnetic field allowing imaging in the upright position, and also the use of both solenoidal and planar receiver coils, allowing patients to be scanned in weight-bearing positions. The image protocol included T1- and T2-weighted sagittal fast spin-echo images that were obtained using a flexible surface coil with the patient seated in upright weight-bearing neutral (0°), flexion (40°) and extension (−20°) positions. The following parameters were used: T1-weighted sagittal spin echo images (repetition time 671 ms, echo time 17 ms, thickness 4.0 mm, field of view 30 cm, matrix 256 × 224, number of excitations 2) and T2-weighted fast spin echo images (repetition time 3000 ms, echo time 140 ms, thickness 4.0 mm, field of view 30 cm, matrix 256 × 224, number of excitations 2).
The angle in flexion, neutral, and extension position in dynamic plain radiograph were similar to the multi-positional MRI angles. Three positions on dynamic plain radiographs and multi-positional MRIs were adjusted by a radiological technician who took both the dynamic plain radiograph and multi-positional MRI for each patient in the same setting.
Images were viewed using the eRAD PACS system (version 7.2.38.0, SC, USA).
Angular parameters measurement
The C2–7 angle (cervical lordotic measurement) was measured as the angle between the tangent lines of the lower endplates of the axis and C7 (Fig. 1). The positive value was the kyphotic alignment and the negative value was the lordotic alignment. The C2–3 angle (C2–3 segmental angle) was defined as the angle between the tangent lines of the lower endplate of the axis and the tangent lines of the lower endplates of C3 (Fig. 2). The subaxial segmental angles (C3–4, C4–5, C5–6, and C6–7) (segmental angle) were measured as the angle between the tangent lines of the upper endplates of the cephalad cervical spine and the tangent lines of the lower endplates of the caudad cervical spine (Fig. 2). All multi-positional MRI angle measurement used the mid-sagittal image in each position.
Statistical analysis
Angular parameters (C2–7 angle and subaxial angles) on the dynamic plain radiographs and multi-positional MRI images were carefully evaluated independently by three spine surgeons. The intraclass correlation coefficients (ICCs) were used to analyze intra- and inter-observer reliability. Pearson correlation was used to evaluate the correlation between dynamic plain radiograph and multi-positional MRI in each parameter. A Pearson correlation coefficient (r) of 0.00–0.19 was considered very weak correlation, r of 0.20–0.39 was considered weak correlation, r of 0.40–0.59 was considered moderate correlation, r of 0.60–0.79 was considered strong correlation, and r of 0.80–1.0 was considered very strong correlation [10]. Linear regression analysis was used to confirm the correlations. For statistical analysis, SPSS 23.0 (Chicago, IL, USA) was used; a p value of less than 0.05 was considered a statistically significant finding.
To test the correlation between two dependent groups, the sample size of 27 in each group was determined using the effect size of 0.278 (calculated by the difference between mean and standard deviation of C2–7 angle in neutral position in both groups), α value of 0.05, and β value of 0.20.
Results
Forty-six patients (25 male and 21 female, ages 45.41 ± 9.32 years old) were enrolled in the study after being carefully evaluated using the previously outlined inclusion and exclusion criteria. The ICCs of intra- and inter-observer between three spine observers showed excellent reliability in all measured parameters; the ICCs were 0.762–0.968.
The Pearson correlation coefficient results showed statistically significant positive correlation between dynamic plain radiograph and multi-positional MRI for all parameters and in all three positions (p < 0.05). The C2–7 angle showed strong correlation in the neutral position (r = 0.756) and moderate correlation in flexion and extension (r = 0.552, and 0.558, respectively). For the subaxial cervical segmental angle, the Pearson correlation coefficient showed moderate and strong correlation between the two imaging modalities. In the neutral position, the segmental angle of the subaxial segments showed strong correlation (r of more than 0.6) at every segment except the C6–7 segment which showed moderate correlation (Table 1).
Linear regression analysis also showed statistical significant correlation between dynamic plain radiograph and multi-positional MRI. R 2 results are shown in Table 1.
Discussion
Our results showed significantly moderate to strong positive correlations of all angular parameters between the cervical spine multi-positional MRI and cervical spine dynamic plain radiograph. Our study also found excellent intra- and inter-observer reliability for all angular parameters measured in both multi-positional MRI images and dynamic radiographs. These findings suggest that the two modalities can be used interchangeably.
While dynamic plain radiographs were mainly used for diagnosis of cervical angular instability [11, 12], MRI of the cervical spine can provide superior evaluation of disc degeneration, soft tissue pathology, for example ligamentous injury, and the spinal canal [13, 14]. Previous studies have evaluated the angular parameters of the cervical spine using either dynamic plain radiograph or multi-positional MRI but not using both. Studies using plain radiographs have primarily focused on stability evaluation [2, 15,16,17,18]. Conversely, most of the cervical spine multi-positional MRI studies have mainly focused on correlation between angular parameters and significant soft tissue pathologies such as disc degeneration, space available for cord, and ligamentum flavum [9]. Our study was the first to compare the two imaging modalities in the evaluation of cervical segment angulation, in order to understand whether the cervical segmental angular information obtained from multi-positional MRI and dynamic plain radiograph can reliably substitute each other. Our data show the measurements from the two modalities to be interchangeable, which suggests that plain radiographs can reliably detect the presence of significant soft tissue pathology, and that multi-positional MRI can be used to reliably evaluate for cervical instability.
For the C2–7 angle and the individual subaxial segmental angles, our study showed significant moderate to strong positive correlation in all parameters measured between multi-positional MRI and dynamic radiograph. This finding was strongest for images taken in the neutral position which showed strong correlation in all parameters except for the C6–7 angle which showed moderate correlation. The regression analysis for each parameter also showed a statistically significant correlation between two image modalities. These results confirmed our hypothesis that the angular measurement parameters measured from either multi-positional MRI or dynamic plain radiograph in the same setting could be reliably substitute each other for radiographic evaluation. In other words, if angular instability on multi-positional MRI was identified, the same patient will have the moderate to strong chance of having the angular instability identified by dynamic plain radiograph. Similarly, the angles measured on dynamic plain radiograph can be used to predict, with moderate to strong reliability, cervical spine soft tissue pathology including disc degeneration, cord compression, and sagittal spine malalignment that would be shown using multi-positional MRI [2, 16,17,18].
Plain radiograph should still be the mainstay for evaluation of dynamic angular parameters in the cervical spine given its widespread availability, affordability, and low risk when used appropriately in the general population. However, our findings show that multi-positional MRI can also be reliably used for angular measurement in the cervical spine. Given this finding, multi-positional MRI should be considered as an alternative for evaluating cervical instability in patients with high risks associated with radiation including children and pregnant women. Furthermore, because multi-positional MRI can perform dynamic soft tissue evaluation whereas dynamic radiographs only show bony structures, multi-positional MRI should also be used in patients being evaluated for cervical instability who also have cervical degeneration or minute cervical trauma that require dynamic soft tissue pathology evaluation. Finally, because our findings show that cervical segmental angular measurements taken with the two imaging modalities are comparable, dynamic plain radiographs can be used to estimate cervical soft tissue pathology.
To our knowledge, this is the first study that has evaluated the reliability and validity of measuring angular parameters on cervical multi-positional MRI using the gold standard of dynamic plain radiograph as a control. In addition to the previously mentioned benefits, multi-positional MRI also allows patients to be imaged in three weight-bearing positions, and can overcome the limitation of X-rays in evaluation below the C7 lower endplate region. The multi-positional MRI was more accurate than dynamic plain radiograph for all parameters. This is particularly important for the lower cervical levels which are not reliably visualized in plain radiograph [13, 19].
While one of the strengths of this study’s design was that it allowed for the direct comparison of multi-positional MRI and dynamic plain radiographs of the cervical spine taken in the same setting, this greatly limited the number of patients eligible for the study which decreased the overall power. Many patients also had to be excluded because their cervical radiographs did not contain a full view of the lower endplate of C7. Another limitation of this study was that it did not allow us to compare the translational motion of the cervical spine between both modalities. This is because plain radiograph provides a two-dimensional image and multi-positional MRI provides multiple sections. For the same reason, multi-positional MRI measurements could be taken on a mid-sagittal image whereas measurements with radiographs did not represent a purely mid-sagittal view which created source of inconsistency. Finally, a lack of the patients’ clinical information was also a limitation because it did not allow the authors to compare correlation of measurements in patients with varying levels of pathology.
Conclusion
Measurements of the C2–7 angle and segmental angles of the cervical spine taken using weight-bearing multi-positional MRI can reliably substitute measurements using dynamic plain radiograph within an acceptable range of error. As such, multi-positional MRI can be used as a reliable tool for angular parameter measurement in the cervical spine. Similarly, dynamic plain radiograph angular measurements can reliably substitute measurements taken using multi-positional MRI within the acceptance of error. Therefore, dynamic plain radiograph angular parameters can potentially be used as a predictor of significant pathological soft tissue findings reported by previous cervical multi-positional MRI studies, including disc degeneration, spinal cord compression, and sagittal misalignment.
References
Harris MB, Kronlage SC, Carboni PA, Robert KQ, Menmuir B, Ricciardi JE, Chutkan NB (2000) Evaluation of the cervical spine in the polytrauma patient. Spine (Phila Pa 1976) 25(22):2884–2891 (discussion 2892)
Dvorak J, Panjabi MM, Grob D, Novotny JE, Antinnes JA (1993) Clinical validation of functional flexion/extension radiographs of the cervical spine. Spine (Phila Pa 1976) 18(1):120–127
Bone CM, Hsieh GH (2000) The risk of carcinogenesis from radiographs to pediatric orthopaedic patients. J Pediatr Orthop 20(2):251–254
Lee MC, Solomito M, Patel A (2013) Supine magnetic resonance imaging Cobb measurements for idiopathic scoliosis are linearly related to measurements from standing plain radiographs. Spine (Phila Pa 1976) 38(11):E656–E661. doi:10.1097/BRS.0b013e31828d255d
Lord EL, Alobaidan R, Takahashi S, Cohen JR, Wang CJ, Wang BJ, Wang JC (2014) Kinetic magnetic resonance imaging of the cervical spine: a review of the literature. Glob Spine J 4(2):121–128. doi:10.1055/s-0034-1375563
Muhle C, Metzner J, Weinert D, Schon R, Rautenberg E, Falliner A, Brinkmann G, Mehdorn HM, Heller M, Resnick D (1999) Kinematic MR imaging in surgical management of cervical disc disease, spondylosis and spondylotic myelopathy. Acta Radiol 40(2):146–153
Miyazaki M, Hong SW, Yoon SH, Zou J, Tow B, Alanay A, Abitbol JJ, Wang JC (2008) Kinematic analysis of the relationship between the grade of disc degeneration and motion unit of the cervical spine. Spine (Phila Pa 1976) 33(2):187–193. doi:10.1097/BRS.0b013e3181604501
Miyazaki M, Hymanson HJ, Morishita Y, He W, Zhang H, Wu G, Kong MH, Tsumura H, Wang JC (2008) Kinematic analysis of the relationship between sagittal alignment and disc degeneration in the cervical spine. Spine (Phila Pa 1976) 33(23):E870–E876. doi:10.1097/BRS.0b013e3181839733
Morishita Y, Naito M, Hymanson H, Miyazaki M, Wu G, Wang JC (2009) The relationship between the cervical spinal canal diameter and the pathological changes in the cervical spine. Eur Spine J 18(6):877–883. doi:10.1007/s00586-009-0968-y
Evans JD (1996) Straightforward statistics for the behavioral sciences. Brooks/Cole Pub. Co., Pacific Grove
Griffiths HJ, Wagner J, Anglen J, Bunn P, Metzler M (2002) The use of forced flexion/extension views in the obtunded trauma patient. Skelet Radiol 31(10):587–591. doi:10.1007/s00256-002-0545-5
Khan SN, Erickson G, Sena MJ, Gupta MC (2011) Use of flexion and extension radiographs of the cervical spine to rule out acute instability in patients with negative computed tomography scans. J Orthop Trauma 25(1):51–56. doi:10.1097/BOT.0b013e3181dc54bf
Sierink JC, van Lieshout WA, Beenen LF, Schep NW, Vandertop WP, Goslings JC (2013) Systematic review of flexion/extension radiography of the cervical spine in trauma patients. Eur J Radiol 82(6):974–981. doi:10.1016/j.ejrad.2013.02.009
Ruegg TB, Wicki AG, Aebli N, Wisianowsky C, Krebs J (2015) The diagnostic value of magnetic resonance imaging measurements for assessing cervical spinal canal stenosis. J Neurosurg Spine 22(3):230–236. doi:10.3171/2014.10.SPINE14346
Kristjansson E, Leivseth G, Brinckmann P, Frobin W (2003) Increased sagittal plane segmental motion in the lower cervical spine in women with chronic whiplash-associated disorders, grades I-II: a case-control study using a new measurement protocol. Spine (Phila Pa 1976) 28(19):2215–2221. doi:10.1097/01.BRS.0000089525.59684.49
Dvorak J, Antinnes JA, Panjabi M, Loustalot D, Bonomo M (1992) Age and gender related normal motion of the cervical spine. Spine (Phila Pa 1976) 17(10 Suppl):S393–S398
Buonocore E, Hartman JT, Nelson CL (1966) Cineradiograms of cervical spine in diagnosis of soft-tissue injuries. JAMA 198(1):143–147
Dimnet J, Pasquet A, Krag MH, Panjabi MM (1982) Cervical spine motion in the sagittal plane: kinematic and geometric parameters. J Biomech 15(12):959–969
Davis JW, Kaups KL, Cunningham MA, Parks SN, Nowak TP, Bilello JF, Williams JL (2001) Routine evaluation of the cervical spine in head-injured patients with dynamic fluoroscopy: a reappraisal. J Trauma 50(6):1044–1047
Acknowledgements
This work was funded by departmental funds. The authors would like to thank AiM Radiology Medical Group, especially to Yusuf A. Khan, Sameer U. Khan and Aziza Qadir MD for their help on obtaining and uploading kMRI images into the database.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest. Disclosures: ZB-Xenco Medical (consultancy), AO Spine (consultancy, past); JCW–Royalties: Aesculap, Biomet, Amedica, Seaspine, Synthes; Stock Ownership: Fziomed; Private Investments: Promethean Spine, Paradigm spine, Benevenue, NexGen, Vertiflex, ElectroCore, Surgitech, Expanding Orthopaedics, Osprey, Bone Biologics, Curative Biosciences, PearlDiver; Board of Directors: North American Spine Society (Second Vice President), North American Spine Foundation (non-financial), Cervical Spine Research Society (Travel expenses), AO Spine/AO Foundation (honorariums for board position); Fellowship Support: AO Foundation (spine fellowship funding paid to institution).
Rights and permissions
About this article
Cite this article
Paholpak, P., Tamai, K., Shoell, K. et al. Can multi-positional magnetic resonance imaging be used to evaluate angular parameters in cervical spine? A comparison of multi-positional MRI to dynamic plain radiograph. Eur Spine J 27, 1021–1027 (2018). https://doi.org/10.1007/s00586-017-5306-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-017-5306-1