Abstract
Purpose
The purpose of this review was to develop recommendations for non-invasive management of pain due to osteoporotic vertebral compression fractures (OVCF) that could be applied in medically underserved areas and low- and middle-income countries.
Methods
We conducted a systematic review and best evidence synthesis of systematic reviews on the non-invasive management of OVCF. Eligible reviews were critically appraised using the Scottish Intercollegiate Guidelines Network criteria. Low risk of bias systematic reviews and high-quality primary studies that were identified in the reviews were used to develop recommendations.
Results
From 6 low risk of bias systematic reviews and 14 high-quality primary studies we established that for acute pain management, in addition to rest and analgesic medication, orthoses may provide temporary pain relief, in addition to early mobilization. Calcitonin can be considered as a supplement to analgesics; however, cost is of concern. Once acute pain control is achieved, exercise can be effective for improving function and quality of life.
Conclusion
The findings from this study will help to inform the GSCI care pathway and model of care for use in medically underserved areas and low- and middle-income countries. Conservative management of acute pain and recovery of function in adults with OVCF should include early mobilization, exercise, spinal orthosis for pain relief, and calcitonin for analgesic-refractory acute pain.
Graphical Abstract
These slides can be retrieved under Electronic Supplementary Material.

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The acute osteoporotic vertebral compression fracture (OVCF) is a serious form of spinal pathology, typically associated with moderate to severe initial pain, which is most commonly managed on an out-patient basis. Spinal compression fractures occur when the anterior portion of the vertebra breaks and loses height, while the posterior portion is maintained [1]. There are two types of compression fractures: Type I, where the anterior column is involved and the middle and posterior columns are intact; and Type II, where the anterior and middle columns are involved, and posterior column is intact [2]. Most spinal compression fractures occur in patients suffering from osteoporosis, owing to a decrease in vertebral bone mineral density [3]. In patients with healthy bone density, spinal compression fractures are most commonly caused by falls or motor vehicle collisions [4].
Notwithstanding sparse epidemiological information on osteoporosis and other fragility fractures in low- and middle-income countries, the disease burden of osteoporosis is known to be increasing as a result of the aging global population [5]. Major increases are expected to occur outside Europe and North America, impacting in particular Asia and South America [6]. Spinal compression fractures have considerable consequences for patients and society. Globally, in 2000, there were an estimated 1.4 million clinical vertebral osteoporotic fractures [7]. In Europe, the incidence of osteoporotic vertebral fractures is 5.7/1000 for men and 10.7/1000 for women [8], and its cost was estimated at €11 million in 2010 [9]. Osteoporotic spinal compression fractures, which tend to recur, are associated with considerable decline in physical and mental health-related quality of life [10–13].
The conclusions of systematic reviews regarding the management of osteoporotic compression fractures vary [14–22], due in part to differences in critical appraisal and evidence synthesis methodologies. Therefore, we conducted a systematic review of systematic reviews to synthesize the evidence and develop recommendations for the non-invasive management of acute pain due to acute OVCFs. This systematic review was carried out to inform the Global Spine Care Initiative, whose mandate is to transform the delivery of spine care, particularly in medically underserved areas and low- and middle-income countries [18].
Methods
Eligibility criteria
Population Our review targeted systematic reviews of adults or children with Type I or II OVCFs.
Intervention Non-invasive interventions including, but not limited to, bracing, pharmacotherapy, exercise, and passive physical modalities.
Comparison groups We included systematic reviews that compared non-invasive interventions to other non-invasive interventions, as well as placebo/sham intervention, wait list, or no intervention.
Outcomes Eligible reviews had to include at least one of the following outcomes: self-rated recovery, functional recovery (e.g., disability, return to activities, work, or school), clinical outcomes (e.g., pain, health-related quality of life, depression), administrative data (e.g., time on benefits), or adverse events.
Study characteristics Eligible reviews met the following: (1) English language; (2) published in a peer-review journal; (3) adults and/or children with Type I or II osteoporotic spinal compression fractures; and (4) management as outlined in systematic reviews.
We excluded: (1) publication types: letters, editorials, commentaries, unpublished manuscripts, dissertations, government reports, books and book chapters, conference proceedings, meeting abstracts, lectures and addresses, consensus development statements; and (2) previous versions of updated systematic reviews.
Information sources
We developed our search strategy in consultation with a health sciences librarian, which was reviewed by a second librarian using the Peer Review of Electronic Search Strategies (PRESS) Checklist [23, 24]. We systematically searched MEDLINE, EMBASE, AMED, National Guideline Clearinghouse, National Institute for Health and Care Excellence, World Health Organization Guidelines, CPG Infobase, ACP Clinical Practice Guidelines, Institute for Clinical Systems Improvement, and Australian Government from January 1, 1990 to May 13, 2015. Search terms consisted of subject headings specific to each database and free text words relevant to systematic reviews, guidelines, osteoporosis, and fractures (see Online Resource Appendix for the MEDLINE search strategy).
Study selection
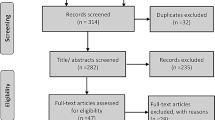
Random pairs of trained, independent reviewers selected eligible systematic reviews using a two-phase screening process [(1) titles/abstracts; and (2) full text]. Reviewers met to resolve disagreements and reach consensus on the eligibility of reviews. We involved a third reviewer if consensus could not be reached.
Assessment of risk of bias
Random pairs of independent reviewers critically appraised the internal validity of eligible systematic reviews using the Scottish Intercollegiate Guidelines Network (SIGN) criteria (see Online Resource Figure 1) [25]. Consensus between reviewers was reached through discussion. An independent third reviewer resolved disagreements if necessary. We contacted authors if additional information was needed to complete the critical appraisal. Low risk of bias systematic reviews were used in the evidence synthesis.
We did not use a quantitative score to assess the internal validity of the review. Instead, we focused on the presence or absence of important biases or methodological issues.
Data extraction and synthesis of results
The lead author extracted data from systematic reviews with a low risk of bias to build evidence tables. Two co-authors then extracted data from all low risk of bias primary studies included in the admissible systematic reviews. A second reviewer independently checked the extracted data. We performed a qualitative synthesis of findings from low risk of bias reviews and high-quality primary studies identified in these reviews to develop evidence statements according to principles of best evidence synthesis [26].
Statistical analysis
We computed inter-rater reliability for article screening using the kappa statistic (k) and 95% confidence interval (CI) [27]. We calculated the percentage agreement for classifying articles as scientifically admissible/inadmissible.
Reporting
We reported our systematic review based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [28].
Recommendations
Through consensus of the Global Spine Care Initiative (GSCI) Executive and co-authors, we categorized the magnitude of benefits and harms, costs and feasibility as uncertain, low/small, moderate, or high based on the categories used in the recent Agency for Healthcare Research and Quality (AHRQ) review on low back pain interventions [29] (see Online Resource Table 1). Recommendations were developed through consensus of the GSCI steering committee taking into consideration possible adaptations for low- and middle-income settings, using evidence of benefits and harms from the reviewed literature. We classified each recommendation using the system proposed by the National Institute for Health and Care Excellence (see Online Resource Table 2) [30]. Based on this methodology, recommendations start with the word ‘‘offer (recommended)’’ are for interventions that are of superior effectiveness compared to other interventions, placebo/sham interventions, or no intervention, “consider (recommended for consideration)” are for interventions providing similar effectiveness to other interventions, or “do not offer (recommended against)” are for interventions providing no benefit beyond placebo/sham or are harmful.
Results
Study selection
After removing duplicates, 649 articles were screened for eligibility resulting in 10 that were eligible for critical appraisal (see Online Resource Figure 2) [14–20, 22, 31, 32]. We were unable to retrieve full text for four eligible articles [33–36]. Six reviews had a low risk of bias and were included in our evidence synthesis [15, 16, 18–20, 22]. The inter-rater agreement for the screening of articles was k = 0.97 (95% CI 0.94, 0.99). The percentage agreement for the admissibility of systematic reviews during independent critical appraisal was 100% (10/10).
Study characteristics
Risk of bias within systematic reviews
We identified six systematic reviews with a low risk of bias for the management of acute pain from OVCFs [15, 16, 18–20, 22]. All six reviews with a low risk of bias had clear research questions, did a comprehensive literature search, specified whether they limited the review by publication type, provided characteristics of included studies, declared conflicts of interest, and appropriately assessed the scientific quality of studies (see Online Resource Table 3). Most reviews: (1) had at least two reviewers selecting studies and extracting data (5/6); and (2) used appropriate methods for combining studies (5/6). Systematic reviews had limitations: (1) did not list included and excluded studies (4/6); and (2) did not assess for the likelihood of publication bias (4/6).
Four systematic reviews with a high risk of bias had the following limitations: (1) unclear whether two reviewers performed data selection and extraction (3/4); (2) did not list included and excluded studies (4/4); (3) unclear or inadequate critical appraisal of study quality (4/4); (4) the scientific quality was not assessed appropriately (4/4); (5) inappropriate methods for combining studies (4/4); (6) no assessment of publication bias (4/4); and (7) did not declare conflicts of interest (3/4) (see Online Resource Table 4).
Quality of primary studies included in the systematic reviews
There were 14 high-quality primary studies within the 6 included systematic reviews (based on appraisal methods used in each review); however, we were unable to retrieve one high-quality primary study [37] (see Online Resource Tables 5 and 6). One systematic review only found low-quality primary studies and, therefore, results from these studies were not extracted and synthesized [20].
Summary of evidence
Medication
Recommendation 1: consider oral analgesics for acute pain control using recognized incremental approaches to the choice of drugs/drug combinations and dosages such as the WHO Analgesic Ladder, with full consideration of and patient education for side effects, complications and risks.
Although acute pain control is often a necessary component of treatment, the inconclusive nature of the current evidence for the effectiveness of any form of non-opioid or opioid analgesics for the treatment of acute pain after OVCFs precludes developing any specific guideline/approach for this injury. In the randomized controlled trial (RCT) by Vorsanger et al., no significant differences were found for pain at 72 h between oxycodone and placebo or between tapentadol and placebo; however, the study was underpowered to detect differences and was terminated early due to poor enrolment [38]. One RCT investigated three medications for the management of acute OVCF in women [39]. Participants in the study were randomized to receive: (1) tramadol hydrochloride (100 mg/day over 4 weeks); (2) diclofenac sodium (75 mg/day over 4 weeks); or (3) Xin Huang Pian (a combination of indomethacin and traditional Chinese medicines used for pain relief) when needed for severe pain. There were statistically significant differences favoring diclofenac sodium over Xin Huang Pian in the short term (≤1 week) [mean difference: −1.66 (95% CI −2.88, −0.44)] and intermediate term (>1 week ≤ 1 month) [mean difference: −1.17 (95% CI −2.32, −0.03)] for improvement of pain [39]. There were also statistically significant differences favouring tramadol hydrochloride over Xin Huang Pian in the short term (≤1 week) [mean difference: −1.58 (95% CI −2.83, −0.33)] and intermediate term (>1 week ≤ 1 month) [mean difference: 1.23 (95% CI −2.42, −0.05)] for improvement of pain [39]. Oxycodone and tapentadol have not been shown to be effective in providing short-term pain relief for vertebral compression fractures. Given the lack of evidence on analgesics specifically for compression fractures, clinicians should follow the WHO analgesic ladder for acute pain when considering analgesic drugs, generally with non-steroidal anti-inflammatories as a first-line option, reserving opioids for moderate to severe, refractory pain [40].
Recommendation 2: if oral analgesics do not achieve adequate pain relief for mild-moderate acute pain in OVCFs, consider supplementation with calcitonin (0–5 days post-onset of symptoms) (three reviews) [15, 16, 22] (see Online Resource Tables 5, 6 and Table 1).
The preponderance of the evidence found that calcitonin was more effective than placebo for acute OVCFs. Four high-quality primary studies in three systematic reviews [15, 16, 22] assessed the effectiveness of calcitonin for acute OVCFs compared to placebo intervention [41–44]. We were unable to retrieve a fifth primary study [37]. Three studies by Lyritis et al. demonstrated that calcitonin administered either through injection or suppository was significantly more effective than placebo for decrease in pain [41–43]. Additionally, two studies showed a significant difference in decreasing use of paracetamol favouring the calcitonin group [41, 43]. However, in another study by Ponteroli et al., there were no significant differences between the three groups (intranasal salmon calcitonin, intramuscular salmon calcitonin, and placebo) in pain [44]. It should be noted that tachyphylaxis is often seen with calcitonin, which limits long-term use. Calcitonin is also more expensive than other available analgesics [45, 46].
Exercise
Recommendation 3: once acute pain has been relieved, consider either supervised or unsupervised exercise (strengthening, stretching, and balance, agility, and posture exercises) for the initial rehabilitation of acute OVCFs (two reviews) [18, 47] (see Online Resource Tables 5, 6 and Table 1).
Exercise may be effective for the treatment of acute OVCFs. Two systematic reviews evaluated the effectiveness of exercise for the treatment of compression fractures [18, 19]. Four studies in the systematic reviews included post-menopausal women with osteoporosis with at least one vertebral compression fracture. Exercise interventions varied within each study but included strengthening, stretching, and balance, agility and posture exercises. Two studies assessed supervised exercise compared to usual activity [48, 49], one assessed home-based exercise compared to usual activity [50] and one assessed pain-free exercises compared to a combination of calcium, vitamin D, calcitonin and low-frequency pulsed electromagnetic field therapy [51]. All primary studies found that exercise was more effective than the comparison interventions for outcomes such as quality of life [49, 50], and various functional outcomes [48, 51]. Exercise should be introduced incrementally with particular caution in patients with acute (<3 months) fractures [48–50].
Orthoses
Recommendation 4: consider a spinal orthosis for the management of acute OVCFs (one review) [22] (see Online Resource Tables 5, 6 and Table 1).
One systematic review included one high-quality primary study that assessed the effectiveness of orthoses [22]. For acute OVCFs in osteoporotic women, subjects who received thoracolumbar orthoses gained significant increases in back extensor strength, abdominal flexor strength, body height, relaxed vital capacity, and well-being compared to no intervention. Statistically significant decreases in average pain and in parameters describing limitations of daily living, such as disability and self-care were seen in the orthotic groups compared to the no-intervention group [52].
Multimodal care
There is insufficient evidence for the effectiveness of multimodal care for acute OVCFs. Two systematic reviews included three high-quality primary studies of multimodal care for women with acute OVCFs [18, 19]. Two primary studies compared multimodal care versus no intervention [53, 54] and one primary study compared multimodal care versus education [55]. In one trial, multimodal care (taping, massage, mobilization, education and exercise addressing range of motion and posture) was more effective than no intervention for mean change (NRS 0–10) in pain on movement [1.8 (95% CI 0.1, 3.5)] or at rest [2.0 (95% CI 0.2, 3.9)] and improvement in physical function (QUALEFOO-41) [4.8 (95% CI 0.5, 9.2)] [54]. In one study by Bautmans et al., there was greater improvement in thoracic kyphosis in the multimodal care group (manual mobilization, taping, and exercises for postural correction) over wait-list (p = 0.017) [53]. In another study by Bautmans et al., no differences were found for quality of life or pain; however, the study had a small sample size and low compliance [53]. In the third study, Gold et al. found statistically significant differences in mean change for trunk extension strength [10.68 (95% CI 6.98, 14.39)] and psychological symptoms [−0.03 (95% CI −0.20, −0.10)] favouring multimodal care (exercise focusing on trunk weakness, flexibility and posture and coping classes) over education [55]. No significant differences were found between groups for pain with activities [55]. In these studies, sessions ranged from 10 weeks to 6 months.
Discussion
We summarized the findings from 6 systematic reviews, which drew upon 14 high-quality primary studies. We did not find evidence that would permit creation of a unique analgesic drug choice/dose guideline specific to acute OVCF pain control: we instead suggest the use of existing general acute analgesia guidelines such as that of WHO [56]. Our review suggests that calcitonin may be effective for moderate to severe pain when oral analgesics have failed to achieve effective pain relief; however, calcitonin is costly compared to other analgesics. Orthoses were found to be effective for interim pain relief and facilitation of early mobilization and have the additional advantage of being potentially available at a low cost; however, evidence was limited to one high-quality trial. Our review found that exercise was effective for initial rehabilitation of OVCF, once acute pain was relieved. However, there was insufficient evidence for increased efficacy through multimodal interventions.
Implications for management of pain due to acute OVCFs in low- and middle-income communities
We conducted this systematic review within the Global Spine Care Initiative, whose mandate is to inform the implementation of evidence-based spine care in underserved and low-income communities worldwide [18].
Most patients who present with an acute OVCF do not require hospitalization; exceptions may include spinal instability, neurological impairment, or absence of pain control. There are a discrete set of components needed in any program of care for effective symptom management and rehabilitation of acute OVCFs within the patient’s own community. These components include education; activity regulation; pain control and facilitation of remobilization through analgesic drugs, spinal orthoses and rehabilitative exercises. Provision of a program of care with these components would appear to be at least potentially feasible for many underserved, low and moderate-income communities.
Osteoporosis is a progressive, systemic illness. Alongside fracture symptom control and rehabilitation, it is critically important to address the underlying osteoporosis. In most cases, and even more so in underserved communities, the onset of the first acute OVCF is the first opportunity to diagnose and then manage the underlying condition.
Strengths
Our review has strengths. First, we developed a comprehensive search strategy in consultation with a health sciences librarian, which was peer reviewed by a second librarian to minimize errors. Second, we defined an explicit set of eligibility criteria and developed a standardized screening process to identify relevant systematic reviews. Pairs of trained, independent reviewers used the SIGN criteria to assess internal validity of relevant studies. Finally, we followed best evidence synthesis principles to only synthesize the evidence from primary studies with low risk of bias and minimize bias associated with high risk of bias studies, increasing confidence in the results.
Limitations
Our review has limitations. We only searched the English literature; however, systematic reviews of clinical trials investigating the impact of language restriction found that it does not lead to bias as most large trials are published in English [28, 57]. It is also possible that potentially relevant articles were excluded from our search, given the lack of consistency in terminology for osteoporotic vertebral compression fracture. Third, critical appraisal of systematic reviews may vary between reviewers. However, reviewers were trained in advance and standardized assessment forms were used to minimize potential bias.
Conclusions
Our review informs the development of evidence-based approaches for the non-invasive management of acute pain and recovery of function in adults with acute OVCFs. Since evidence on the effectiveness of analgesic drugs for acute pain in osteoporotic spinal compression fractures is limited, general principles of analgesic use based on the WHO analgesic ladder are recommended. Calcitonin can be considered for refractory pain; however, cost may be an issue. There is a potential role for spinal orthoses for the management of pain and early mobilization for osteoporotic spinal compression fractures. The current literature suggests that exercise can be effective for restoring function and quality of life after an acute OVCFs.
References
American Association of Neurological Surgeons (2016) Vertebral compression fractures. http://www.aans.org/patient%20information/conditions%20and%20treatments/vertebral%20compression%20fractures.aspx. Accessed 1 Dec 2016
Denis F (1984) Spinal instability as defined by the three-column spine concept in acute spinal trauma. Clin Orthop Relat Res (189):65–76
Cooper C, Melton LJ III (1992) Epidemiology of osteoporosis. Trends Endocrinol Metab 3:224–229. https://doi.org/10.1016/1043-2760(92)90032-V
Hu R, Mustard CA, Burns C (1996) Epidemiology of incident spinal fracture in a complete population. Spine (Phila Pa 1976) 21:492–499
Handa R, Ali Kalla A, Maalouf G (2008) Osteoporosis in developing countries. Best Pract Res Clin Rheumatol 22:693–708. https://doi.org/10.1016/j.berh.2008.04.002
World Health Organization (2007) WHO scientific group on the assessment of osteoporosis at primary health care level. http://www.who.int/chp/topics/Osteoporosis.pdf. Accessed 27 Jan 2017
Johnell O, Kanis JA (2006) An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 17:1726–1733. https://doi.org/10.1007/s00198-006-0172-4
Felsenberg D, Silman AJ, Lunt M, Armbrecht G, Ismail AA, Finn JD, Cockerill WC, Banzer D, Benevolenskaya LI, Bhalla A, Bruges Armas J, Cannata JB, Cooper C, Dequeker J, Eastell R, Felsch B, Gowin W, Havelka S, Hoszowski K, Jajic I, Janott J, Johnell O, Kanis JA, Kragl G, Lopes Vaz A, Lorenc R, Lyritis G, Masaryk P, Matthis C, Miazgowski T, Parisi G, Pols HA, Poor G, Raspe HH, Reid DM, Reisinger W, Schedit-Nave C, Stepan JJ, Todd CJ, Weber K, Woolf AD, Yershova OB, Reeve J, O’Neill TW (2002) Incidence of vertebral fracture in Europe: results from the European Prospective Osteoporosis Study (EPOS). J Bone Miner Res 17:716–724. https://doi.org/10.1359/jbmr.2002.17.4.716
Svedbom A, Hernlund E, Ivergard M, Compston J, Cooper C, Stenmark J, McCloskey EV, Jonsson B, Kanis JA (2013) Osteoporosis in the European Union: a compendium of country-specific reports. Arch Osteoporos 8:137. https://doi.org/10.1007/s11657-013-0137-0
Lindsay R, Silverman SL, Cooper C, Hanley DA, Barton I, Broy SB, Licata A, Benhamou L, Geusens P, Flowers K, Stracke H, Seeman E (2001) Risk of new vertebral fracture in the year following a fracture. JAMA 285:320–323
Al-Sari UA, Tobias J, Clark E (2016) Health-related quality of life in older people with osteoporotic vertebral fractures: a systematic review and meta-analysis. Osteoporos Int 27:2891–2900. https://doi.org/10.1007/s00198-016-3648-x
Silverman SL (1992) The clinical consequences of vertebral compression fracture. Bone 13(Suppl 2):S27–S31
Burger H, Van Daele PL, Grashuis K, Hofman A, Grobbee DE, Schutte HE, Birkenhager JC, Pols HA (1997) Vertebral deformities and functional impairment in men and women. J Bone Miner Res 12:152–157. https://doi.org/10.1359/jbmr.1997.12.1.152
Blau LA, Hoehns JD, Nazario M, Gagnon L (2003) Analgesic efficacy of calcitonin for vertebral fracture pain. Ann Pharmacother 37:564–570. https://doi.org/10.1345/aph.1C350
Knopp-Sihota JA, Newburn-Cook CV, Homik J, Cummings GG, Voaklander D (2012) Calcitonin for treating acute and chronic pain of recent and remote osteoporotic vertebral compression fractures: a systematic review and meta-analysis. Osteoporos Int 23:17–38. https://doi.org/10.1007/s00198-011-1676-0
Knopp JA, Diner BM, Blitz M, Lyritis GP, Rowe BH (2005) Calcitonin for treating acute pain of osteoporotic vertebral compression fractures: a systematic review of randomized, controlled trials. Osteoporos Int 16:1281–1290
Longo UG, Loppini M, Denaro L, Maffulli N, Denaro V (2012) Conservative management of patients with an osteoporotic vertebral fracture: a review of the literature. J Bone Jt Surg Br 94:152–157. https://doi.org/10.1302/0301-620X.94B2.26894
Dusdal K, Grundmanis J, Luttin K, Ritchie P, Rompre C, Sidhu R, Harris SR (2011) Effects of therapeutic exercise for persons with osteoporotic vertebral fractures: a systematic review. Osteoporos Int 22:755–769. https://doi.org/10.1007/s00198-010-1497-6
Giangregorio LMM, Macintyre NJ, Thabane L, Skidmore CJ, Papaioannou A (2013) Exercise for improving outcomes after osteoporotic vertebral fracture. Cochrane Database Syst Rev 1:CD008618. https://doi.org/10.1002/14651858.CD008618.pub2
Giele BM, Wiertsema SH, Beelen A, van der Schaaf M, Lucas C, Been HD, Bramer JA (2009) No evidence for the effectiveness of bracing in patients with thoracolumbar fractures. Acta Orthop 80:226–232. https://doi.org/10.3109/17453670902875245
Chen LX, Li YL, Ning GZ, Li Y, Wu QL, Guo JX, Shi HY, Wang XB, Zhou Y, Feng SQ (2015) Comparative efficacy and tolerability of three treatments in old people with osteoporotic vertebral compression fracture: a network meta-analysis and systematic review. PLoS One 10:e0123153. https://doi.org/10.1371/journal.pone.0123153
Rzewuska M, Ferreira M, McLachlan AJ, Machado GC, Maher CG (2015) The efficacy of conservative treatment of osteoporotic compression fractures on acute pain relief: a systematic review with meta-analysis. Eur Spine J 24:702–714. https://doi.org/10.1007/s00586-015-3821-5
Sampson M, McGowan J, Cogo E, Grimshaw J, Moher D, Lefebvre C (2009) An evidence-based practice guideline for the peer review of electronic search strategies. J Clin Epidemiol 62(9):944–952
McGowan JSM, Lefebvre C (2010) An evidence based checklist for the peer review of electronic search strategies. Evid Based Libr Inf Pract 5(1):149–154
Shea BJ, Grimshaw JM, Wells GA, Boers M, Andersson N, Hamel C, Porter AC, Tugwell P, Moher D, Bouter LM (2007) Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol 7:10. https://doi.org/10.1186/1471-2288-7-10
Slavin RE (1995) Best evidence synthesis: an intelligent alternative to meta-analysis. J Clin Epidemiol 48:9–18
Viera AJ, Garrett JM (2005) Understanding interobserver agreement: the kappa statistic. Fam Med 37:360–363
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ (Clinical research ed) 339:b2535. https://doi.org/10.1136/bmj.b2535
Chou R, Hashimoto R, Friedly J, Fu R, Dana T, Sullivan S, Bougatsos C, Jarvik J (2015) AHRQ Technology assessments. In: Pain management injection therapies for low back Pain. Agency for Healthcare Research and Quality (US), Rockville (MD)
National Institute for Health and Care Excellence (NICE) (2012) The guidelines manual. https://www.nice.org.uk/article/pmg6/chapter/1%20introduction#ftn.footnote_1. Accessed 16 May 2016
de Kam D, Smulders E, Weerdesteyn V, Smits-Engelsman BC (2009) Exercise interventions to reduce fall-related fractures and their risk factors in individuals with low bone density: a systematic review of randomized controlled trials. Osteoporos Int 20:2111–2125. https://doi.org/10.1007/s00198-009-0938-6
Elliot-Gibson V, Bogoch ER, Jamal SA, Beaton DE (2004) Practice patterns in the diagnosis and treatment of osteoporosis after a fragility fracture: a systematic review. Osteoporos Int 15:767–778. https://doi.org/10.1007/s00198-004-1675-5
Bajaj S, Saag KG (2003) Osteoporosis: evaluation and treatment. Curr Womens Health Rep 3:418–424
Anonymous (2000) Osteoporosis prevention, diagnosis, and therapy. NIH Consens Statement 17:1–45
Hough SM, Mahlati MP (2000) Diagnosis and management of osteoporosis-full guideline. S Afr Med J 90:907–944
Coggins ME (1995) Nonunions and malunions of thoracolumbar spine injuries. Semin Spine Surg 7:137–140
Consoli V, Alfieri P, Giuntini C, Mancia M, Avaldi F, Soncini R (1991) A double blind placebo-controlled trial of the efficacy and tolerability of intranasal elcatonin administered to patients suffering from senile and postmenopausal osteoporosis. Curr Ther Res 50:369–378
Vorsanger GJ, Farrell J, Xiang J, Chow W, Moskovitz BL, Rosenthal NR (2013) Tapentadol, oxycodone or placebo for acute pain of vertebral compression fractures: a randomized Phase IIIb study. Pain Manag 3:109–118. https://doi.org/10.2217/pmt.13.5
Zhang THD, YH, Yu SM, Zhnag C, Ya B (2013) Analgesics osteoporotic fracture healing. J Clin Rehabil Tissue Eng Res 17:6364-6374
World Health Organization WHO’s cancer pain ladder for adults. http://www.who.int/cancer/palliative/painladder/en/. Accessed 5 Feb 2017
Lyritis GP, Ioannidis GV, Karachalios T, Roidis N, Kataxaki E, Papaioannou N, Kaloudis J, Galanos A (1991) Analgesic effect of salmon calcitonin in osteoporotic vertebral fractures: a double-blind placebo-controlled clinical study. Calcif Tissue Int 49:369–372
Lyritis GP, Paspati I, Karachalios T, Ioakimidis D, Skarantavos G, Lyritis PG (1997) Pain relief from nasal salmon calcitonin in osteoporotic vertebral crush fractures. A double blind, placebo-controlled clinical study. Acta Orthop Scand Suppl 275:112–114
Lyritis GP, Ioannidis GV, Karachalios T, Roidis N, Kataxaki E, Papaioannou N, Kaloudis J, Galanos A (1999) Analgesic effect of salmon calcitonin suppositories in patients with acute pain due to recent osteoporotic vertebral crush fractures: a prospective double-blind, randomized, placebo-controlled clinical study. Clin J Pain 15:284–289
Pontiroli AE, Pajetta E, Scaglia L, Rubinacci A, Resmini G, Arrigoni M, Pozza G (1994) Analgesic effect of intranasal and intramuscular salmon calcitonin in post-menopausal osteoporosis: a double-blind, double-placebo study. Aging (Milan, Italy) 6:459–463
Flynn JA, Choi MJ, Wooster LD (2013) Oxford American handbook of clinical medicine. Oxford University Press, New York
Carroll R, Matfin G (2010) Endocrine and metabolic emergencies: hypercalcaemia. Ther Adv Endocrinol Metab 1:225–234. https://doi.org/10.1177/2042018810390260
Giangregorio LM, Macintyre NJ, Thabane L, Skidmore CJ, Papaioannou A (2013) Exercise for improving outcomes after osteoporotic vertebral fracture. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD008618.pub2
Bergland A, Thorsen H, Karesen R (2011) Effect of exercise on mobility, balance, and health-related quality of life in osteoporotic women with a history of vertebral fracture: a randomized, controlled trial. Osteoporos Int 22:1863–1871. https://doi.org/10.1007/s00198-010-1435-7
Malmros B, Mortensen L, Jensen MB, Charles P (1998) Positive effects of physiotherapy on chronic pain and performance in osteoporosis. Osteoporos Int 8:215–221. https://doi.org/10.1007/s001980050057
Papaioannou A, Adachi JD, Winegard K, Ferko N, Parkinson W, Cook RJ, Webber C, McCartney N (2003) Efficacy of home-based exercise for improving quality of life among elderly women with symptomatic osteoporosis-related vertebral fractures. Osteoporos Int 14:677–682. https://doi.org/10.1007/s00198-003-1423-2
Yang LH, Cheng-qi H, Lei Z, Xie W, Lan Q (2007) Effect of pain-free exercises on female osteoporosis patients with spinal compressive fracture. J Clin Rehabil Tissue Eng Res 11:9108–9111
Pfeifer M, Kohlwey L, Begerow B, Minne HW (2011) Effects of two newly developed spinal orthoses on trunk muscle strength, posture, and quality-of-life in women with postmenopausal osteoporosis: a randomized trial. Am J Phys Med Rehabil 90:805–815. https://doi.org/10.1097/PHM.0b013e31821f6df3
Bautmans I, Van Arken J, Van Mackelenberg M, Mets T (2010) Rehabilitation using manual mobilization for thoracic kyphosis in elderly postmenopausal patients with osteoporosis. J Rehabil Med 42:129–135. https://doi.org/10.2340/16501977-0486
Bennell KL, Matthews B, Greig A, Briggs A, Kelly A, Sherburn M, Larsen J, Wark J (2010) Effects of an exercise and manual therapy program on physical impairments, function and quality-of-life in people with osteoporotic vertebral fracture: a randomised, single-blind controlled pilot trial. BMC Musculoskelet Disord 11:36. https://doi.org/10.1186/1471-2474-11-36
Gold DT, Shipp KM, Pieper CF, Duncan PW, Martinez S, Lyles KW (2004) Group treatment improves trunk strength and psychological status in older women with vertebral fractures: results of a randomized, clinical trial. J Am Geriatr Soc 52:1471–1478. https://doi.org/10.1111/j.1532-5415.2004.52409.x
World Health Organization (2012) Scoping document for WHO guidelines for the pharmacological treatment of persisting pain in adults with medical illnesses. In: Pain TGo (ed). http://www.who.int/medicines/areas/quality_safety/Scoping_WHO_GLs_PersistPainAdults_webversion.pdf?ua=1. Accessed 5 Feb 2017
Morrison A, Polisena J, Husereau D, Moulton K, Clark M, Fiander M, Mierzwinski-Urban M, Clifford T, Hutton B, Rabb D (2012) The effect of English-language restriction on systematic review-based meta-analyses: a systematic review of empirical studies. Int J Technol Assess Health Care 28:138–144. https://doi.org/10.1017/s0266462312000086
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The Global Spine Care Initiative and this study were funded by grants from the Skoll Foundation and NCMIC Foundation. World Spine Care provided financial management for this project. The funders had no role in study design, analysis, or preparation of this paper.
Conflict of interest
AA declares no COI. KR declares funding to UOIT from Skoll Foundation, NCMIC Foundation through World Spine Care. HY declares funding to UOIT from Skoll Foundation, NCMIC Foundation through World Spine Care. PC declares funding to UOIT from Skoll Foundation, NCMIC Foundation through World Spine Care; Canadian Institutes of Health Research Canada. Research Chair Ontario Ministry of Finance; Financial Services Commission of Ontario; Ontario Trillium Foundation, ELIB Mitac; Fond de Recherche and Sante du Quebec. SH declares funding to UOIT from Skoll Foundation, NCMIC Foundation through World Spine Care; Clinical Policy Advisory Board and stock holder, Palladian Health; Advisory Board, SpineHealth.com; Book Royalties, McGraw Hill; Travel expense reimbursement—CMCC Board. RC declares funding from AHRQ to conduct systematic reviews on treatments for low back pain within last 2 years. Honoraria for speaking at numerous meetings of professional societies and non-profit groups on topics related to low back pain (no industry sponsored talks). EH declares he is a consultant for: RAND Corporation; EBSCO Information Services; Southern California University of Health Sciences; Western University of Health Sciences Data and Safety Monitoring Committee; Chair, Palmer Center for Chiropractic Research; Research Committee Co-chair, World Spine Care. MN declares funding from Skoll Foundation and NCMIC Foundation through World Spine Care; Co-Chair, World Spine Care Research Committee; Palladian Health, Clinical Policy Advisory Board member; Book Royalties Wolters Kluwer and Springer; Honoraria for speaking at research method courses. JJW declares funding to UOIT from Skoll Foundation, NCMIC Foundation through World Spine Care. HR declares funding to UOIT from Skoll Foundation, NCMIC Foundation through World Spine Care. ATV declares funding to UOIT from Skoll Foundation, NCMIC Foundation through World Spine Care.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ameis, A., Randhawa, K., Yu, H. et al. The Global Spine Care Initiative: a review of reviews and recommendations for the non-invasive management of acute osteoporotic vertebral compression fracture pain in low- and middle-income communities. Eur Spine J 27 (Suppl 6), 861–869 (2018). https://doi.org/10.1007/s00586-017-5273-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-017-5273-6