Abstract
Background
Protocols including combination of surgery and radiotherapy are more and more frequent in the treatment of bone tumors of the spine. In metastatic disease, combination of surgery and radiotherapy is since long time accepted, as based on clinical evidence. In primary tumors, combination of surgery and radiotherapy can be considered in all the cases in which a satisfactory oncological margin cannot be achieved: high-grade malignancies, recurrent tumors, huge tumors expanding in an extracompartimental area, and when tumor-free margin requires unacceptable functional sacrifices. However, metal implants are an obstacle in the collaboration between surgeons and radiation oncologists. Carbon-fiber-reinforced polyethil–ether–ether–ketone (CFR-PEEK) composite implants could make easier and more effective the treatment as radiolucent and not interfering with ionizing radiation and accelerated particles. The purpose of this article is to report the preliminary results from a cohort of patients treated with CFR-PEEK and to evaluate the safety and the non-inferiority of the device respect the commonly used titanium implants.
Materials and methods
This study concerns an ambispective cohort series of 34 tumor patients (14 metastases and 20 primaries, most of them recurrent) submitted to thoracic and lumbar spine fixation with a CFR-PEEK composite implants. Oncologic surgery was palliative decompression and fixation in 9 cases, tumor excision in 21, and enbloc resection in 4. Data collected for this preliminary report were all intraoperative remarks, incidence of complications, changes in neurological status, local control, and survival. All the cases were followed 6–36 months (mean 13 months).
Results
Only one intraoperative screw breakage occurred out of 232 implanted screws. Pain control and neurological improvement were the early clinical results. Two sacral screws loosening were found at 9 and 12 months in multilevel constructs performed on multirecurrent tumors. Six local recurrences were early found thanks to the implant radiolucency. Radiation oncologists’ opinion was favourable as concerning better treatment planning on CT and lacking of scattering effect during the treatment.
Conclusions
No artifacts on imaging studies mean early local recurrence detection. For radiation oncologists, no artifacts on imaging studies mean easier planning and no scattering effect means more effective and safe radiotherapy, particularly when particles are used. Moreover, it seems that the clinical use of CFR-PEEK composite implants may be safe and at least comparable with the commonly used titanium implants in terms of intraoperative complications, stability at weight bearing and at functional recovery. Larger patient series and longer follow-up are required to confirm these data.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Combination of surgery and radiotherapy is becoming more and more frequent in the protocols for the treatment of bone tumors of the spine [1].
Primary tumor treatment is based on diagnosis and oncological staging and surgical aggressiveness should be proportional to biological behavior [2, 3].
Intralesional excision is the procedure of choice of active stage 2 benign tumors. Intralesional excision combined with radiotherapy can be performed in aggressive benign tumors (stage 3). Enbloc resection is the treatment of choice of primary malignant or aggressive benign tumors [4] and can occasionally be performed in some selected solitary metastases [5].
Enbloc resection is a very demanding [6, 7] and morbid [8] surgical technique.
Enbloc resection is not always feasible due to anatomical and surgical constraints. Criteria for feasibility have been proposed to achieve a tumor-free margin specimen [9, 10]; however, sometimes to achieve adequate tumor margins, enbloc resection can include loss of function due to sacrifice of anatomical structures (nerves, dura, and vessels) [11]. Intentional transgression to oncological principles can be necessary to respect patient requirements (even if associated with a substantially increased risk of local recurrence and with a worse final outcome). Margin violation can occur incidentally particularly in huge tumors or in tumors expanding towards an extracompartimental space and, therefore, only covered by a thin pseudocapsule. In huge high-grade sarcomas, the thickness of margins achieved in the spine can be inadequate compared to the tumor aggressiveness. Both intentional and accidental transgressions of oncological principles are indications to radiotherapy [12]. In the treatment of local recurrence, enbloc resection is associated with lower effectiveness in local control: consequently, morbidity and functional loss are less acceptable [13, 14]. When enbloc resection is not feasible or refused by the patient, gross-total excision combined with radiotherapy is frequently the only option.
Therefore, combination of surgery and radiotherapy is a reasonable option when:
-
enbloc resection is not feasible or requiring unacceptable morbidity and/or loss of function;
-
intentional margin transgression is planned as functional loss not accepted by the patient;
-
accidental margin transgression occurs during surgery with tumor spilling and/or violation of the margins. In high-grade tumors, required margins are difficult to achieve in the spine;
-
in recurrent tumor when enbloc resection is less effective due to tumor contamination and associated with increased morbidity.
Conversely, in the treatment of spine metastases, radiotherapy combined with surgery is considered since long time the most reliable strategy [15]. This concept has been reinforced over the time and it is included in all the proposed protocols [16]. With the progressive improvements of radiotherapy protocols and the introduction of new techniques, the best combination seems to select the less morbid surgery (from partial curettage to gross-total excision) combined with the most effective radiotherapy [17, 18].
The emerging obstacle to the symbiotic evolution of surgery and radiotherapy is the metallic hardware that can interfere due to the artifacts on imaging and due to the scattering effects on treatment by ionizing radiations including accelerated particles. The risk of over irradiation of neighboring structures limits the dose delivered making treatment less effective.
Composite materials such as carbon-fiber-reinforced (CFR) polyethil–ether–ether–ketone (PEEK) have been used since many years for interbody and body replacement cages [19, 20]. This material is biologically compatible and experimental works confirmed a strong effectiveness in promoting osteoblastic activity [21]. These cages proved to be excellent from a laboratory and clinical point of view, with an outstanding positive clinical experience of almost 30 years [22, 23]. These cages are radiolucent at the standard radiograms, barely visible on TC scan and MRI, allowing easy planning CT scan [24], early detection of local recurrence and very useful to avoid any scattering effect during radiotherapy.
CFR-PEEK fixation systems are available as plates and nails since several years for long bones fixation [25, 26]. Recently, a CFR-PEEK spine fixation system featuring an original rod/screw connection by impaction has been recently proposed.
The purpose of this article is to report on the preliminary results from an ambispective cohort of patients treated by this new implant for the treatment of bone tumors in the perspective of subsequent radiation treatment.
The target of this study is to demonstrate that this new system is at least not inferior if compared to the literature report on the commonly used titanium implants from the point of view of intra- and early post-operative safety and reliability and to report on the radiation oncologists’ opinion at planning and delivering of different techniques and protocols of radiotherapy.
Further studies will follow to report on middle- and long-term local results and patients’ outcome.
Materials and methods
An ambispective study was performed on the first 34 consecutive tumor patients, treated in a single institution from December 2013 to July 2016, who underwent spinal surgery including a composite CFR-PEEK fixation system (Carboclear™, produced by CarboFix Orthopedics® Ltd., Herziliya, IL).
The inclusion criteria were patients with metastases in the thoracic and lumbar spine with skeletal-related events, including severe pain, pathologic fractures, and metastatic epidural spinal cord compression. Patients with radioresistant or previously radiated spinal lesions were also included in this study.
Primary tumors were also included, whose planned treatment strategy had to combine surgery and radiotherapy.
Fixation was associated with: (a) palliative surgery (decompression) in 9 cases; (b) tumor intralesional excision (debulking/curettage) in 21; and (c) en bloc resection (extralesional removal of the whole tumor covered by a continuous shell of healthy tissue all around it) in 4. When reconstruction of the anterior column was needed (15 cases), composite CFR-PEEK cage was implanted in four cases, acrylic cement was used in eight cases, and titanium cage in two and massive allograft in one.
At the discharge, the patients were referred to different centers of radiotherapy with a specific questionnaire for radiation oncologist’s comment about the validity of the system for improving the effectiveness of radiotherapy. The results of their opinions are still pending and will be the subject of a further article.
This study obtained the approval of the Institute’s Ethical Committee: the results of the prospective study on the first 15 patients were submitted to achieve the EC mark for the implanted device.
The population of the cohort object of the present report includes 18 males and 16 females with a mean age of 57.4 years (range 16–78). Eighteen patients were older than 60. Patients’ age distribution is summarized in Fig. 1.
In all of the cases, a histological diagnosis is available: 20 primary tumors, 15 of which recurrent, 14 metastases, and 8 of them recurrent (Table 1). All cases were submitted to clinical and imaging studies including standard radiograms, CT scan, and MRI and primary tumors were staged according to Enneking staging system [3].
Extension of fixation ranged from three levels (two couple of screws, with or without anterior column reconstruction) to eight levels. Total number of implanted screws was 232.
The construct involved the thoracic spine in 5, the lumbar spine in 2, the thoraco-lumbar junction in 19, and the lumbo-sacral junction in 8.
Details of surgical technique of implanting, incidence of complications (intra- and post-operative), changes in neurological status, local control (LC), and local recurrence (LR) were recorded. The neurologic function was evaluated according to the ASIA score and local pain by visual analogic scale (VAS) score at the admission and at discharge.
All the cases were submitted to post-op CT scan and standard radiograms before discharge. Periodical follow-up clinical and radiographic controls performed by the surgeons’ team were performed at 3, 6, and 12 months and each year later to assess implant stability and possible tumor recurrence.
Close contacts with the radiation oncologists were kept to record their opinion during treatment planning and execution.
Results
Intraoperative findings
The surgical technique of pedicle screw introduction is the same as for titanium screw. To take advantage of full radiolucency to minimize radiographic/radiotherapy interference, full composite screw without any metallic component was preferred in this study. These screws are radiotransparent and positioning cannot be verified by the standard intraoperative radiograms, while intraoperative CT scan allows.
However, the producer can provide both screws covered by a thin layer of titanium and screws including a titanium small reference point at the tip.
The connection screw/rod could not be achieved by the usual fixation by set screw as CFR-PEEK composite is brittle and such a kind of connection cannot be manufactured. Connection can be achieved by a special device impacting a small component fixed on the rod into the screw collar. Furthermore, the rod contour cannot be changed on the operative field. These two technical requirements make the surgical technique not user-friendly and careful education and training are needed.
Only one intraoperative complication occurred: a screw breakage during the third surgical procedure of the series. This occurred while replacing a thinner titanium screw without reaming the pedicle with the diameter of the composite screw.
Early (0–7 days) post-operative findings
Weight bearing was encouraged in the immediate post-operative course for all the patients without orthosis.
Only one patient complained radicular pain: the CT scan showed the malpositioning of a sacral screw impinging the S1 nerve root in the foramen. Immediate revision was performed with correct re-positioning, followed by pain resolution without motor weakness.
Pre-operative ASIA score was: B in 1 patient, C in 3 patients, D in 5 patients, and E in 25 patients. At the discharge, ASIA score changed in three patients: two pre-operative C became D and one pre-operative D became E; in the other patients, the score has not changed.
The mean VAS score decreased from a pre-operative of 2.7 (±2.3 SD, range 0–8) to a post-operative of 0.3 (±0.6 SD, range 0–2).
Late (second week to the last follow-up) post-operative findings
No patient was lost to follow-up. No rod breakage, neither any screw/rod disconnection was found during the considered follow-up (Figs. 2, 3). Two cases of loosening of sacral screws were found at 9 and 12 months in two different patients submitted to previous surgery and revised with CFR-PEEK screws. The constructs were, respectively, composed by four and five levels. These were multirecurrent malignant tumors and loosening was found at the time of the local recurrence provoking instability of the construct.
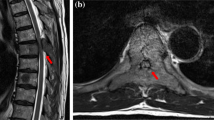
a Male, 71 years. L4 osteosarcoma. Pre-operative CT scan. Cauda syndrome, unable to walk. Chemotherapy not allowed due to severe cardiopathy. Only short surgery allowed. b Male, 71 years L4 osteosarcoma. Intralesional intracapsular tumor excision and posterior fixation with CFR-PEEK implant. Post-operative CT. c Male, 71 years L4 osteosarcoma. Intralesional intracapsular tumor excision and posterior fixation with CFR-PEEK implant, followed by carbon ion therapy (76 Gy). One year follow-up. Walking with canes, no pain. Ossification of the lytic areas
a Female, 42 years. L1 hemangioendothelioma. Submitted elsewhere to palliative posterior decompression (supposed diagnosis of metastasis). b Female, 42 years. L1 hemangioendothelioma. Gross-total double approach excision. Posterior fixation by CFR-PEEK composite implant. Intraoperative image. c Female, 42 years. L1 hemangioendothelioma. Posterior fixation by CFR-PEEK composite implant; anterior reconstruction by CFR-PEEK composite cage filled with autogenous bone cheaps. Radiotherapy (44 Gy). d Female, 42 years. L1 hemangioendothelioma. Gross-total double approach excision. Reconstruction by anterior and posterior CFR-PEEK composite implants. Radiotherapy. 2D CT reconstruction at 10 months follow-up. No tumor recurrence. Full implants stability. Fusion of the graft
The overall number of LR was 6: these were immediately detected thanks to implant radiolucency.
No infection occurred.
Discussion
The main features of composite CFR-PEEK spine stabilization systems, related to the use in tumor surgery, are radiolucency and the ability to minimize interference with ionizing radiation including particles. These features are presumed to be associated with at least the same mechanical performances of titanium.
Radiolucency is particularly helpful during follow-up imaging studies: the use of CFR-PEEK spine stabilization systems, thanks to the optimal visualization of the bone and soft-tissue structures also in the close proximity, allows a best post-operative assessment and is helpful to identify any early tumor regrowth.
Highly conformal radiotherapy with particles (protons and ions) is mostly recommended in the treatment of spinal tumors because of its intrinsic physical selectivity allowing delivery of a high dose to the tumor (or tumor bed) sparing surrounding healthy tissues.
In particular, particle therapy increasing the probability of local control as its physical selectivity allows achieving steep dose gradients and delivery of high doses even to targets in close proximity to the spinal cord. It is well known that the spinal cord is the most important organ at risk in this anatomical district because of a low tolerance limiting delivery of curative high dose to the tumors.
Artifacts in CT imaging caused by metallic hardware used for fixation or reconstruction affect not only contouring precision but even more significantly hinder precise range calculation of delivered particles and introduce a high degree of uncertainties in calculating dose distributions. Metallic implants significantly differ from normal tissues in terms of density and composition producing substantial perturbation effects.
In some series, the presence of metallic hardware was the strongest predictive factor for local recurrences in spinal tumors treated with particle therapy [27].
In general, the irradiation through metal implants should be avoided in proton and carbon-ion therapy.
Experimental data by Monte Carlo simulations and TLD measurements show that carbon plates will neither increase the incident surface dose nor lead to the decrease of exit surface dose (the effect of a second build-up) using six MV photons [28]. Contouring and range calculation for patients with CFR-PEEK stabilization devices show almost negligible image artifacts reducing contouring uncertainties and increasing the accuracy of dosimetric treatment planning [25]. CFR-PEEK stabilization devices are more suitable than commonly used titanium devices in patients eligible for particle therapy. The absence of image artifacts and, consequently, the reduction in contouring, together with significantly less dose perturbation, improve the dosimetric treatment planning accuracy and plan robustness against setup and range uncertainties [29].
A disadvantage of the CFR-PEEK system is the inability to contour the rods intra-operatively, thus making the use more demanding when compared with the standard titanium devices. Moreover, this issue may affect spinal alignment and further study is needed. However, the preliminary results of this cohort of patients did not show a number of mechanical adverse events superior to those reported in the literature and commonly observed with titanium implants [30]. Conversely, according to the radiation oncologists’ opinion, the patients who received this implants had an easier CT planning of radiotherapy and the radiotherapy course was performed without the side effect of radiation scattering.
A limitation of the study is the relatively small number of patients. Another bias of the study is the use of different materials for the reconstruction of the anterior column. Especially, in patients with titanium, cage or acrylic cement may occur artifacts during RT, thus reducing the advantage of CFR-PEEK system.
Conclusions
From the data of this preliminary report, it seems that the clinical use of CFR-PEEK composite implants for fixation in the thoracic and lumbar spine may be safe and at least comparable with the commonly used titanium implants in terms of intraoperative complications, stability at weight bearing and at functional recovery.
The use of these fully radiolucent implants, thanks to the optimal visualization of the bone and soft-tissue structures also in the close proximity, allows identifying any early tumor regrowth by imaging studies.
The radiation oncologists’ opinion confirms that composite implants, thanks to their low atomic number, have radiation properties similar to those of biological tissues, and therefore, they are more suitable to patient’s candidates for radiotherapy.
The advantage of using CFR-PEEK composite implants in terms of overall results and patients’ outcome needs to be prospectively defined with larger patient series and longer follow-up analysing the site of recurrences.
In this perspective, even the final prognosis could be positively affected by combination of less aggressive surgery and appropriate courses of radiotherapy.
References
Sharan AD, Szulc A, Krystal J, Yassari R, Laufer I, Bilsky MH (2014) The integration of radiosurgery for the treatment of patients with metastatic spine diseases. Am Acad Orthop Surg 22(7):447–454. doi:10.5435/JAAOS-22-07-447
Campanacci M (1990) Bone and soft tissue tumors. Springer, Berlin. doi:10.1007/978-3-662-29279-2
Enneking WF, Spanier SS, Goodman MA (1980) A system for the surgical staging of musculoskeletal sarcoma. Clin Orthop Relat Res 153:106–120
Fisher CG, Andersson GB, Weinstein JN (2009) Spine focus issue. Summary of management recommendations in spine oncology. Spine (Phila Pa 1976) 34(22 Suppl):S2–S6. doi:10.1097/BRS.0b013e3181baae29
Tomita K, Kawahara N, Baba H, Tsuchiya H, Nagata S, Toribatake Y (1994) Total en bloc spondylectomy for solitary spinal metastases. Int Orthop 18(5):291–298
Stener B (1989) Complete removal of vertebrae for extirpation of tumors. A 20-year experience. Clin Orthop Relat Res 245:72–82
Kato S, Murakami H, Demura S, Yoshioka K, Ota T, Shinmura K, Yokogawa N, Kawahara N, Tomita K, Tsuchiya H (2013) Patient and family satisfaction with en bloc total resection as a treatment for solitary spinal metastasis. Orthopedics 36(11):e1424–e1430. doi:10.3928/01477447-20131021-27
Boriani S, Bandiera S, Donthineni R, Amendola L, Cappuccio M, De Iure F, Gasbarrini A (2010) Morbidity of en bloc resections in the spine. Eur Spine J 19(2):231–241. doi:10.1007/s00586-009-1137-z
Boriani S, Weinstein JN, Biagini R (1997) Primary bone tumors of the spine. Terminology and surgical staging. Spine (Phila Pa 1976) 22(9):1036–1044 (review)
Boriani S, Gasbarrini A, Bandiera S, Ghermandi R, Lador R (2016) En bloc resections in the spine—the experience of 220 cases over 25 years. World Neurosurg. doi:10.1016/j.wneu.2016.10.086
Charest-Morin R, Dea N, Fisher CG (2016) Health-related quality of life after spine surgery for primary bone tumour. Curr Treat Options Oncol 17(2):9. doi:10.1007/s11864-015-0383-z (review)
Chang UK, Lee DH, Kim MS (2014) Stereotactic radiosurgery for primary malignant spinal tumors. Neurol Res 36(6):597–606. doi:10.1179/1743132814Y.0000000381
Stacchiotti S, Sommer J, Chordoma Global Consensus Group (2015) Building a global consensus approach to chordoma: a position paper from the medical and patient community. Lancet Oncol 16(2):e71–e83. doi:10.1016/S1470-2045(14)71190-8
Germscheid NM, Fisher CG (2016) Focus issue II in spine oncology: compendium of spine oncology recommendations. Spine (Phila Pa 1976) 41(Suppl 20):S163–S170
Patchell RA, Tibbs PA, Regine WF, Payne R, Saris S, Kryscio RJ, Mohiuddin M, Young B (2005) Direct decompressive surgical resection in the treatment of spinal cord compression caused by metastatic cancer: a randomised trial. Lancet 366(9486):643–648
Bilsky MH, Laufer I, Burch S (2009) Shifting paradigms in the treatment of metastatic spine disease. Spine (Phila Pa 1976) 34(22 Suppl):S101–S107. doi:10.1097/BRS.0b013e3181bac4b2 (review)
Sahgal A, Bilsky M, Chang EL, Ma L, Yamada Y, Rhines LD, Létourneau D, Foote M, Yu E, Larson DA, Fehlings MG (2011) Stereotactic body radiotherapy for spinal metastases: current status, with a focus on its application in the postoperative patient. J Neurosurg Spine 14(2):151–166. doi:10.3171/2010.9.SPINE091005 (review)
Zuckerman SL, Laufer I, Sahgal A, Yamada YJ, Schmidt MH, Chou D, Shin JH, Kumar N, Sciubba DM (2016) When less is more: the indications for mis techniques and separation surgery in metastatic spine disease. Spine (Phila Pa 1976) 41(Suppl 20):S246–S253
Brantigan JW, McAfee PC, Cunningham BW, Wang H, Orbegoso CM (1994) Interbody lumbar fusion using a carbon fiber cage implant versus allograft bone. An investigational study in the Spanish goat. Spine (Phila Pa 1976) 19(13):1436–1444
Boriani S, Biagini R, Bandiera S, Gasbarrini A, De Iure F (2002) Reconstruction of the anterior column of the thoracic and lumbar spine with a carbon fiber stackable cage system. Orthopedics 25(1):37–42
Morelli C, Barbanti-Brodano G, Ciannilli A, Campioni K, Tognon M (2007) Cell morphology, markers, spreading, and proliferation on orthopaedic biomaterials. An innovative cellular model for the “in vitro” study. J Biomed Mater Res A 83(1):178–183
Kersten RF, van Gaalen SM, de Gast A, Öner FC (2015) Polyetheretherketone (PEEK) cages in cervical applications: a systematic review. Spine J 15(6):1446–1460. doi:10.1016/j.spinee.2013.08.030 (review)
Boriani S, Bandiera S, Biagini R (2006) Vertebral resection and reconstruction using the stackable cage system. In: Brantigan JW, Lauryssen C (eds) Intervertebral fusion using carbon fiber reinforced polymer implants. Quality Medical Publishing, St. Louis
Jackson JB 3rd, Crimaldi A, Peindl R, Norton HJ, Anderson WE, Patt JC (2016) The effect of polyether ether ketone on therapeutic radiation to the spine—a pilot study. Spine (Phila Pa 1976) 42(1):E1–E7. doi:10.1097/BRS.0000000000001695
Zimel MN, Hwang S, Riedel ER, Healey JH (2015) Carbon fiber intramedullary nails reduce artifact in postoperative advanced imaging. Skelet Radiol 44(9):1317–1325. doi:10.1007/s00256-015-2158-9
Zoccali C, Soriani A, Rossi B, Salducca N, Biagini R (2016) The Carbofix™ “piccolo proximal femur nail”: a new perspective for treating proximal femur lesion. A technique report. J Orthop 13(4):343–346. doi:10.1016/j.jor.2016.07.001
Rutz HP, Weber DC, Sugahara S, Timmermann B, Lomax AJ, Bolsi A, Pedroni E, Coray A, Jermann M, Goitein G (2007) Extracranial chordoma: outcome in patients treated with function-preserving surgery followed by spot-scanning proton beam irradiation. Int J Radiat Oncol Biol Phys 67(2):512–520
Xin-ye N, Xiao-bin T, Chang-ran G, Da C (2012) The prospect of carbon fiber implants in radiotherapy. J Appl Clin Med Phys 13(4):3821. doi:10.1120/jacmp.v13i4.3821
Bar-Deroma R, Borzov E, Nevelsky A, Daniel S (2015) Perturbation effects of carbon fiber-PEEK screws on radiotherapy dose distribution. ESTRO Forum. doi:10.1016/S0167-8140(15)40850-3 (PO-0858)
Nasser R, Yadla S, Maltenfort MG, Harrop JS, Anderson DG, Vaccaro AR, Sharan AD, Ratliff JK (2010) Complications in spine surgery. J Neurosurg Spine 13(2):144–157. doi:10.3171/2010.3.SPINE09369
Acknowledgements
The AA thanks Cristiana Griffoni for their incomparable work for data collection and editing and Carlo Piovani for his activity in imaging storage and elaboration.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Boriani, S., Tedesco, G., Ming, L. et al. Carbon-fiber-reinforced PEEK fixation system in the treatment of spine tumors: a preliminary report. Eur Spine J 27, 874–881 (2018). https://doi.org/10.1007/s00586-017-5258-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-017-5258-5