Abstract
Purpose
The aim of the study is to assess and quantify the effectiveness of interbody lordotic cages applied by trans-psoas approach to improve radiographic parameters, showing the differences between completely mini-invasive and hybrid approach.
Methods
We collected data of 65 patients affected by degenerative lumbar deformity/diseases and underwent mini-invasive lateral interbody fusion followed by percutaneous (group A, completely mini-invasive) or open (group B, hybrid) posterior instrumentation. A subgroup underwent anterior column realignment (ACR). We assessed statistical differences in preoperative and postoperative (at least 6-month) coronal and sagittal parameters, and disc angle (DA) at each level of cage application.
Results
107 lordotic cages were implanted. Group B had the most significant mean changes, especially in coronal Cobb angle, sagittal vertical axis, lumbar lordosis (LL), pelvic incidence-LL mismatch and DA. Concerning DA, at each level of lordotic cage application, in group A changed from −2.9° preop to −6.5° postop (p = 0.01); in group B, DA changed from −2.6° to −9.5° (p = 0.002) and from +1° to −13.2° in patients underwent ACR.
Conclusions
Minimally invasive lateral lumbar interbody fusion is an effective technique in improving sagittal parameters. When combined with posterior open approach and/or application of ACR procedure greater corrections are possible.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The goals of spinal deformity surgery include the decompression of neural elements, the restoration of sagittal and coronal spinal balance and promotion of arthrodesis, to improve debilitating symptoms and patients quality of life. Minimally invasive surgery (MIS) is becoming an alternative tool in the treatment of adult spinal deformity (ASD) with the aim to reduce perioperative complications due to surgical access morbidity. Several techniques and surgical approaches have been described. The effect of retroperitoneal lateral lumbar interbody fusion (LLIF) on sagittal balance and spino-pelvic parameters seems to be significantly enhanced when combined with a posterior approach [1,2,3,4]. However, patients with moderate–severe deformity, fixed sagittal imbalance and spino-pelvic malalignment are poor candidates for MIS surgery alone and often require a hybrid MIS + open approach or open posterior osteotomies [5]. In this contest, while it seems to be demonstrated that interbody cage application produces significant increase in average disk height, foraminal and canal area [6,7,8,9], the degree of correction achieved on radiographic parameters by lordotic cages is not well defined, even after the anterior longitudinal ligament release.
The aim of this study is to assess and quantify the effectiveness of interbody lordotic cages applied by minimally invasive trans-psoas approach to improve radiographic parameters, especially with respect sagittal parameters such as lumbar lordosis and segmental lordosis [disc angle (DA)], showing the differences between the values obtained through the completely mini-invasive and hybrid approach.
Materials and methods
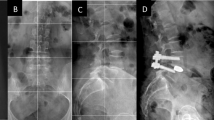
Two institutions and three surgeons with experience in minimally invasive spinal surgery were involved in this study. The authors retrospectively reviewed demographic, surgical and radiographic database about all patients underwent surgical treatment at our Institutions for adult spine deformity and degenerative spinal diseases, such as adult degenerative scoliosis, kyphos-scoliosis, lumbar kyphosis, and degenerative instability-spondylolisthesis. We included patients older than 40 years and treated by minimally invasive retroperitoneal lateral trans-psoas approach, with at least one-level lateral lumbar interbody fusion (LLIF) through lordotic cage (10°) as described by Pimenta et al. [10], and/or anterior column realignment technique (ACR) with anterior longitudinal ligament release and application of trans-psoas hyperlordotic cage (20°), using the technique described by Akbarnia et al. [11]. Patients with stand-alone procedure and without additional posterior instrumentation were excluded. Only patients with good quality preoperative and at least 6-month postoperative radiographic data were included. Subsequently, the 65 enrolled patients were divided in two groups: completely minimally invasive surgery group (group A—27 patients), in which patients underwent lateral retroperitoneal trans-psoas approach to the lumbar spine according to standard XLIF procedure, combined with percutaneous posterior fixation using bilateral pedicle screws and rods, putting patient in prone or lateral position in the same anesthesia (Fig. 1); hybrid surgery group (group B—38 patients), in which patients received supplementary open posterior approach with the addition of various degrees of segmental decompression, minor posterior column osteotomies (facetectomy or Smith–Petersen osteotomy) and fixation using bilateral pedicle screws and rods. In this last group, patients underwent ACR procedures were distinguished in a subgroup (Fig. 2). Compression was applied posteriorly, in every case, at the interbody cage application level. All procedures were done under continuous neuromonitoring.
Radiographic measurements were done on preoperative and at least 6-month postoperative anterior–posterior and lateral full-standing X-ray of the spine by two independent operators. The following radiographic parameters were assessed: coronal Cobb of the scoliotic curve; thoracic kyphosis (TK); lumbar lordosis (LL); sacral slope (SS); pelvic tilt (PT); pelvic incidence (PI); PI–LL mismatch. To assess and quantify the effective role of lordotic cages to improve sagittal parameters, we measured preoperative and postoperative DA at each level of cage application, calculated as the angle between the lower endplate of the upper vertebra and the upper endplate of the lower vertebra, referring to lordosis as a negative value and to kyphosis as a positive value (Fig. 3). We also measured preoperative and postoperative DA variation (DAv) both in cMIS and hybrid group.
Student’s t test was applied to assess any difference between parametric data. For non-parametric data, Mann–Whitney test (SPSS statistics software) was used, with a level of significance of 0.05.
Results
Sixty-five patients had a complete and good quality data set and were enrolled in this study. Completely minimally invasive surgery approach was performed in 27 patients (group A—41.5%), while 38 patients (group B—58.5%) underwent hybrid surgery. The mean age was 62.4 years (40–81), mostly women (49 F, 16 M) with a mean BMI of 24.9 (16.6–29.6). Demographic and surgical differences between two groups are reported in Table 1. Mean follow-up was 13 months (6–19). Admitting diagnosis were adult degenerative scoliosis (26 patients—40%), lumbar stenosis-instability with deformity in sagittal and/or coronal plane (15 patients—23.1%), thoracic-lumbar kyphosis (24 patients—36.9%). Ten patients had prior lumbar spine surgery (15.3%). Instrumented vertebrae were in mean 7.2 (range 2–16) for patient, 3.2 (2–5) in group A and 10.1 (4–16) in group B, with a total number of 107 cages implanted (103°–10°, 4°–20°) through the lateral trans-psoas approach. The mean cages for patient were 1.7 (1–3). In group B, a subgroup of four patients (6.1%) underwent ACR procedure, with resection of ALL and application of 20° lordotic cage. In Table 2, we reported levels of cages application.
Mean radiographic data (Table 3) in group A—cMIS changed as follow: max coronal Cobb angle from 8.7° preop to 4.2 postop (p = 0.003), TK from 32.2° preop to 38° (p = 0.03), LL from 41.4° preop to 46.5° postop (p = 0.07), SVA from 24.8° preop to 21° postop (p = 0.04), SS from 30.3° to 33.5° (p = 0.08) PT from 18.2° to 15.1° (p = 0.03), and PI–LL mismatch from 8.2° to 4.2° (p = 0.02), Table 4. In group B—hybrid, max coronal Cobb angle improved from 32.7° preop to 11.6 postop (p = 0.001), TK from 30.6° to 35.3° (p = 0.04), LL from 36.9° preop to 46° postop (p = 0.01), SVA from 56.5° to 39.3° (p = 0.003), SS from 29.7° to 32° (p = 0.06), PT from 26.3° to 20.1° (p = 0.001), and PI–LL mismatch from 17.7° to 10.4° (p = 0.001) (Table 5).
In group A, DA at each level of cage application changed from a mean preoperative value of −2.9° to −6.5° postop (p = 0.01) with mean DAv of 3.6° (p = 0.01); in group B, DA changed from −2.6° to −9.5°, with mean DAv of 6.9° (p = 0.002). In the subgroup underwent ACR procedure with application of 20° lordotic cage, DA changed from a mean preop value of +0.7° to −13.2° postop, with mean DAv of −14.2° (Table 6); LL improved from a mean value of 22.6° preop to 45.9° postop.
Discussion
Adult spinal deformity is one of the most important topics for spinal surgeons owing to its various clinical presentations and radiographic patterns, challenging treatment and significant impact on quality of life, especially with the advancement of aging society. Surgical management may be started for patients that despite conservative treatment have progressive and debilitating symptoms. The main goal of ASD surgery is to obtain balanced spine with low morbidity and mortality rate [12].
Schwab et al. demonstrated that the radiographic parameters having the strongest correlations with disability and quality of life are all sagittal measurements. Specifically, SVA, PT and the mismatch between the LL and the PI can predict patient disability and provide a guide for patient assessment for appropriate therapeutic decision making [13]. Others studies emphasize the critical importance of sagittal spino-pelvic alignment and provide radiographic objectives for surgical correction [14,15,16]. Traditional open surgery (like Smith–Petersen osteotomy, pedicle subtraction osteotomy, vertebral column realignment) showed good correction of coronal and sagittal parameters, but it is associated with high complications and morbidity rate.
In recent years, minimally invasive approaches have been developed as alternative methods to avoid the complications of traditional open surgery. Percutaneous techniques may be helpful to reduce approach-related morbidity [17]. Lateral lumbar interbody fusion (LLIF) was first time introduced by Pimenta et al. in the year 2006 [10]. General indications for this approach included mainly neurogenic claudication and radicular symptoms with the history of chronic low back pain, and the objective of the surgery was indirect decompression [18]; however, it is now used to treat a multitude of conditions, including degenerative deformity, disc disease, spondylolisthesis, foraminal stenosis, tumor and trauma [5]. Nowadays, in adult spinal deformity, LLIF is widely used alone [1] or more frequently associated with additional surgical procedures [2, 3, 9, 11]. “Completely” or “circumferential” MIS (cMIS), involves 360° deformity correction with anterior column support (interbody cage placement) and posterior percutaneous instrumentation through an entirely MIS approach. Hybrid surgery most frequently refers to LLIF in combination with traditional open posterior surgery that includes segmental decompression, minor osteotomies, instrumentation and fusion [19]. Others MIS techniques can be associated with these approaches to obtain greater correction. Anterior column realignment (ACR) involves the combination of lateral lumbar discectomy/osteophytectomy, anterior longitudinal ligament (ALL) release, and placement of hyperlordotic cage. Discectomy and contralateral annulus release are essential to ensure symmetrical distraction, proper bilateral decompression, and deformity correction and to isolate and facilitate a safe division of the ALL. Recent studies demonstrated that ACR is effective in correcting sagittal plane deformity and suggested this technique as an alternative tool than traditional open posterior three-column osteotomy, associated with significant risk of complications [9, 11, 20, 21].
Only few recent studies have compared cMIS and hybrid surgery for the treatment of adult spinal deformity. Park et al. [22], in a series of 105 consecutive patients, demonstrated that both these approaches are effective for correcting sagittal deformity and improving quality of life. Hybrid group, however, demonstrated greater improvement in radiographic parameters, especially coronal Cobb, lumbar lordosis and PI–LL mismatch, but higher complication rate compared with the cMIS group (55 vs. 33%). Wang et al. [4] demonstrated a major complication rate of 40% in 35 patients undergoing hybrid surgery compared with 14% in the cMIS group (43 patients). Both groups had improvement of quality of live scores and significant reduction of coronal Cobb angle. However, the two studies mentioned above did not investigate the segmental lordosis obtained at each level of cage application.
Our study provides a large and detailed series to clarify radiographic outcomes obtained by completely MIS and hybrid approach in ASD treatment; in addition, the authors quantify the real contribution of the lordotic cages to improve sagittal parameters. In our practice, generally, we performed hybrid treatment to patients with more severe deformities, according to the principles reported by Mummaneni et al. [23]. In particular, with a coronal Cobb > 20° and/or SVA > 6 cm and/or PT > 25° and/or PI–LL > 10°, we applied more invasive techniques through additional posterior open surgery. Both approaches confirmed good effectiveness of LLIF to obtain coronal deformity correction, probably due to discectomy, contralateral annulus release and distraction across disc space. Obviously, due to the greater number of instrumented levels and to the open posterior procedures, in group B we obtained greater variations of radiographic parameters, especially SVA (−3.8 vs. −17.2 mm), PT (−3.1° vs. −6.2°) and PI–LL mismatch (−4° vs. −7.3°).
The effectiveness of interbody lordotic cages on segmental lordosis was greater in group B than group A (DAv = 6.9° vs. 3.6°), in which minor posterior column osteotomy and compression were performed. The mean change in DA value obtained through ACR procedure and 20° lordotic cage application (14.2°) was more significantly than those achieved with LLIF alone; however, the two groups are completely different in size and therefore difficult to compare in statistic way; a more consistent ACR subgroup will be necessary for an accurate and significant assessment.
Although with the same surgical techniques, the surgeries were performed by three orthopedic surgeons in two different spinal surgery divisions; this represents a potential bias of the study. Furthermore, the retrospective study design and the non-randomized patient’s selection represent further limitations.
Conclusions
Minimally invasive lateral lumbar interbody fusion is an effective technique in improving sagittal parameters, especially sagittal vertical axis, lumbar lordosis, pelvic tilt and PI–LL mismatch. When combined with posterior open approach and/or anterior column realignment procedure, greater corrections are possible. Lordotic cages application showed best effectiveness to restore DA and lordosis when hybrid approach and anterior longitudinal ligament release were performed. In future work, we intend to analyze the clinical results and the complications associated with these approaches.
References
Castro C, Oliveira L, Amaral R et al (2014) Is the lateral transpsoas approach feasible for the treatment of adult degenerative scoliosis? Clin Orthop Relat Res 472(6):1776–1783
Sharma A, Kepler C, Girardi F et al (2011) Lateral lumbar interbody fusion: clinical and radiographic outcomes at 1 year: a preliminary report. J Spinal Disord Tech 24(4):242–250
Acosta F, Liu J, Slimack N et al (2011) Changes in coronal and sagittal plane alignment following minimally invasive direct lateral interbody fusion for the treatment of degenerative lumbar disease in adults: a radiographic study. J Neurosurg Spine 15(1):92–96
Wang MY, Mummaneni PV, Fu G et al (2014) Less invasive surgery for treating adult spinal deformities: ceiling effects for deformity correction with 3 different techniques. Neurosurg Focus 36:E12
Tempel ZJ, GanDhoke GS, Bonfiel CM, Okonkwo DO, Kanter AS (2014) Radiographic and clinical outcomes following combined lateral lumbar interbody fusion and posterior segmental stabilization in patients with adult degenerative scoliosis. Neurosurg Focus 36(5):E11 (©AANS)
Alimi M, Hofstetter CP, Tsiouris AJ, Elowitz E, Härtl R (2015) Extreme lateral interbody fusion for unilateral symptomatic vertical foraminal stenosis. Eur Spine J 24 Suppl 3:346–352
Khajavi K, Shen AY (2014) Two-year radiographic and clinical outcomes of a minimally invasive, lateral, transpsoas approach for anterior lumbar interbody fusion in the treatment of adult degenerative scoliosis. Eur Spine J 23(6):1215–1223
Kepler CK, Sharma AK, Huang RC, Meredith DS, Girardi FP et al (2012) Indirect foraminal decompression after lateral transpsoas interbody fusion. J Neurosurg Spine 16(4):329–333
Marchi L, Oliveira L, Amaral R, Castro C, Coutinho T, Coutinho E, Pimenta L (2012) Anterior elongation as a minimally invasive alternative for sagittal imbalance—a case series. HSS J 8:122–127
Ozgur BM, Aryan HE, Pimenta L, Taylor WR (2006) Extreme Lateral Interbody Fusion (XLIF): a novel surgical technique for anterior lumbar interbody fusion. Spine J 6:435–443
Akbarnia BA, Mundis GM, Moazzaz P et al (2014) Anterior column realignment (ACR) for focal kyphotic spinal deformity using a lateral transpsoas approach and ALL release. J Spinal Disord Tech 27(1):29–39
Taneichi Hiroshi (2016) Update on pathology and surgical treatment for adult spinal deformity. J Orthop Sci 2:116–123
Schwab FJ, Blondel B, Bess S, Hostin R, Shaffrey CI et al (2013) Radiographical spinopelvic parameters and disability in the setting of adult spinal deformity. Spine 38(13):E803–E812
Glassman SD, Bridwell K, Dimar JR et al (2005) The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976) 30:2024–2029
Schwab F, Lafage V, Patel A et al (2009) Sagittal plane considerations and the pelvis in the adult patient. Spine (Phila Pa 1976) 34:1828–1833
Lafage V, Bharucha NJ, Schwab F et al (2012) Multicenter validation of a formula predicting postoperative spinopelvic alignment. J Neurosurg Spine 16:15–21
Logroscino CA, Proietti L, Pola E, Scaramuzzo L, Tamburrelli FC (2011) A minimally invasive posterior lumbar interbody fusion for degenerative lumbar spine instabilities. Eur Spine J 20(Suppl 1):S41–S45
Pimenta L, Fortti F, Oliveira L, Marchi L, Jensen R et al (2015) Anterior column realignment following lateral interbody fusion for sagittal deformity correction. Eur J Orthop Surg Traumatol 25(Suppl 1):S29–S33
Kanter AS, Tempel ZJ, Ozpinar A, Okonkwo DO (2016) A review of minimally invasive procedures for the treatment of adult spinal deformity. Spine 41(8S):S59–S65
Berjano P, Cecchinato R, Sinigaglia A, Damilano M, Ismael MF et al (2015) Anterior column realignment from a lateral approach for the treatment of severe sagittal imbalance: a retrospective radiographic study. Eur Spine J 24(suppl 3):433–438
Turner JD, Akbarnia BA, Eastlack RK, Bagheri R, Nguyen S et al (2015) Radiographic outcomes of anterior column realignment for adult sagittal plane deformity: a multicenter analysis. Eur Spine J 24(Suppl 3):S427–S432
Park P, Wang MY, Lafage V, Nguyen S, Ziewacz J et al (2015) Comparison of two minimally invasive surgery strategies to treat adult spinal deformity. J Neurosurg Spine 22:374–380
Mummaneni PV, Shaffrey CI, Lenke LG, Park P, Wang MY et al (2014) The minimally invasive spinal deformity surgery algorithm: a reproducible rational framework for decision making in minimally invasive spinal deformity surgery. Neurosurg Focus 36(5):E6
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no potential conflict of interest.
Rights and permissions
About this article
Cite this article
Barone, G., Scaramuzzo, L., Zagra, A. et al. Adult spinal deformity: effectiveness of interbody lordotic cages to restore disc angle and spino-pelvic parameters through completely mini-invasive trans-psoas and hybrid approach. Eur Spine J 26 (Suppl 4), 457–463 (2017). https://doi.org/10.1007/s00586-017-5136-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-017-5136-1