Abstract
Purpose
Current standard methods to quantify disc height, namely distortion compensated Roentgen analysis (DCRA), have been mostly utilized in the lumbar and cervical spine and have strict exclusion criteria. Specifically, discs adjacent to a vertebral fracture are excluded from measurement, thus limiting the use of DCRA in studies that include older populations with a high prevalence of vertebral fractures. Thus, we developed and tested a modified DCRA algorithm that does not depend on vertebral shape.
Methods
Participants included 1186 men and women from the Framingham Heart Study Offspring and Third Generation Multidetector CT Study. Lateral CT scout images were used to place 6 morphometry points around each vertebra at 13 vertebral levels in each participant. Disc heights were calculated utilizing these morphometry points using DCRA methodology and our modified version of DCRA, which requires information from fewer morphometry points than the standard DCRA.
Results
Modified DCRA and standard DCRA measures of disc height are highly correlated, with concordance correlation coefficients above 0.999. Both measures demonstrate good inter- and intra-operator reproducibility. 13.9 % of available disc heights were not evaluable or excluded using the standard DCRA algorithm, while only 3.3 % of disc heights were not evaluable using our modified DCRA algorithm.
Conclusions
Using our modified DCRA algorithm, it is not necessary to exclude vertebrae with fracture or other deformity from disc height measurements as in the standard DCRA. Modified DCRA also yields identical measurements to the standard DCRA. Thus, the use of modified DCRA for quantitative assessment of disc height will lead to less missing data without any loss of accuracy, making it a preferred alternative to the current standard methodology.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Back pain is a highly prevalent and costly condition, with a total cost, both direct and indirect, of more than $100 billion annually in the US [1]. Intervertebral disc (IVD) degeneration is commonly associated with back pain, morbidity, and increased mortality [2, 3]. Clinically, semi-quantitative techniques are used to describe the prevalence and progression of IVD degeneration and loss of disc height. These techniques are generally based on magnetic resonance imaging (MRI) [4], but they have also been applied to computed tomography (CT) images and lateral spine radiographs [5, 6]. Semi-quantitative evaluations of IVD degeneration may be insufficient for tracking the prevalence and progression of the condition [7]. Thus, various methods have been proposed for quantification of IVD height using vertebral morphometry data [8, 9].
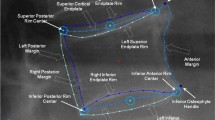
Vertebral morphometry, often used in vertebral fracture assessment, involves the placement of points on the superior and inferior vertebral margins, commonly six points (Fig. 1a). The early studies assessed disc height as the distance between vertebral endplates on adjacent vertebrae [10]. However, this overestimates IVD height in cases where adjacent vertebral bodies are misaligned in the sagittal plane (i.e., spondylolisthesis). Several recent studies have continued to use this method, even in the cases of spondylolisthesis [11, 12]. To correct for sagittal plane displacement, Frobin et al. [8] developed distortion compensated Roentgen analysis (DCRA). DCRA takes into consideration the shape and position of adjacent vertebral bodies to more accurately assess IVD height and has become a standard of measure in studies describing IVD height (Fig. 1b). However, because vertebral shape directly affects height measurements using this approach, common conditions, such as vertebral fractures (often wedging of the vertebral body) and osteophytes, are exclusion criteria in studies utilizing DCRA, limiting the broad applicability of the technique. Furthermore, because the DCRA algorithm requires morphometry data for two full vertebral bodies, it is sensitive to missing morphometry points, which could be a particular issue in the thoracic spine as overlying ribs often obscure vertebral endplates in lateral radiographic projections. Finally, most studies have focused on the lumbar or cervical spine [13, 14], and more information is needed regarding the reproducibility of morphometry-based thoracic IVD height measures [15].
a Illustration of six-point morphometry and straight-line distances. b Distortion compensated Roentgen analysis (DCRA): corner morphometry points are used to create a midplane line through adjacent vertebrae (solid lines), a line bisecting the midplanes is found (dashed line), and the sum of the perpendicular distances (lines connecting morphometry points and bisecting line) is the resulting disc height. c Modified DCRA (DCRA*) method: midpoints between anterior morphometry points and superior morphometry points at adjacent levels are found (squares), a midline is drawn connecting these points (dashed line), and the sum of perpendicular distances is the resulting disc height. Example anterior, middle, and posterior heights are illustrated here
Methods
Study design and subjects
To address these limitations, we developed and evaluated a modified DCRA method for quantitative assessment of IVD height utilizing the traditional six-point vertebral morphometry. We hypothesized that our method would show good agreement with the traditional DCRA methodology while offering fewer missing data points.
We performed a cross-sectional study of IVD height measurements assessed from lateral computed tomography scout images from individuals aged 50 years and older in the Framingham Heart Study Offspring and Third Generation Multidetector CT Study [16]. Participants included 650 women (mean age 66.5, SD 8.5 years) and 536 men (mean age 66.4, SD 8.8 years). The current study was approved by the Institutional Review Boards of Hebrew SeniorLife and Beth Israel Deaconess Medical Center.
Computed tomography scans
CT scans were acquired using a 64-slice multidetector CT/PET scanner (Discovery VCT, GE Healthcare, Milwaukee, WI, USA). Details of the imaging protocol were previously reported [16, 17]. Scout images were lateral low-energy scanograms spanning from the upper thoracic spine (T4) to the sacrum (S1).
Vertebral morphometry
We used a semi-automated algorithm to identify vertebral morphometry points in the scout images (SpineAnalyzer, Optasia Medical, Cheadle, UK), as previously published [18, 19]. Briefly, users placed points nearest to each vertebral centroid from L4 to T4. The algorithm identified the outer contour of each vertebral body. The operator could then correct and confirm contours. Based on the contours, six morphometry points were automatically placed (Fig. 1a). We and others have previously reported high reliability for vertebral height assessment using this approach [18, 19]. Operators electronically recorded when morphometry points could not be reliably contoured due to overlaid ribs, poor image quality, or metal artifacts.
Disc height calculations
We created custom scripts in MATLAB (The Mathworks, Natick, MA, USA) to process vertebral morphometry data and calculate disc height using three different algorithms: (1) straight-line distance between anterior morphometry points; (2) DCRA [8]; and (3) our modified DCRA method (DCRA*). Briefly, DCRA uses the four corner morphometry points from the two vertebrae adjacent to the disc. A midplane is drawn through each vertebral centroid using those points. A bisectrix divides the midplanes, and the sum of the distances from anterior morphometry points to the bisectrix describes the disc height (Fig. 1b). The DCRA* method utilizes the six vertebral morphometry points directly superior and inferior to the IVD that is being measured (Fig. 1c). First, the anterior and posterior morphometry points from adjacent vertebral bodies are connected and the midpoints of these lines are identified. A midline is then drawn from the posterior midpoint to the anterior midpoint. The sum of the perpendicular distances from both the superior and inferior morphometry points at the anterior, mid, and posterior vertebral body to the midline yields disc heights, respectively (Fig. 1c). The individual anterior, mid, and posterior disc heights could then be averaged, if desired.
Reliability
We determined both inter- and intraobserver reliability of the IVD height measurements by randomly selecting 20 individuals (10 men and 10 women) from the sample, and the 20 images were analyzed twice each by two different operators. We computed disc heights using the three algorithms described above and derived intraclass correlation coefficients (ICC) at each vertebral level T4 through L4.
Statistical analysis
We computed concordance correlation coefficients [20] to evaluate agreement between DCRA and DCRA*. To evaluate the comparability of different algorithms for calculation of disc height, we used linear regression and Bland–Altman plots. All analyses were completed using the MATLAB statistical package.
Results
Reliability
Reliability of IVD height measurements was similar for all three disc height methods. Specifically, intra-operator ICCs were 0.79 and 0.84 for the two operators for DCRA*; 0.78 and 0.84 for DCRA; and 0.77 and 0.80 for straight line. Inter-operator ICC values were 0.85, 0.85, and 0.82 for DCRA*, DCRA, and straight line, respectively. Measurements were generally less reliable in the thoracic spine than in the lumbar spine, especially in the upper thoracic region (Fig. 2).
Agreement between methods for computing disc height
Disc heights calculated by DCRA* were highly correlated with both DCRA and straight line (r 2 > 0.98). However, disc heights computed using the straight-line algorithm expectedly overestimated disc height compared with DCRA and midline methods. Disc height measurements from the DCRA and DCRA* algorithms were virtually identical with a concordance correlation coefficient of 0.9998 for lumbar discs and 0.9997 for thoracic discs (Fig. 3a, c). Bland–Altman plots show very narrow limits of agreement with no association between mean value and difference between disc height measures (Fig. 3b, d).
Missing data
In both DCRA and DCRA*, some disc heights were unevaluable due to issues, such as poor scan quality or ribs obscuring vertebral endplates. These features resulted in 508 unevaluable disc heights via DCRA, 3.6 % of total available discs, and 465 unevaluable disc heights via DCRA*, 3.3 % of discs. Furthermore, in DCRA, 1468 intervertebral discs (10.3 % of total available discs) were adjacent to a vertebral fracture and unevaluable. The vertebral fracture exclusion does not apply to DCRA* method, so these disc heights were evaluated (Fig. 4).
Characterization of missing data using DCRA and DCRA*. Stacked bars represent amount of unevaluable disc heights due to vertebral fracture (light gray), scan quality (medium gray), or lack of visualization due to ribs (dark gray), shown here as a percentage of total discs in the scan region available for measure
Discussion
This study presents an improvement to the DCRA approach for calculating disc heights using vertebral morphometry points, in that it leads to comparable values, but decreases the amount of missing data. We found high concordance and no systematic differences in disc heights between the original and modified DCRA methods, and found high inter- and intra-reader reliability for each approach.
Original DCRA requires all corner morphometry points of two adjacent vertebral bodies to compute a disc height, and the shape of the vertebral body informs disc height calculations. Our modified DCRA* algorithm relies only on the endplates immediately adjacent to the disc of interest, so there is no need to automatically exclude disc height measurements adjacent to a vertebral fracture. This is important, as disc degeneration may be related to altered spine loading and vertebral fractures [21]. In addition, this method could be applied to improve epidemiological studies, as in diabetes [12]. In addition, missing morphometry points from a single endplate would prevent measurement of two different discs in the DCRA analysis. In cases when overlaid ribs obscure a thoracic vertebral endplate, only the disc adjacent to the obscured endplate would be unevaluable with the DCRA* method. By not relying on whole vertebral morphometry, DCRA* markedly reduces the amount of missing data, and this may be especially advantageous in studies that include the thoracic spine.
Though DCRA* reduces the amount of missing disc heights compared with DCRA, it remains subject to missing morphometry points when vertebral endplates are difficult to visualize. In this lateral CT scout data set, roughly 3.3 % of theoretically available disc heights were still missing in DCRA*. If mid-sagittal CT scan reconstructions were available, the interference of structures, such as overlying ribs, could be avoided, but the challenges of superposition will remain an issue for measurements in 2D CT scout views and radiographs. Another potential limitation is that the images used in this study were acquired with subjects lying supine, so we cannot directly address the validity of DCRA* in more clinically relevant standing radiographs, where disc heights may be expected to be lower. However, the method was developed to be applicable to all lateral images of the spine, and we see no reasons why the posture of the subject would influence either the accuracy or utility of the modified DCRA method compared with the standard DCRA approach.
Conclusions
In conclusion, this new method for measuring disc height from 2D lateral spine images offers a robust way to calculate disc heights that is highly correlated with accepted methodology, and eliminates the need to exclude fractured or deformed vertebrae. The method offers excellent reproducibility, can be employed with any lateral 2D images of the spine, can be used with either commercially available semi-automated morphometry software or older manual-morphometry methods, and reduces the amount of missing data compared with currently accepted methodology. Thus, this new DCRA* methodology is preferable for calculating disc height measurements in studies of disc degeneration, particularly in the thoracic spine and in older adults with high prevalence of vertebral fracture and degenerative changes in the vertebral body shape.
References
Katz JN (2006) Lumbar disc disorders and low-back pain: socioeconomic factors and consequences. J Bone Joint Surg Am 88(Suppl 2):21–24. doi:10.2106/JBJS.E.01273
Luoma K, Riihimaki H, Luukkonen R, Raininko R, Viikari-Juntura E, Lamminen A (2000) Low back pain in relation to lumbar disc degeneration. Spine (Phila Pa 1976) 25:487–492
Kraemer J (1995) Natural course and prognosis of intervertebral disc diseases. International Society for the Study of the Lumbar Spine Seattle, Washington, June 1994. Spine (Phila Pa 1976) 20:635–639
Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N (2001) Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine (Phila Pa 1976) 26:1873–1878
Wilke HJ, Rohlmann F, Neidlinger-Wilke C, Werner K, Claes L, Kettler A (2006) Validity and interobserver agreement of a new radiographic grading system for intervertebral disc degeneration: part I. Lumbar spine. Eur Spine J 15:720–730. doi:10.1007/s00586-005-1029-9
Kettler A, Rohlmann F, Neidlinger-Wilke C, Werner K, Claes L, Wilke HJ (2006) Validity and interobserver agreement of a new radiographic grading system for intervertebral disc degeneration: part II. Cervical spine. Eur Spine J 15:732–741. doi:10.1007/s00586-005-1037-9
Yu LP, Qian WW, Yin GY, Ren YX, Hu ZY (2012) MRI assessment of lumbar intervertebral disc degeneration with lumbar degenerative disease using the Pfirrmann grading systems. PLoS One 7:e48074. doi:10.1371/journal.pone.0048074
Frobin W, Brinckmann P, Biggemann M, Tillotson M, Burton K (1997) Precision measurement of disc height, vertebral height and sagittal plane displacement from lateral radiographic views of the lumbar spine. Clin Biomech (Bristol, Avon) 12(Suppl 1):S1–S63
Bilgic S, Sahin B, Sonmez OF, Odaci E, Colakoglu S, Kaplan S, Ergur H (2005) A new approach for the estimation of intervertebral disc volume using the Cavalieri principle and computed tomography images. Clin Neurol Neurosurg 107:282–288. doi:10.1016/j.clineuro.2004.08.001
Amonoo-Kuofi HS (1991) Morphometric changes in the heights and anteroposterior diameters of the lumbar intervertebral discs with age. J Anat 175:159–168
Abu-Leil S, Floman Y, Bronstein Y, Masharawi Y (2016) A morphometric analysis of all lumbar intervertebral discs and vertebral bodies in degenerative spondylolisthesis. Eur Spine J 25:2535–2545. doi:10.1007/s00586-016-4673-3
Agius R, Galea R, Fava S (2016) Bone mineral density and intervertebral disc height in type 2 diabetes. J Diabetes Complicat 30:644–650. doi:10.1016/j.jdiacomp.2016.01.021
Kumar MN, Jacquot F, Hall H (2001) Long-term follow-up of functional outcomes and radiographic changes at adjacent levels following lumbar spine fusion for degenerative disc disease. Eur Spine J 10:309–313
Frobin W, Leivseth G, Biggemann M, Brinckmann P (2002) Vertebral height, disc height, posteroanterior displacement and dens-atlas gap in the cervical spine: precision measurement protocol and normal data. Clin Biomech (Bristol, Avon) 17:423–431
Oner FC, van der Rijt RR, Ramos LM, Dhert WJ, Verbout AJ (1998) Changes in the disc space after fractures of the thoracolumbar spine. J Bone Joint Surg Br 80:833–839
Hoffmann U, Massaro JM, Fox CS, Manders E, O’Donnell CJ (2008) Defining normal distributions of coronary artery calcium in women and men (from the Framingham Heart Study). Am J Cardiol 102:1136–1141
Samelson EJ, Christiansen BA, Demissie S, Broe KE, Louie-Gao Q, Cupples LA, Roberts BJ, Manoharam R, D’Agostino J, Lang T, Kiel DP, Bouxsein ML (2012) QCT measures of bone strength at the thoracic and lumbar spine: the Framingham Study. J Bone Miner Res 27:654–663. doi:10.1002/jbmr.1482
Brett A, Miller CG, Hayes CW, Krasnow J, Ozanian T, Abrams K, Block JE, van Kuijk C (2009) Development of a clinical workflow tool to enhance the detection of vertebral fractures: accuracy and precision evaluation. Spine (Phila Pa 1976) 34:2437–2443
Kim YM, Demissie S, Eisenberg R, Samelson EJ, Kiel DP, Bouxsein ML (2011) Intra-and inter-reader reliability of semi-automated quantitative morphometry measurements and vertebral fracture assessment using lateral scout views from computed tomography. Osteoporos Int 22:2677–2688. doi:10.1007/s00198-011-1530-4
Lin LI (1989) A concordance correlation coefficient to evaluate reproducibility. Biometrics 45:255–268
Adams MA, Pollintine P, Tobias JH, Wakley GK, Dolan P (2006) Intervertebral disc degeneration can predispose to anterior vertebral fractures in the thoracolumbar spine. J Bone Miner Res 21:1409–1416. doi:10.1359/jbmr.060609
Acknowledgments
This study was funded by grants from the National Institutes of Health (R01AG041658, R01AR053986, R01AR41398, and F31AG041629). The Framingham Heart Study is supported by Contract Number HHSN268201500001I from the National Heart, Lung, and Blood Institute (NHLBI) with additional support from other sources. The contents are solely the responsibility of the authors, and do not necessarily represent the views of the NIH, the Framingham Heart Study or the NHLBI.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Allaire, B.T., DePaolis Kaluza, M.C., Bruno, A.G. et al. Evaluation of a new approach to compute intervertebral disc height measurements from lateral radiographic views of the spine. Eur Spine J 26, 167–172 (2017). https://doi.org/10.1007/s00586-016-4817-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-016-4817-5