Abstract
Purpose
Lumbar spinal stenosis in the presence of degenerative spondylolisthesis is generally treated by means of surgery. The role of lumbar decompression without fusion is not clear. Therefore, the aim of this study was to assess whether patients who undergo decompression alone have a favourable outcome without the need for a subsequent fusion.
Methods
This is a prospective cohort study with single blinding of 83 consecutive patients with lumbar stenosis and degenerative spondylolisthesis treated by decompression, without fusion, using a spinous process osteotomy. Blinded observers collected pre- and post-operative Oswestry Disability Index (ODI), EuroQol Five Dimensions (EQ-5D), and visual analogue scale (VAS) for back and leg pain scores prospectively. Failures for this study were those patients who required a subsequent lumbar fusion procedure at the decompressed levels. Statistical analysis was performed using paired t test and Mann–Whitney test.
Results
There were 36 males and 47 females with a mean age of 66 years (range 35–82). The mean follow-up was 36 months (range 19–48 months). The mean pre-operative ODI, EQ-5D, and VAS scores were 52 [standard deviation (SD) 18], 0.25 (SD 0.30), and 61 (SD 22), respectively. All mean scores improved post-operatively to 38 (SD 23), 0.54 (SD 0.34) and 36 (SD 27), respectively. There was a statistically significant improvement in all scores (p ≤ 0.0001). Nine patients (11 %) required a subsequent fusion procedure and five patients (6 %) required revision decompression surgery alone.
Conclusion
Our study’s results show that a lumbar decompression procedure without arthrodesis in a consecutive cohort of patients with lumbar spinal stenosis with degenerative spondylolisthesis had a significant post-operative improvement in ODI, EQ-5D, and VAS. The rate of post-operative instability and subsequent fusion is not high. Only one in 10 patients in this group ended up needing a subsequent fusion at a mean follow-up of 36 months, indicating that fusion is not always necessary in these patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In the case of lumbar spinal stenosis (LSS) with degenerative spondylolisthesis (DS), the Spine Patient Outcomes Research Trial (SPORT) studies support operative over nonsurgical management [1, 2]. However, the literature is not clear as to which surgical technique is the best course of action; in particular, whether an arthrodesis should be added to the procedure. Some state that a fusion should be combined with a lumbar decompression in the setting of a DS [3–5]. Post-operative spinal instability is a major concern surgeons have when performing decompression alone in the presence of DS. Greater intervertebral disc height [6–8], higher body mass index [6], motion at the spondylolisthesis of more than 1.25 mm, and facet angle greater than 50° [7] have been mentioned in the literature as risk factors for the same segment disease (SSD) at the operated level following decompression alone. Others believe that a simultaneous arthrodesis is not required [9–13]; clinical outcomes have not always correlated with radiological findings in these degenerative spine patients [14, 15] and fusing these patients does not seem to improve outcomes [16].
If decompression alone is first done in patients with LSS and DS, how many patients actually end up needing a fusion? Sato et al. [6] have tried to answer this question, but their study suffers from selection and indication bias, besides being a retrospective study. Different decompression techniques may also have different outcomes. The primary aim of our study was to answer this question for our patients, so that we can guide them better in the surgical consent process. We have also evaluated the clinical outcome of this cohort of patients.
Methods
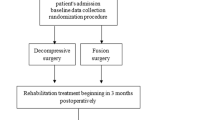
This is a prospective cohort study with single blinding. The study was done at a single UK tertiary referral centre with an aim of evaluating the outcome of decompression alone in patients with LSS due to DS. To avoid recruitment and selection bias, it was decided that surgeons participating in the study would agree to perform a decompression surgery alone, and no fusions, in a consecutive group of patients with LSS due to DS. Those surgeons who did not agree (i.e. wanted to fuse some patients) were excluded, leaving only two senior authors (BSB and DCJ) in the study. Between 2010 and 2013, 83 consecutive patients with LSS and DS, as coming through their outpatient clinics, underwent lumbar decompression surgery without arthrodesis. All patients with LSS but no degenerative olisthesis were excluded. No patients were lost to follow up in this study, and the minimum follow-up was 18 months. The hospital outcome centre team, who had no contact with the surgical or treating team, did the collection of outcome data pre-operatively and post-operatively.
Patients were considered surgical candidates if they had neurogenic claudication or radiculopathy significantly limiting their activities of daily living, and after failure of non-operative measures. Surgery was indicated on the basis of leg pain being worse than back pain; if back pain was the worst problem, no surgery was offered, in line with the policy adopted by all the surgeons in the department. These patients were managed by injections and physiotherapy, and offered surgery only when leg pain overtook the back pain in severity.
The diagnosis of LSS and DS was confirmed on cross-sectional imaging using magnetic resonance imaging (MRI) and standing radiographs. In suspected cases, flexion–extension radiographs were also used to rule out an olisthesis if standing radiographs were normal and MRI images showed significant facet effusions. The measurement of the extent of the olisthesis slip was done on mid-sagittal imaging MRI cuts, or on radiographs, and the size had to be at least 4 mm for the definition of DS to be met. This is similar to parameters used in other reports studying DS patients [9, 13]. The degree of lumbar intervertebral disc degeneration as classified by Pfirrman et al. [17] was done on mid-sagittal MRI slices.
The operative procedure consisted of single or multi-level lumbar decompression using a spinous process osteotomy to gain access. This approach involves dissecting muscles only on one side of the involved spinous processes, keeping the other side intact, and then performing an osteotomy at the base of spinous processes and reflecting the spinous process along with the opposite intact muscle groups to the other side to get a good bilateral view. Subsequently a laminotomy, flavectomy, and partial medial inferior facetectomy were done on both sides to gain access to the central canal, followed by superior facetectomy up to the pedicle, and superior undercutting to clear the lateral recess and foramina. This approach allows a good decompression across both sides without compromising stability. Complete laminectomy was not performed in any patient. The same approach was used regardless of the degree of stability, and a bilateral decompression was done in every case, even if symptoms were unilateral.
Primary outcome measures were the Oswestry Disability Index (ODI), EuroQol Five Dimensions (EQ-5D), and visual analogue scale (VAS) for back and leg pain. These data were obtained from questionnaires completed by patients at baseline, and prospectively collected and analysed at final follow-up by blinded observers. Minimal clinically important difference (MCID) after spine surgery for the ODI [18, 19], EQ-5D [20], and VAS scores [21] was taken as 10, 0.17, and 14 points, respectively.
Clinical assessment was done 3 months post-operatively and then at 18 months, with further follow-up appointments as needed. Patients had to have a minimum follow-up of 18 months to be included in the study. Patients own estimation of walking distance, post-operative medical and surgical complications were recorded. If any patient had persistent pain (back and/or leg), further imaging (radiographs and MRI) was done to record if their DS had worsened. Any patients needing further operations at the affected site, or adjacent levels, and the reasons for the reoperation were recorded.
Failures for this study were those patients who required a subsequent lumbar fusion procedure at the decompressed levels. It was taken that these patients may have benefited from having an arthrodesis at the index procedure.
Statistical analysis was performed using paired t-test (ODI scores) and Mann–Whitney test (EQ-5D and VAS scores) to compare the differences in the mean of the outcome scores from prior to and after surgery. A p value of less than 0.05 was accepted as showing statistical significance. Higher scores in the ODI and VAS, and lower scores in EQ-5D indicate more severe symptoms. Analysis was also carried out on demographical, radiological and clinical factors that may influence subsequent fusion rates. These included age, gender, the grade of olisthesis, the amount of slip, Pfirrman grade, the number of levels decompressed, and the post-operative ODI, EQ-5D, and VAS scores. Again, statistical analysis was performed using paired t-test, Mann–Whitney test, and Chi-squared test, and a p value of less than 0.05 was accepted as showing statistical significance. The estimated walking distance from pre-operative to post-operative was represented by the degree of improvement (better, no change or worse).
Results
The mean follow-up was 36 months (range 19–48 months). The study population comprised of 36 males and 47 females with a mean age of 66 years (range 35–82 years). The majority (86 %) of the spondylolisthesis were Meyerding grade one with the remaining 12 patients being grade two. The mean pre-operative slip was calculated at 5.4 mm (range 4–13 mm). Lumbar intervertebral disc degeneration (Pfirrman grading) was present in the following numbers of patients: I = zero, II = one, III = 17, IV = 29 and V = 36 (mean = 4.2). Seventy-one percent of patients had a one or two level lumbar decompression, and three or more spinal levels were decompressed in 29 % of patients.
The mean pre-operative ODI, EQ-5D, and VAS scores were 52 [standard deviation (SD) 18], 0.25 (SD 0.30), and 61 (SD 22), respectively. All mean scores improved post-operatively to 38 (SD 23), 0.54 (SD 0.34), and 36 (SD 27), respectively. There was a statistically significant improvement in all outcome scores (p ≤ 0.0001). Also, this improvement in mean scores bettered the MCID for the three outcome measures. Patients’ estimated walking distance and improvement in ambulation had become better in 82 % of cases, with only one patient describing worsening of their mobility.
With regard to the primary aim of the study, nine patients (11 %) required a subsequent fusion procedure and five patients (6 %) required revision decompression surgery alone. Indications for fusion were back pain only (five), back and leg pain (two), leg pain only (one), and lumbar vertebral body fracture following a fall (one). Excluding the patient who had revision surgery for a fracture, the total failure rate for patients requiring a fusion in this group was 10 % (eight out of 83).
Of the potential correlating factors, patients who underwent a subsequent fusion procedure had a mean 1.3 (SD 0.5) number of levels decompressed at their initial operation compared with 2.1 (SD 0.9) for those who did not undergo fusion. This was statistically significant with a p value of 0.0139 (see Table 1). Also, the post-operative VAS score was significantly greater for those patients who required a lumbar fusion [mean 55.8 (SD 27.6)] than those who did not [mean 33.1 (SD 26.4)], p = 0.0204 (see Table 2). There was no difference in all the other correlating factors comparing patients that were fused and those that were not.
There were three CSF leaks intra-operatively, which were repaired successfully at the time of surgery. Five patients (6 %) developed post-operative medical complications.
Discussion
Our results show that a lumbar decompression procedure without arthrodesis in a consecutive cohort of patients with LSS and DS had a significant post-operative improvement in ODI, EQ-5D, and VAS. Only one in 10 patients in this group ended up needing an arthrodesis at a mean follow-up of 36 months, indicating that fusion is not always necessary.
There is ample proof in the literature that surgery in patients with LSS is better than non-operative care [22, 23]. The surgeries mentioned in the literature for this condition can broadly be divided into some form of decompression alone, or decompression combined with an arthrodesis. The results of the Swedish Spine Registry by Forsth et al. [9] involving 5390 LSS patients support statistically significant improvement with both these surgical groups, with no difference between the two. Katz et al. [11] had similar results in a prospective multicentre observational study of 272 patients.
Others have tried to address the specific issue of surgery in patients with DS and LSS. Forsth et al. [9] in the same article reporting on 1306 patients with LSS and DS found no differences between decompression alone and decompression with arthrodesis at a final follow-up of 24 months. Sigmundsson et al. [10] used Swespine to report on 1624 patients with L4/5 stenosis and olisthesis and found that adding a fusion did not result in a significant difference in back pain or leg pain at the 2-year follow-up mark. Similar results were found in a smaller study [13]. Other studies [3, 24] have found much better results with an arthrodesis with decompression as compared with decompression alone. These results have been supported by a randomised controlled trial [5]. Turner et al. [16] clearly mention the importance of splitting DS and LSS with LSS alone. Pearson et al. [25] found no differences at baseline between these groups, but better results with surgery in patients with DS.
It is interesting to note that only 21 % of all LSS surgeries mentioned in the Swedish spine registry involve fusions [9], as opposed to 79 % that have decompression alone; in a group of LSS with DS, however, the split is 50–50. Pearson et al. [25] report that 94 % of patients with DS and LSS in their study were fused as opposed to 11 % in LSS group. Surgeons, therefore, differ in their approach to treating with DS with LSS with regards to adding a fusion. Rompe et al. [12] found that the technique of undercutting decompression made a difference to the outcome, and was better than decompression and fusion. There is a lack of clarity about the type of decompression used in some series; laminectomy is mentioned by some [3, 24] but no clear description of its extent. A complete laminectomy is likely to result in instability and this lack of clarity makes it difficult to compare results form different series. Deyo et al. [26] have reported clear problems associated with arthrodesis, both in terms of morbidity and revision surgery; others have reported problems with adjacent segment disease [27–30]. Novel techniques to surgically treat these degenerative spinal conditions have also been tried [31, 32]. Lee et al. [31] found improved clinical outcomes when adding non-fusion dynamic stabilisation to the decompression, and Anekstein et al. [32] showed decompression with total facet joint replacement had clinical success and radiological stability at long-term follow-up.
It is, therefore, critical, in our view, for surgeons to evaluate the results of their own decompression technique in this group of patients (LSS with DS). Our patients routinely ask whether it is necessary to do a more complicated operation instead of a simpler one, keeping in mind the possible complications, longer recovery and risk of further surgery. The results of our study have helped us in counselling our patients better; that only one in 10 patients with this condition will end up needing a fusion at a mean follow-up of 3 years, and the others would be able to avoid a more complicated procedure. Moreover, Mannion et al. [33] have developed criteria for determining the suitability for surgical treatment in DS patients. This may well be the way forward in the future considering the scrutiny that is placed on failed spinal surgery and that patient selection is crucial for its success.
We also found that multilevel decompressions (more than two levels) are unlikely to end up needing an arthrodesis. Smorgick et al. [34] found that fusing more levels in this group of patients is accompanied by more complications. It is highly likely that the process of degeneration is quite advanced in this group of patients, with more loss of disc height at multiple levels resulting in more stiffness. This could also explain why all our patients that ended up getting a fusion had grade 1 olisthesis. The only patient that needed a fusion in grade 2 olisthesis patients was the one who had a fracture from a fall. Pearson et al. [14] reported improved results in conservatively managed DS patients with increased flexibility on pre-operative flexion–extension radiographs compared with those with a smaller amount of mobility. The findings from their cohort study imply that there is no clear relationship between the degree of radiographic instability and patients’ clinical outcomes.
The complication rates in our series are in line with those reported in the literature. The CSF leak rates in these studies are similar to ours of 4 %. Revision decompression was needed on 6 % in our series, not dissimilar to other series [9]. The reasons for fusion were mainly related to worsening of back pain (five out of eight patients); worsening of leg pain resulting in fusion was seen in only three patients. These risks from a decompression alone have to be balanced against the morbidity of longer operating time in this older group of patients with medical comorbidities, which could lead to substantial systemic problems that could even lead to death [26, 35].
There are limitations to our study. First, our sample size is small compared with registry studies and multicentre trials. However, our study has no loss to follow up and does not suffer from any selection or recruitment bias, with data collected by blinded observers. Second, we have not used standing flexion–extension radiographic views for determining instability. We have been thorough in including everyone with an olisthesis, and have carefully studied the longstanding approach in our institution of primarily decompressing these patients, regardless of the presence of instability. A recent study [36] has revealed that the presence of a standing radiograph and supine MRI is enough to diagnose instability; and flexion–extension radiographs offer no added benefit. Other authors have looked at various factors affecting surgical outcome in this group of patients, and flexion–extension instability, greater disc height and facet angle more than 50°, has been reported by Blumenthal et al. [7]. Sato et al. [6] found that the same segment disease-related reoperations were affected by high BMI and disc height, and adjacent segment disease reoperations affected by male gender and facet degeneration. They, however, did not find flexion–extension instability as a significant factor. We have never considered flexion–extension related micro-instability as a significant factor, and thus, it has not been used to differentiate between LSS and DS patients in our series. Last, this is a relatively short-term follow-up study with a mean of three years. Deyo et al. [26] clearly mention that results with time differ in decompression patients as opposed to those who have simple or complex arthrodesis. Most of the reoperations for decompression are performed in the first 2 years, as opposed to the risk of reoperations for simple arthrodesis, which gets worse with time over 4 years. Sato et al. [6] report that reoperation rate for decompression alone is highest in the short- and long-term for SSD, but a closer analysis of their reoperations reveals that the risk is higher in the first 3 years, and the risk for reoperation is no different in the two groups (decompression or decompression and fusion), once the patient survives 3 years (six failed between 3 and 6 years in the fusion group, and seven failed in the decompression alone group). We, therefore, believe that our mean follow-up of 36 months is adequate to comment on the aims of our study.
In conclusion, this prospective cohort single blinded study shows that decompression alone (laminotomy with spinous process osteotomy) for LSS in the setting of DS has good clinical results. The rate of post-operative instability and subsequent fusion is not high with only 10 % of patients needing a subsequent fusion at a mean follow-up of 3 years. We believe, therefore, that fusion is not necessary in every patient undergoing decompression surgery for LSS with DS.
References
Weinstein JN, Lurie JD, Tosteson TD et al (2009) Surgical versus non-operative treatment for lumbar degenerative spondylolisthesis: four-year results of the spine patient outcomes research trial (SPORT) randomized and observational cohorts. J Bone Joint Surg Am 91:1295–1304
Weinstein JN, Lurie JD, Tosteson TD, Hanscom B, Tosteson AN, Blood EA, Birkmeyer NJ, Hilibrand AS, Herkowitz H, Cammisa FP, Albert TJ, Emery SE, Lenke LG, Abdu WA, Longley M, Errico TJ, Hu SS (2007) Surgical versus nonsurgical treatment for lumbar degenerative spondylolisthesis. N Engl J Med 356:2257–2270
Herkowitz HN, Kurz LT (1991) Degenerative lumbar spondylolisthesis with spinal stenosis. A prospective study comparing decompression with decompression and intertransverse process arthrodesis. J Bone Joint Surg Am 73:802–808
Mardjetko SM, Connolly PJ, Shott S (1994) Degenerative lumbar spondylolisthesis: a metaanalysis of literature 1970–1993. Spine (Phila Pa 1976) 19(Suppl):2256–2265
Malmivaara A, Slatis P, Heliovaara M, Sainio P, Kinnunen H, Kankare J, Dalin Hirvonen N, Seitsalo S, Herno A, Kortekangas P, Niinim¨aki T, R¨onty H, Tallroth K, Turunen V, Knekt P, H¨ark¨anen T, Hurri H, Finnish Lumbar Spinal Research Group (2007) Surgical or nonoperative treatment for lumbar spinal stenosis? A randomized controlled trial. Spine 32:1–8 (PubMed: 17202885)
Sato et al (2015) Reoperation rate and risk factors of elective spinal surgery for degenerative spondylolisthesis: minimum 5-year follow-up. Spine J 15:1536–1544
Blumenthal et al (2013) Radiographic predictors of delayed instability following decompression without fusion for degenerative Grade I lumbar spondylolisthesis. J Neurosurg Spine 18:340–346
Lombardi et al (1985) Treatment of degenerative spondylolisthesis. Spine 10:821–827
Försth P, Michaëlsson K, Sandén B (2013) Does fusion improve the outcome after decompressive surgery for lumbar spinal stenosis? A two-year follow-up study involving 5390 patients. Bone Joint J 95-B:960–965
Sigmundsson FG, Jönsson B, Strömqvist B (2015) Outcome of decompression with and without fusion in spinal stenosis with degenerative spondylolisthesis in relation to preoperative pain pattern: a register study of 1,624 patients. Spine J 15(4):638–646. doi:10.1016/j.spinee.2014.11.020
Katz JN, Lipson SJ, Lew RA et al (1997) Lumbar laminectomy alone or with instrumented or noninstrumented arthrodesis in degenerative lumbar spinal stenosis: patient selection, costs, and surgical outcomes. Spine (Phila Pa 1976) 22:1123–1131
Rompe JD, Eysel P, Zöllner J, Nafe B, Heine J (1999) Degenerative lumbar spinal stenosis: long-term results after undercutting decompression compared with decompressive laminectomy alone or with instrumented fusion. Neurosurg Rev 22:102–106
Herron LD, Trippi AC (1989) L4-5 degenerative spondylolisthesis. The results of treatment by decompressive laminectomy without fusion. Spine 14:534–538
Pearson AM, Lurie JD, Blood EA, Frymoyer JW, Braeutigam H, An H, Girardi FP, Weinstein JN (2008) Spine patient outcomes research trial: radiographic predictors of clinical outcomes after operative or nonoperative treatment of degenerative spondylolisthesis. Spine 33:2759–2766
Fox MW, Onofrio BM, Hanssen AD (1996) Clinical outcomes and radiological instability following decompressive lumbar laminectomy for degenerative spinal stenosis: a comparison of patients undergoing concomitant arthrodesis versus decompression alone. J Neurosurg 85:793–802
Turner JA, Ersek M, Herron L, Deyo R (1992) Surgery for lumbar spinal stenosis: attempted meta-analysis of the literature. Spine (Phila Pa 1976) 17:1–8
Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N (2001) Magnetic resonance grade of lumbar intervertebral disc degeneration. Spine 26:1873–1878
Davidson M, Keating JL (2002) A comparison of five low back disability questionnaires: reliability and responsiveness. Phys Ther 82(1):8–24
Davidson M, Keating J (2005) Oswestry disability questionnaire (ODQ). Aust J Physiother 51(4):270
Johnsen LG, Hellum C, Nygaard ØP, Storheim K, Brox JI, Rossvoll I, Leivseth G, Grotle M (2013) Comparison of the SF6D, the EQ5D, and the oswestry disability index in patients with chronic low back pain and degenerative disc disease. BMC Musculoskelet Disord 14(148):1–9
Strömkvist B, Fritzell P, Hägg O, Jönsson B (2009) SWESPINE- the Swedish Spine Register. The 2009 report. http://www.4s.nu/pdf/English_version%20_report2009.pdf Accessed 7 Sep 2015
Weinstein JN, Tosteson TD, Lurie JD et al (2010) Surgical versus nonoperative treatment for lumbar spinal stenosis four-year results of the spine patient outcomes research trial. Spine (Phila Pa 1976) 35:1329–1338
Weinstein JN, Tosteson TD, Lurie JD et al (2008) Surgical versus nonsurgical therapy for lumbar spinal stenosis. N Engl J Med 358:794–810
Bridwell KH, Sedgewick TA, O’Brien MF et al (1993) The role of fusion and instrumentation in the treatment of degenerative spondylolisthesis with spinal stenosis. J Spinal Disord 6:461–472
Pearson A, Blood E, Lurie J et al (2010) Degenerative spond ylolisthesis versus spinal stenosis: does a slip matter? Comparison of baseline characteristics and outcomes (SPORT). Spine (Phila Pa 1976) 35:298–305
Deyo RA, Mirza SK, Martin BI et al (2010) Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA 303:1259–1265
Park P, Garton HJ, Gala VC, Hoff JT, McGillicuddy JE (2004) Adjacent segment disease after lumbar or lumbosacral fusion: review of the literature. Spine (Phila Pa 1976) 29:1938–1944
Chow DH, Luk KD, Evans JH et al (1996) Effects of short anterior lumbar interbody fusion on biomechanics of neighboring unfused segments. Spine 21:549–555
Nagata H, Schendel MJ, Transfeldt EE et al (1993) The effects of immobilization of long segments of the spine on the adjacent and distal facet force and lumbosacral motion. Spine 18:2471–2479
Lehmann TR, Spratt KF, Tozzi JE et al (1987) Long-term follow-up of lower lumbar fusion patients. Spine (Phila Pa 1976) 12:97–104
Lee SE, Jahng TA, Kim HJ (2014) Decompression and nonfusion dynamic stabilization for spinal stenosis with degenerative lumbar scoliosis: Clinical article. J Neurosurg Spine 21(4):585–594 (Epub 2014 Aug 1)
Anekstein Y, Floman Y, Smorgick Y, Rand N, Millgram M, Mirovsky Y (2015) Seven years follow-up for total lumbar facet joint replacement (TOPS) in the management of lumbar spinal stenosis and degenerative spondylolisthesis. Eur Spine J 24(10):2306–2314 (Epub 2015 Mar 8)
Mannion AF, Pittet V, Steiger F, Vader JP, Becker HJ, Porchet F (2014) Development of appropriateness criteria for the surgical treatment of symptomatic lumbar degenerative spondylolisthesis (LDS). Eur Spine J 23(9):1903–1917 (Epub 2014 Apr 24)
Smorgick et al (2013) Single-versus multilevel fusion for single-level degenerative spondylolisthesis and multilevel lumbar stenosis: four-year results of the spine patient outcomes research trial. Spine (Phila Pa 1976) 38:797–805
Jansson KA, Blomqvist P, Granath F, Németh G (2003) Spinal stenosis surgery in Sweden 1987-1999. Eur Spine J 12:535–541
Segebarth PB, Kurd MF, Haug PH, Davis R (2015) Routine upright imaging for evaluating degenerative lumbar stenosis: incidence of degenerative spondylolisthesis missed on supine MRI. J Spinal Disord Tech 28(10):394–397. doi:10.1097/BSD.0000000000000205
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest. No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Additional information
We would be grateful if you could review this revised manuscript, which we have submitted for publication in the European Spine Journal. This work has not been published elsewhere, and all authors believe that it is honest work. We are grateful to the Orthopaedic Institute Ltd, Oswestry for funding.
Rights and permissions
About this article
Cite this article
Ahmad, S., Hamad, A., Bhalla, A. et al. The outcome of decompression alone for lumbar spinal stenosis with degenerative spondylolisthesis. Eur Spine J 26, 414–419 (2017). https://doi.org/10.1007/s00586-016-4637-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-016-4637-7