Abstract
Purpose
Although adolescent idiopathic scoliosis (AIS) is known to impact the 3D orientation of the spine and pelvis, the impact of the vertebral position relative to the X-ray scanner on the agreement between 2D and 3D measurements of a curve has not been evaluated. The purpose of this study was to investigate the agreement between 2D and 3D measurements of the scoliotic curve as a function of the 3D spinal parameters in AIS.
Methods
Three independent observers measured the thoracic and lumbar Cobb angles, Kyphosis, and lordosis on the posterior–anterior and lateral X-rays of AIS patients. The 3D reconstructions were created from bi-planar X-rays and the 3D spinal parameters were calculated in both radio and patient planes using SterEOS software. The degree of agreement between the 2D and 3D measurements was tested and its relationship with the curve axial rotation was determined.
Results
2D and 3D measurements of the sagittal plane spinal parameters were significantly different (p < 0.05). The differences between the 2D and 3D measurements were related to the apical vertebrae rotation, the orientation of the plane of maximum curvature, pelvic axial rotation, and the curve magnitude. Differences between the radio plane and patient plane measurements were related to the pelvic axial rotation, Cobb angles, and apical vertebrae rotation, p < 0.05.
Conclusion
Clinically and statistically significant differences were observed between the 2D and 3D measurements of the scoliotic spine. The differences between the 2D and 3D techniques were significant in sagittal plane and were related to the spinal curve and pelvic rotation in transverse plane.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
Adolescent idiopathic scoliosis (AIS) presents as a complex 3D spinal deformity. Anterior–posterior and lateral X-ray images of the spine have been used for diagnosis and follow-up of this common spinal condition in adolescents. Considering the 3D nature of the spinal deformity in AIS, efforts have been made to develop 3D models of the spine from bi-planar X-ray images using calibration objects [1] or self-calibration techniques [2, 3] to expand our understanding of the true shape of the spinal deformity in AIS. The 3D parameters of the spine have been increasingly used in AIS research to evaluate surgical outcomes [4] and curve progression [5]. 3D parameters combined with mathematical and statistical models [6–8] were used to improve AIS classification and overcome some limitations in the current classification systems. However, some constraints such as time consuming 3D reconstruction process and cost-related considerations limit the application of the 3D measurements in AIS daily clinical care. Additionally, the vast majority of clinical research on AIS treatment decision-making has been based on 2D radiographic measurements [9–11]. The importance of 3D measurement of the spinal curvature and its possible impact on daily clinical care of AIS remains unjustified.
In the past decade a low dose slot scanning machine, EOS (EOS imaging, Paris, France), has been used for AIS diagnostic and follow-up. A dedicated software, SterEOS 2D/3D (EOS imaging, Paris, France) provides a platform for 3D modeling of the spine and pelvis using the 3D position of anatomical landmarks and a statistical model [12, 13]. The accuracy of the 3D reconstruction of the spine has been compared to the 3D reconstructions of the CT scans and no clinically significant difference in terms of bone morphology and clinical measurements were reported [14, 15]. The repeatability and reproducibility of the EOS 3D spinal measurements in moderate spinal curve measurements was shown [12, 13, 16–20]. The maximum differences between the 2D conventional measurements and 3D parameters in surgical cases and post-operative patients were at 7° and 6.9°, respectively [16]. The lordosis 2D and 3D measurements were significantly different for mild to severe cases of AIS, which was related to L5 vertebral wedge [18]. However, the effect of axial rotation of the curve and vertebrae on the agreement between the 2D and 3D clinical measurements of the spine has not been tested.
To identify the impact of spinal axial parameters on the clinical measurements of the spine, we evaluated the agreement between 2D and 3D radiological measurements of the coronal and sagittal spinal parameters and related it to the spinal and pelvic parameters in the transverse plane. We hypothesized that the degree of agreement between the 2D and 3D measurements is associated with the 3D parameters of the spinal curvature.
Methods
Subjects A total number of 36 consecutive AIS patients were retrospectively enrolled. All patients were 10–18 years old with no previous spinal surgery and no other spinal abnormalities including hemivertebrae, spina bifida, supernumerary vertebrae, and spondylolisthesis. Simultaneous posterior–anterior (PA) and lateral X-ray images of the spine and pelvis were registered in EOS (EOS imaging, Paris, France). All patients were positioned posterior-anteriorly with their shoulders and elbows flexed at 45° and knuckles or fingertips touching their ipsilateral clavicles. A total of 29 patients had been scheduled for their spinal fusion within a week from their X-ray exam. The average thoracic and lumbar Cobb angles were 46° (0°–110°) and 30° (0°–90°), respectively.
3D reconstructions and spinal measurements The 3D reconstruction of the spine and pelvis was generated by one trained observer in SterEOS 2D/3D 1.6. This software uses a semi-automated technique that incorporates the user input and a statistical model to generate the 3D model of the spine [12]. To make the patient position with respect to the PA X-ray scanner consistent across the cohort, bi-femoral heads are identified manually and the 3D model was rotated from the original plane, also known as the radio plane (RP), to the patient plane (PP) that passes through the bi-femoral head axis and is perpendicular to the transverse plane (Fig. 1a, b). This alignment is compatible with the coordinate system defined by the Scoliosis Research Society 3D task force (Fig. 1b) [21]. Next, the positions of T1 and L5 superior and inferior endplates were identified, respectively. The software then generates a spline that can be adjusted manually for both the shape of the spinal curve and the width of the vertebrae [12, 13]. A total number of 28 points were digitized on each vertebra to determine the vertebral contour. Additional adjustments can be done manually as needed, to achieve an acceptable contour for each vertebra [12]. Lastly, a 3D model of the spine is generated using a database of vertebral 3D morphology in SterEOS software (EOS imaging, Paris, France). Accuracy of bone morphology was about 1 mm with a maximum error of 4.7 mm [12, 15] and the average angle measurements error was at 4°. In the local vertebral Cartesian coordinate system the Z axis connects the inferior and superior vertebral body centers, the Y axis connects the right and left pedicles, and the X axis was defined as the cross product of the Z- and Y-axes [21] (Fig. 1c). Each vertebra in this model contains 2000 nodes. A least-square regression model was used to define each vertebral superior and inferior endplates using the cloud of points of each vertebra. The clinical measurements of the spine were defined as the angle between the intersection of the superior and inferior vertebral endplates embedding the region of interest by the frontal plane (PP) and sagittal planes (perpendicular to PP) for frontal and sagittal spinal measurements, respectively (Fig. 2). The accuracy of this technique for mild cases of scoliosis and post-operative AIS has been verified [19–21]. The 3D model was used to calculate the thoracic Cobb (TC), lumbar Cobb (LC), T1/T12 Kyphosis (TK) and L1/S1 lordosis (LL) in both PP and RP. Apical vertebrae rotation in the global coordinate system was obtained from the SterEOS software. A code in MATLAB R2014a (The MathWorks Inc., Natick, Massachusetts, United States) was developed to calculate the orientation of the plane of maximum curvature for the thoracic and lumbar curves [8]. In this process a plane was defined using the centroids of the curve end vertebrae and the apex of the curve for thoracic and lumbar curves separately. The angle between this plane and sagittal plane defines the orientation of the plane of maximum curvature of the thoracic and lumbar curves (Fig. 3) [8].
2D spinal measurements Three independent observers measured TC, LC, TK, and LL on the PA and lateral X-rays in iSite® Enterprise (Philips Electronics, 2011, N.V.). To avoid the measurement error due to including different vertebrae in Cobb measurements, curves’ end vertebral levels defined by the SterEOS software were provided to all the three raters. Tangent to the vertebral endplates or the big diameter of the oval resultant from the projection of the vertebral endplate on the X-ray were used to define the vertebral endplate alignment.
Statistical analysis The intraclass reliability was determined for the 2D spinal measurements. The agreement between the 2D and 3D measurements was determined using the Bland–Altman plots. ANOVA test followed by a post hoc Tukey’s HSD was performed to compare 3D RP, 3D PP and 2D measurements of the spinal parameters. A multiple linear regression analysis was used to predict the relationship between the 2D and 3D parameters of spine. Pearson correlation coefficient was used to characterize the relationship between the 2D and 3D techniques differences and spinal and pelvic parameters.
Results
Case presentation
2D radiographical measurements of the TC, LC, TK and LL are shown in Fig. 4a. The frontal view of the spinal 3D reconstruction and the orientation of the thoracic and lumbar end vertebrae, i.e., T6, T11, and L4 are shown in Fig. 4b. The sagittal view of the spine and the 3D orientation of the T1, T12, L1, and L5 are shown in Fig. 4c. The magnitude of the spinal curve measurements using the 2D and 3D techniques were shown on the images.
a 2D radiographical measurements of TC (T6–T11), LC (T11–L4), TK (T1–T12), and LL (L1–L5). b 3D reconstruction of the spine (frontal view) and the 3D orientation of the thoracic and lumbar curves end vertebrae. Cobb angles measurements are shown. c 3D reconstruction of the spine (sagittal view) and the 3D orientation of the T1, T12, and L5 vertebrae. Kyphosis and lordosis measurements are shown
Comparison between the 2D and 3D measurements
A Shapiro–Wilk test showed the data was normally distributed p < 0.05. The average and standard deviation of the 2D and 3D measurements of the TK, LL, TC and LC angles are presented in Table 1. The average of the thoracic and lumbar apical rotation was 12.9° ± 9.8° and 13.3° ± 8.8°, respectively, in PP. The average of the thoracic and lumbar planes of maximum curvature was 47° ± 50.6° and 39.9° ± 54.2°, respectively, in PP. The pelvic rotation calculated by the orientation of the bi-femoral axis in RP was 5.5° ± 3.4°.
The intraclass coefficient of correlation (ICC) was excellent for all the 2D measurements for 95 % confidence interval: TK = 0.90, 0.81 < ICC < 0.95, LL = 0.87, 0.66 < ICC < 0.94, TC = 0.97, 0.95 < ICC < 0.98, LC = 0.97, 0.94 < ICC < 0.98.
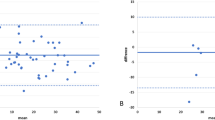
In sagittal plane, a proportional error was observed between the 2D and 3D TK and LL measurements (Fig. 5a, b) while an agreement between the 3D PP and 3D RP measurements for TK and LL measurement was shown (Fig. 5c, d). In terms of LL measurements a large bias (10°) was observed between the 2D and 3D measurements (Fig. 5b). In the frontal plane, 2D and 3D measurement showed agreement for TC and LC measurements (Fig. 6a, b).
a Bland–Altman plots of TK measurements showing an increased bias between the 2D and 3D PP measurements as the average TK increased (Bias = −4.3°, and 95 % limits of agreement 11.3 to −19.1). A negative value shows a higher 3D PP TK value. b Bland–Altman plots of TK measurements showing an agreement between the 3D RP and 3D PP measurements (Bias = 2.9°, and 95 % limits of agreement 11.2 to −5.8). A negative value shows a higher 3D RP TK value. c Bland–Altman plots of LL measurements showing an increased bias between the 2D and 3D PP measurements as the average LL increased (Bias = −11.4°, and 95 % limits of agreement 6.8 to −29.1). A negative value shows a higher 3D PP LL value. d Bland–Altman plots of LL measurements showing an agreement between the 3D RP and 3D PP measurements (Bias = 1.9°, and 95 % limits of agreement 5.9 to −1.9). A negative value shows a higher 3D RP LL value
a Bland–Altman plots of TC measurements showing an agreement between the 2D and 3D PP measurements as the (Bias = −1.2°, and 95 % limits of agreement 1.7 to −4.2). A negative value shows a higher 3D PP TC value. b Bland–Altman plots of LC measurements showing an agreement between the 2D and 3D PP measurements as the (Bias = −1.3°, and 95 % limits of agreement 2.7 to −5.5). A negative value shows a higher 3D PP LC value
ANOVA test showed significant differences between the three measurements, i.e, 2D, 3D RP, and 3D PP. Tukey’s test showed significant differences between 2D and 3D PP measurements for TK p < 0.05 and LL p < 0.01 (Table 1). The coefficient of determination (R 2) of linear regression models between the 2D and 3D PP measurements was at R 2 = 0.57 for LL, R 2 = 0.67 for TK, R 2 = 0.98 for TC, and R 2 = 0.99 for LC, p < 0.05. Including the curve frontal Cobb angle and the pelvic rotation into the multiple linear regression increased the coefficient of determination to R 2 = 0.79 and R 2 = 0.77 for LL and TK, p < 0.05, respectively.
Significant Pearson’s coefficient of correlation between the 2D-3D and PP-RP differences and the spinal and pelvic parameters are listed in Tables 2 and 3, respectively. Significant correlation was found between the 2D-3D differences and pelvic rotation, PMC, apical rotation, and both frontal and sagittal curve magnitudes while the differences between the RP and PP were only related to the pelvic rotation, apical rotation, and frontal Cobb angle (p < 0.05).
Discussion
2D measurement of the spinal deformity is the standard of care for AIS clinical follow-up and surgical planning. New technology using low dose bi-planar stereoradiography in EOS system has made it possible to create 3D models of the spine and visualize the 3D spino-pelvic alignment in standing position. However, as this new technology emerges in clinical care, it is not clear how the 3D measurements of the scoliotic curve relate to 2D clinical X-ray measurements and whether the differences between the 2D and 3D measurements are adversely affected by the axial rotation of the scoliotic curve and curve severity.
Previously, the reproducibility of the spinal angle measurements using the self-calibrated 3D reconstruction of the spine in SterEOS software was tested in pre- and post-operative AIS patients [12, 13, 16–20]. Excellent reliability and reproducibility was reported for 3D measurements in patients with different curve severity except for LL measurements [18]. A high correlation between the 2D and 3D measurements was also reported [18]; however, the agreement between the two measurement techniques and specifics regarding the clinically significant differences between the 2D and 3D parameters as a function of 3D deformities of the spine in transverse plane was not characterized. It has been shown that considering the apical rotation, although measured on the 2D radiographs, will improve the prediction of the Cobb angle from the 2D measurements of the spine which suggest the relationship between the frontal and transverse plane parameters in a scoliotic spine [22]. In line with the current body of literature we found a high correlation between the 2D and 3D parameters; however, further analysis showed significant differences between the 2D and 3D parameters mean values in the sagittal plane. These differences were statistically related to the curve severity in the frontal plane, rotational components of the scoliotic curve, and alignment of the patients with respect to the PA X-ray scanner. Moreover the agreement between the two techniques was affected by the curve severity in the sagittal view.
The differences between the Cobb measurement methods on 2D X-ray images and in SterEOS software® (EOS imaging, Paris, France) can contribute to the 2D and 3D measurement differences. In the 2D X-ray measurements the vertebral endplates or the diameter of the oval shape presenting the endplate is projected on the X-ray projection planes. This technique was shown to be prone to error as the scoliotic curve was rotated with respect to the scanner [23]. In line with these results we showed that the differences between the 2D and 3D techniques increased as the pelvic axial rotation and apical vertebrae rotation increased (Table 2). On the other hand in the SterEOS software a best-fit plane represents the vertebral endplate. Thus the orientation of the lines resultant from the intersection of the best-fit plane representing the vertebral endplates and the projection planes, i.e, RP or PP is dependent to the 3D orientation of the best-fit plane. Different endplate orientation can produce similar projection on the projection plane in the 2D technique; however, the orientation of the intersection of the best-fit plane and projection plane may differ (Fig. 7).The differences can be specially significant in case of an significant off-plane tilt of the vertebral endplate similar to the T11 and T12 orientations in Fig. 4. 3D Vertebral wedging also impacts the orientation of the best-fit plane and the resultant projection on the PP (Fig. 8). Our results showed that the degree of agreement between the 2D and 3D techniques is correlated with the curve severity, which is shown to be related to the vertebral wedging [24]. The 3D orientation of the vertebral endplate and the ability of the software to calculate the best-fit plane are important considerations in patients with significant deformation of the vertebral endplate. Although the accuracy of EOS 3D method has been compared with CT 3D reconstruction [15], this validation was done using a synthetic Sawbone model and severe vertebral wedging and vertebral torsion were not been considered. The effect of vertebral wedging on the degree of agreement between the 2D and 3D measurement were not evaluated in this study and should be the subject of another study.
Schematic of the vertebral endplate projections using the 2D and 3D techniques. The oval’s diameter is projected on the X-ray plane in 2D measurement (black lines). The best-fit plane was intersected by the projection plane in 3D measurements (Bold black lines). While the 2D projections of the 2 ovals’ diameter are parallel (black lines on X-ray projection plane), the best-fit plane intersections results in different alignment (bold black lines on PP)
The linear regression model suggested a significant relationship between the 2D and 3D sagittal plane measurements; however, including the curve severity and the patient alignment with respect to the X-ray scanner in the multiple regression model improved the predictability of the 2D parameters from the corresponding 3D measurements. This suggests that the 3D characteristics of the curve should be integrated into characterization of the relationship between the 2D and 3D parameters especially in the sagittal plane. The latter prohibits us from specifying a cut-off angle where the difference between the 2D and 3D techniques becomes clinically significant only based on the sagittal angle measurement.
Emerging technology available with slot scanning can provide substantially more information about scoliotic deformity than its 2D predecessor. However, current treatment decision-making relies heavily on a body of literature derived from 2D measurements [9–11] and cut-off measurements suggested for classification have not been determined in 3D. Therefore, establishing the ability to “translate” the 3D measurements into 2D is imperative as the first step in integrating the 3D parameters into AIS clinical care.
Conclusion
Differences between the 2D and 3D measurements of the spine were related to the spine and pelvic transverse plane parameters and curve severity. The differences between these measurements need to be acknowledged in clinical consideration of AIS.
References
Dansereau J, Beauchamp A, Guise JD, Labelle H (1990) Three dimensional reconstruction of the spine and the rib cage from stereoradiographic and imaging techniques. 16th Conf Can SocMech Eng 2:61–64
Cheriet F, Meunier J (1999) Self-calibration of a biplane X-ray imaging system for an optimal three dimensional reconstruction. Comput Med Imaging Graph 23(3):133–141
Kadoury S, Cheriet F, Laporte C, Labelle H (2007) A versatile 3D reconstruction system of the spine and pelvis for clinical assessment of spinal deformities. Med Biol Eng Comput 45(6):591–602
Kadoury S, Labelle H, Parent S (2014) 3D spine reconstruction of postoperative patients from multi-level manifold ensembles. Med Image Comput Comput Assist Interv 17(Pt 3):361–368
Nault ML, Mac-Thiong JM, Roy-Beaudry M et al (2014) Three-dimensional spinal morphology can differentiate between progressive and nonprogressive patients with adolescent idiopathic scoliosis at the initial presentation: a prospective study. Spine (Phila Pa 1976) 39(10):E601–E606
Labelle H, Aubin CE, Jackson R, Lenke L, Newton P, Parent S (2011) Seeing the spine in 3D: how will it change what we do? J Pediatr Orthop 31(1 Suppl):S37–S45
Kadoury S, Labelle H (2012) Classification of three-dimensional thoracic deformities in adolescent idiopathic scoliosis from a multivariate analysis. Eur Spine J 21(1):40–49
Sangole AP, Aubin CE, Labelle H et al (2009) Three-dimensional classification of thoracic scoliotic curves. Spine (Phila Pa 1976) 34(1):91–99
Lenke LG, Betz RR, Harms J et al (2001) Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis. J Bone Joint Surg Am 83-A(8):1169–1181
Lark RK, Yaszay B, Bastrom TP, Newton PO, Harms Study G (2013) Adding thoracic fusion levels in Lenke 5 curves: risks and benefits. Spine (Phila Pa 1976) 38(2):195–200
Cho RH, Yaszay B, Bartley CE, Bastrom TP, Newton PO (2012) Which Lenke 1A curves are at the greatest risk for adding-on and why? Spine (Phila Pa 1976) 37(16):1384–1390
Humbert L, De Guise JA, Aubert B, Godbout B, Skalli W (2009) 3D reconstruction of the spine from biplanar X-rays using parametric models based on transversal and longitudinal inferences. Med Eng Phys 31(6):681–687
Gille O, Champain N, Benchikh-El-Fegoun A, Vital JM, Skalli W (2007) Reliability of 3D reconstruction of the spine of mild scoliotic patients. Spine (Phila Pa 1976) 32(5):568–573
Al-Aubaidi Z, Lebel D, Oudjhane K, Zeller R (2013) Three-dimensional imaging of the spine using the EOS system: is it reliable? A comparative study using computed tomography imaging. J Pediatr Orthop B 22(5):409–412
Glaser DA, Doan J, Newton PO (2012) Comparison of 3-dimensional spinal reconstruction accuracy: biplanar radiographs with EOS versus computed tomography. Spine (Phila Pa 1976) 37(16):1391–1397
Ilharreborde B, Steffen JS, Nectoux E et al (2011) Angle measurement reproducibility using EOS three-dimensional reconstructions in adolescent idiopathic scoliosis treated by posterior instrumentation. Spin (Phila Pa 1976)e 36(20):E1306–E1313
Illes T, Tunyogi-Csapo M, Somoskeoy S (2011) Breakthrough in three-dimensional scoliosis diagnosis: significance of horizontal plane view and vertebra vectors. Eur Spine J 20(1):135–143
Somoskeoy S, Tunyogi-Csapo M, Bogyo C, Illes T (2012) Clinical validation of coronal and sagittal spinal curve measurements based on three-dimensional vertebra vector parameters. Spine J 12(10):960–968
Illes T, Somoskeoy S (2013) Comparison of scoliosis measurements based on three-dimensional vertebra vectors and conventional two-dimensional measurements: advantages in evaluation of prognosis and surgical results. Eur Spine J 22(6):1255–1263
Somoskeoy S, Tunyogi-Csapo M, Bogyo C, Illes T (2012) Accuracy and reliability of coronal and sagittal spinal curvature data based on patient-specific three-dimensional models created by the EOS 2D/3D imaging system. Spine J 12(11):1052–1059
Stokes IA (1994) Three-dimensional terminology of spinal deformity. A report presented to the Scoliosis Research Society by the Scoliosis Research Society Working Group on 3-D terminology of spinal deformity. Spine (Phila Pa 1976) 19(2):236–248
Morrison DG, Chan A, Hill D, Parent EC, Lou EH (2015) Correlation between Cobb angle, spinous process angle (SPA) and apical vertebrae rotation (AVR) on posteroanterior radiographs in adolescent idiopathic scoliosis (AIS). Eur Spine J 24(2):306–312
Schmid SL, Buck FM, Boni T, Farshad M (2015) Radiographic measurement error of the scoliotic curve angle depending on positioning of the patient and the side of scoliotic curve. Eur Spine J 25(2):379–384. doi:10.1007/s00586-015-4259-5
Villemure I, Aubin CE, Grimard G, Dansereau J, Labelle H (2001) Progression of vertebral and spinal three-dimensional deformities in adolescent idiopathic scoliosis: a longitudinal study. Spine (Phila Pa 1976) 26(20):2244–2250
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors has any potential conflict of interest.
Rights and permissions
About this article
Cite this article
Pasha, S., Cahill, P.J., Dormans, J.P. et al. Characterizing the differences between the 2D and 3D measurements of spine in adolescent idiopathic scoliosis. Eur Spine J 25, 3137–3145 (2016). https://doi.org/10.1007/s00586-016-4582-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-016-4582-5