Abstract
Purpose
To establish a chordoma tissue cohort (n = 43) and to correlate localization, size, metastasis, residual disease (R-status), recurrences, histological subtype, matrix content, and Ki-67 proliferation index with patients’ overall survival (OS).
Methods and results
We used routine histopathology supplemented by immunohistochemistry. In our patient cohort (median age 69 years, range 17 to 84 years) the median OS was 8.25 years. 24 chordomas were localized in the sacrum, 6 in lumbar vertebrae, 7 in thoracic and cervical vertebrae, 5 were limited to the clivus, and one was localized in the nasal septum. Ten patients had metastases, with pulmonary, nodal, and hepatic involvement. 23 patients had recurrent disease. 23 chordomas were classified as ‘not otherwise specified’ (NOS). Besides NOS, we found the following differentiation patterns: renal cell cancer like in six cases, chondroid in four cases, hepatoid differentiation in three cases, and anaplastic morphology in six cases. Ki-67 index of ≥10 %, presence of metastasis, and the low content of extracellular matrix were statistically linked to poor OS (p < 0.05). The matrix-poor phenotype had a higher Ki-67 index (p < 0.05). Furthermore, presence of metastasis was associated with a higher Ki-67 index in the primary lesion, a positive resection margin, and multiple recurrences (p < 0.05 each).
Conclusion
We propose to include these parameters in the final pathologic report of the resected chordoma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chordomas are rare tumors thought to arise from notochordal remnants along the spine [1]. Although histologically considered as low-grade malignant, chordomas recur frequently with clinical progression very similar to that of overt malignant tumors [2]. Current therapy is surgery followed by radiotherapy [3]. After resection, chordoma recurs in up to 50 % and metastasizes in up to 40 %. Only a minority is completely cured by surgery; the disease-free survival is generally short [4]. There is no efficient standard chemotherapy due to the generally slow growth; however, tyrosine-kinase inhibitors (TKI) [5, 6] and therapeutical targeting of EGFR [7], VEGFR [8], and CDK4/6 [9] have been tried or discussed. The median survival is 6–7 years after diagnosis. Since the disease-free survival after surgery is currently unpredictable, there is a need for new parameters obtained from histological analyses on the resection specimen that allows a risk stratification of chordoma patients and help defining chordoma patients who might benefit from a further adjuvant treatment by chemotherapy or higher doses of conventional radiotherapy [10]. In order to find new histological and immunohistological parameters, we have established a chordoma tissue cohort of 43 patients and have correlated the clinical parameters such as age, localization, size, presence of metastasis, status of residual disease, histological types, matrix content, and proliferation rate with clinical parameters, such as survival and recurrences.
Material and methods
Tumor samples
The study cohort comprises chordoma samples (24 sacrococcygeal/sacral, 13 spinal, 5 clivus, and one extra axial in the nasal septum) from 43 patients (median age at diagnosis, 69 years; 26 male, 17 female; see Fig. 10 for patients’ data) collected during the years 1986 to 2013. Chordomas were pseudonymized to comply with the German law for correct usage of archival tissue for clinical research [11].
Immunomorphology and evaluation of matrix content
Immunochemical staining was performed on formalin-fixed paraffin-embedded tissue sections as described previously [12, 13].
The proportion of stained chordoma cells for each antigen was categorized as no staining “−”; staining in up to 30 % “+”; staining in more than 30 % and up to 70 % “++”, and staining in more than 70 % “+++” of the total number of chordoma cells.
We used the following antibodies: polyclonal antibody against S-100 protein (Dako, Glostrup, Denmark, 1:1000) and monoclonal antibodies against cytokeratin (AE1/AE3, Dako, 1:100), epithelial membrane antigen (EMA; E29, Dako, 1:100), vimentin (3b4, Dako, 1:300), brachyury (H-210, Santa Cruz, Santa Cruz Biotechnology, Heidelberg, Germany 1:100), Ki-67 (clone MIB-1; Dianova, Hamburg, Germany, 1:200). The proliferation index (percentage of Ki-67 positive chordoma cells) was assessed by counting 1000 cells in at least 2 representative areas of the chordomas and the average of both values was used for further analysis as published [14].
For the evaluation of the extracellular matrix content, we used an Azan staining, which is a commonly used routine histological staining consisting of a mixture of Azokarmin G and Anilinblue-Goldorange dyes. This staining marks unselectively collagen fibers in dark-blue.
The Ki-67 index and matrix content (Azan staining) were evaluated on a multihead microscope by two of us (TFB and AvW).
Statistics
GraphPad Prism software (Version 6, La Jolla, USA) and IBM SPSS Statistics (Version 21, Armonk, USA) were used for statistical analysis. All statistical tests are two-sided, and p values lower than 0.05 were regarded as significant.
Results
Chordoma tissue cohort
Our chordoma tissue cohort presently harbors samples of 43 patients (n = 60, including recurrences and metastases) of various localizations. The cohort included 26 male and 17 female patients. The median age of patients at diagnose was 69 years (range 17 to 84 years). The tumor size varied between 0.5 and 50 cm. The distribution of the chordomas along the spine was as follows: clivus (n = 5), cervical and thoracic (n = 7) region, as well as in lumbar (n = 6) and sacral (n = 24) region. One chordoma was localized in the nasal septum. Regarding size, chordomas of the clivus were smaller than all other chordomas studied; the largest chordoma measured 50 cm in diameter and was located in the sacral region (ID: 42, Fig. 1, Supplement Figure 1).
Diagnosis and subtyping was based on the WHO 2013 classification [15]. Twenty-three of 43 chordomas were of the ‘not otherwise specified’ (NOS)-subtype, while two chordomas (one sacral and a cervical chordoma) showed a focal lipoma-like feature, which is claimed to be a putative precursor lesion of a chordoma, i.e., a benign notochordal tumor (Fig. 2f). In 21 chordomas we found focal chondroid (n = 4), renal cell cancer like (n = 6), and hepatoid (n = 3) differentiation (Fig. 2). Six chordomas contained focal anaplasia (Fig. 2e). One chordoma had a chondroid differentiation throughout. The histological subtype was not linked to the topographic distribution along the spine. All chordoma samples consistently expressed brachyury by immunohistochemistry (Fig. 2a). S100-protein and epithelial membrane antigen (EMA) were positive in most samples (Fig. 10).
Histomorphology of chordomas and a benign notochordal tumor (hematoxylin-eosin staining). a Not otherwise specified (NOS) subtype (ID: 17); inset brachyury staining. b Chondroid subtype (ID: 1). c Renal cell cancer-like feature (ID: 28). d Hepatoid feature (ID: 29). e Anaplastic feature (ID: 33). f Benign notochordal tumor (ID: 9); (scale bar 100 µm)
Ten patients had metastasis [lung (n = 5), lymph node (n = 3), and liver (n = 3)] and 21 patients had local recurrences. In our cohort, metastases were restricted to cervical, cervical/thoracic, and sacral chordomas. In 2/43 patients, metastases were present at time of diagnosis (ID 3 and 21). The tumors were resected: complete resection, R0 (n = 7); fragmented tissue, no statements on the resection margin possible, Rx (n = 22); microscopic remnants of chordoma at the resection margin, R1 (n = 12); and macroscopic remnants at the resection margin, R2 (n = 1). The Rx status was more frequent in the clivus and thoracic chordomas compared to the other regions (Supplement Figure 2). Recurrences occurred in cervical, cervical/thoracic, lumbar, and sacral sites (Supplement Figure 3). No metastases and recurrences were detected in thoracic or clivus chordomas. The follow-up data were available from 40 patients; 27 were alive (with a follow-up from 0.5 to 234 months; Fig. 3). Clinical data including surgical strategy and adjuvant radiotherapy are given in Fig. 10.
Correlation of histopathological parameters with clinical data
Of the various parameters evaluated, we found that presence of metastasis has a significant negative impact on OS (p < 0.01; Fig. 4a). A positive R-status was correlated with higher rate of metastases. We found a significant correlation regarding metastasis formation and to the R-status showing that R0 resected chordomas had no metastases at diagnosis or during time course (Fig. 4b). A positive correlation of metastases with the number of recurrences emerged (Fig. 4c). In our cohort age (Supplement Figure 4) and size did not have an impact on OS. To rule out an influence of the topographic localization of the chordomas, we conducted this analysis separately on the mobile spine and non-mobile spine (i.e., clivus chordomas). Metastases were found only in chordomas of the mobile spine. Leaving out the five clivus cases in the above-cited analysis no differences regarding OS and metastasis formation emerged. This means that in our cohort “spine” versus “non-mobile spine” had no influence on these parameters.
a Kaplan–Meier survival estimation according to presence or absence of metastasis. b Bar graph of metastases and R-status. In this correlation, only n = 9 metastases are listed, since one sample with metastasis the R-status is missing. c XY-area graph correlating metastases and recurrences (p < 0.03)
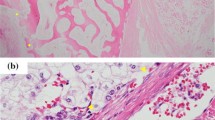
We then focused on the correlation of histological subtypes, the content of extracellular matrix, and the Ki-67 index with OS. In order to establish a cut-off value for Ki-67 we tested values of 1, 1–10, and ≥10 %. The cut-off value of 10 % was chosen since this value showed a clear separation into two groups (see Supplement Figure 5). The histological subtype did not statistically affect the OS (data not shown). We noticed differences in extracellular matrix content in the chordoma samples. For analysis of this parameter the content of extra cellular matrix including stromal cells and connective tissue was estimated in every sample. For this estimation sections of three tissue blocks (if possible) were analyzed in a simple semi quantitative fashion as follows. An extracellular matrix content ≥50 % of tissue volume was categorized as “matrix-rich”; an extracellular matrix content <50 % was defined as “matrix-poor”. Examples of this feature are shown in Fig. 7. These two categories were correlated with the OS; the matrix-poor status turned out to be negatively correlated with OS (p ≤ 0.05; Fig. 8a).
The Ki-67 index ranged from 1 to 50 % with a median of 5 % (Fig. 5). Ki-67 ≥10 % was negatively correlated with OS (p ≤ 0.05; Fig. 6) and, positively, with the matrix-poor phenotype (p ≤ 0.05; Fig. 8b). Furthermore, Ki-67 ≥10 % was correlated with formation of metastases during the observation time (p ≤ 0.05; Fig. 9).
Matrix-rich and matrix-poor chordoma subtype. Hematoxylin-eosin staining (left), Azan staining (right); scale bar 250 µm (left) and 200 µm (right). a Matrix-rich type (ID: 42). b Matrix-poor type (ID: 3), as intrinsic positive control, see in the bottom left corner the positive Azan staining of the tumor capsule
Discussion
Chordomas are slowly proliferating neoplasms, and the overall survival of patients is generally long. In our study, the age and sex distribution as well as median OS being about 8.25 years are in accordance with published data [16]. In our study group, the sacral region was most frequently involved. Size was correlated with site, i.e., the smallest chordomas were localized in the clivus and the largest in the sacrum. Again these data are in line with WHO data [1].
We first analyzed the histology of chordomas and found a wide range of histomorphological features among chordomas and within one tumor. In our cohort, we have chordomas with renal carcinoma like, chondroid, hepatoid differentiation, and anaplastic morphology, which may be misinterpreted as metastasis of carcinomas. Therefore, a brachyury staining is mandatory and defining, if expressed, chordoma as such.
In two cases, we have detected within the chordomas the alleged precursor lesion of chordoma, i.e., a benign notochordal tumor. This finding argues for a possible stepwise evolution of chordoma [17].
For risk estimation of chordoma patients, we have analyzed different histological parameters.
A hitherto not published feature that had a negative influence on OS was the matrix-poor type of a chordoma. Of note, low matrix content is an adverse prognosis pattern in neuroblastomas [18–20]. In line with this observation Naka et al. have found a negative correlation of the content of the intralesional fibrous septa and overall survival in chordomas [21]. In the present study, we extend this concept to a simple estimation of content of extracellular matrix.
The evaluation of the Ki-67 index is a well-known parameter for risk evaluation of chordomas [2, 20–25]. We confirm this concept in our cohort and show that a higher Ki-67 index is correlated with a higher rate of metastasis formation. What is more, we show that the Ki-67 index is higher in matrix-poor chordomas as compared to matrix-rich chordomas. Therefore, we propose to stratify chordomas not only according to histological subtypes but to include description of matrix content in the final report of the histological diagnosis. This histological quantification of matrix content defines the matrix-poor phenotype of chordoma as a more aggressive chordoma, which is associated with a higher Ki-67 index and a shorter OS. This routine stainings done by the pathologist during standard histological work up of the chordoma resection specimen may be of help to recognize patients with a more aggressive type of chordoma; the matrix-poor phenotype may be used as an additional risk factor for the clinical decision after resection of the chordoma, i.e., towards adequate doses of adjuvant radio-/chemotherapy. Furthermore, these new parameters in the final histological report may help estimate more accurately the prognosis of a patient after resection of the chordoma. Nevertheless, these suggested additional new parameters have to be re-evaluated in other cohorts.
Taken together, we have analyzed a representative chordoma cohort and have shown that a positive resection margin, the content of extracellular matrix, and the Ki-67 index have an impact on consecutive metastasis formation and OS. Therefore, we suggest to mention these histological parameters in a final histopathological report on a chordoma. This fast and easy estimation of matrix content may give additive information of prognosis and aggressiveness of the chordoma. However, these new findings have to be approved in an independent cohort.
References
Walcott BP, Nahed BV, Mohyeldin A et al (2012) Chordoma: current concepts, management, and future directions. Lancet Oncol 13:e69–e76. doi:10.1016/S1470-2045(11)70337-0
Bergh P, Kindblom LG, Gunterberg B et al (2000) Prognostic factors in chordoma of the sacrum and mobile spine: a study of 39 patients. Cancer 88:2122–2134
DeLaney TF, Liebsch NJ, Pedlow FX et al (2009) Phase II study of high-dose photon/proton radiotherapy in the management of spine sarcomas. Int J Radiat Oncol Biol Phys 74:732–739
Stacchiotti S, Casali PG, Lo Vullo S et al (2010) Chordoma of the mobile spine and sacrum: a retrospective analysis of a series of patients surgically treated at two referral centers. Ann Surg Oncol 17:211–219. doi:10.1245/s10434-009-0740-x
Casali PG, Messina A, Stacchiotti S et al (2004) Imatinib mesylate in chordoma. Cancer 101:2086–2097
Stacchiotti S, Tamborini E, Lo Vullo S et al (2013) Phase II study on lapatinib in advanced EGFR-positive chordoma. Ann Oncol 24:1931–1936
Hof H, Welzel T, Debus J (2006) Effectiveness of cetuximab/gefitinib in the therapy of a sacral chordoma. Onkologie 29:572–574
Akhavan-Sigari R, Gaab MR, Rohde V et al (2014) Prognostic significance of immunohistochemical expression of VEGFR2 and iNOS in spinal chordoma. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 23:2416–2422. doi:10.1007/s00586-014-3417-5
Von Witzleben A, Goerttler LT, Marienfeld R et al (2015) Preclinical characterization of novel chordoma cell systems and their targeting by pharmocological inhibitors of the CDK4/6 cell cycle pathway. Cancer Res. doi:10.1158/0008-5472.CAN-14-3270
Noel G, Habrand JL, Mammar H et al (2001) Combination of photon and proton radiation therapy for chordomas and chondrosarcomas of the skull base: the Centre de Protontherapie D’Orsay experience. Int J Radiat Oncol Biol Phys 51:392–398
Ärztebl D (2003) 100(A):2251 (Heft 34–35 )
Barth TFE, Martin-Subero JI, Joos S et al (2003) Gains of 2p involving the REL locus correlate with nuclear c-Rel protein accumulation in neoplastic cells of classical Hodgkin lymphoma. Blood 101:3681–3686
Weniger MA, Pulford K, Gesk S et al (2006) Gains of the proto-oncogene BCL11A and nuclear accumulation of BCL11A(XL) protein are frequent in primary mediastinal B-cell lymphoma. Leukemia 20:1880–1882
Determann O, Hoster E, Ott G et al (2008) Ki-67 predicts outcome in advanced-stage mantle cell lymphoma patients treated with anti-CD20 immunochemotherapy: results from randomized trials of the European MCL network and the german low grade lymphoma study group. Blood 111:2385–2387. doi:10.1182/blood-2007-10-117010
Flanagan AMYT (2013) Chordoma. In: Fletcher CDM, Bridge JA, Hogendoorn PCW, Mertens F (eds) World Health Organization classification of tumours. Pathology and genetics of tumours of soft tissue and bone. IARC Press, Lyon, pp 328–329
McMaster ML, Goldstein AM, Bromley CM et al (2001) Chordoma: incidence and survival patterns in the United States, 1973–1995. Cancer Causes Control CCC 12:1–11
Shen J, Li C-D, Yang H-L et al (2011) Classic chordoma coexisting with benign notochordal cell rest demonstrating different immunohistological expression patterns of brachyury and galectin-3. J Clin Neurosci Off J Neurosurg Soc Australas 18:96–99. doi:10.1016/j.jocn.2010.03.066
Ambros IM, Zellner A, Roald B et al (1996) Role of ploidy, chromosome 1p, and Schwann cells in the maturation of neuroblastoma. N Engl J Med 334:1505–1511. doi:10.1056/NEJM199606063342304
Joshi VV (2000) Peripheral neuroblastic tumors: pathologic classification based on recommendations of international neuroblastoma pathology committee (Modification of shimada classification). Pediatr Dev Pathol Off J Soc Pediatr Pathol Paediatr Pathol Soc 3:184–199
Shimada H, Ambros IM, Dehner LP et al (1999) The International Neuroblastoma Pathology Classification (the Shimada system). Cancer 86:364–372
Naka T, Boltze C, Kuester D et al (2005) Intralesional fibrous septum in chordoma: a clinicopathologic and immunohistochemical study of 122 lesions. Am J Clin Pathol 124:288–294
Saad AG, Collins MH (2005) Prognostic value of MIB-1, E-cadherin, and CD44 in pediatric chordomas. Pediatr Dev Pathol Off J Soc Pediatr Pathol Paediatr Pathol Soc 8:362–368
Yakkioui Y, Temel Y, Creytens D et al (2014) A comparison of cell-cycle markers in skull base and sacral chordomas. World Neurosurg 82:e311–e318
Sakai K, Hongo K, Tanaka Y, Nakayama J (2007) Analysis of immunohistochemical expression of p53 and the proliferation marker Ki-67 antigen in skull base chordomas: relationships between their expression and prognosis. Brain Tumor Pathol 24:57–62
Horbinski C, Oakley GJ, Cieply K et al (2010) The prognostic value of Ki-67, p53, epidermal growth factor receptor, 1p36, 9p21, 10q23, and 17p13 in skull base chordomas. Arch Pathol Lab Med 134:1170–1176
Acknowledgments
The technical help Iwona Nerbas, Julia Melzner, Lena Kelsch, and Michaela Buck is greatly acknowledged.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There is no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
586_2015_4242_MOESM1_ESM.pdf
Supplement Figures: 1. Bar graph regarding localization and size of chordoma. 2. Bar graph of topographic localization and R-status. 3. Bar graph of recurrences and topographic localization of chordomas. 4. Kaplan–Meier survival estimation according to age. 5. Kaplan–Meier survival estimation according to Ki-67 1 %, >1–10 % and ≥10 %. (pdf 594 kb)
Rights and permissions
About this article
Cite this article
von Witzleben, A., Goerttler, L.T., Lennerz, J. et al. In chordoma, metastasis, recurrences, Ki-67 index, and a matrix-poor phenotype are associated with patients’ shorter overall survival. Eur Spine J 25, 4016–4024 (2016). https://doi.org/10.1007/s00586-015-4242-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-015-4242-1