Abstract
Purpose
To investigate the regional tensile properties of human annulus fibrosus (AF) and relate them to magnetic resonance imaging (MRI) findings.
Methods
44 human cadaveric lumbar spines were harvested (24 male, 20 female, aged 25–64 years). MRI was used to identify Pfirrmann grade of disc degeneration, and Modic changes (MCs). Intervertebral discs were then removed and dissected into five regions: nucleus pulposus, anterior AF, anterolateral AF, lateral AF, and posterolateral AF. Samples for tensile testing (1.5 mm × 1.5 mm × 5 mm) were removed from inner, middle and outer parts of each region.
Results
1969 specimens from 189 discs were stretched to failure. Average tensile stiffness (modulus) increased from 4.80 MPa in the inner AF to 13.0 MPa in the outer AF. Strength (UTS) increased similarly, from 1.18 to 3.29 MPa, whereas elongation at failure decreased, from 49 to 38 %. The only significant change with age was a reduction in UTS in the middle annulus. In contrast, severe grades of disc degeneration were associated with consistent and highly significant reductions in tensile properties. Effects were greatest in the outer AF, where stiffness and strength fell by 29 and 43 %, respectively. Modic changes also were associated with reduced stiffness and strength, but here the effects were greatest in the inner and middle AF.
Conclusion
Weakening of degenerated AF may be caused by accumulating structural defects, and enzymatic degradation. MRI has the potential to identify local weakening of the AF.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The tensile mechanical properties of the annulus fibrosus (AF) are clinically important, because tensile failure of the AF can allow disc herniation to occur, and probably is an irreversible step in the disc degeneration process [1]. However, less is known about the mechanical properties of the AF than, for example, the properties of the adjacent vertebral bodies. One of the underlying problems is that the AF is a complex inhomogeneous and anisotropic laminated structure, and its properties vary with location and direction, so it is difficult to reconcile information from different studies.
The AF comprises 15–25 concentric lamellae of collagen fibers embedded in a proteoglycan matrix. Annulus fibers are oriented at 45°–65° to the spinal axis, with fibre direction alternating between consecutive lamellae (Fig. 1). The AF acts in tension to restrain the increasing fluid pressure in the nucleus when the spine is compressed, and it is sufficiently rigid to stabilise the spine by resisting bending, torsion and shear. Typically the AF fails in tension, when combined loading in compression and bending forces pressurised nucleus tissue through a fissure growing radially outwards in the AF, usually posterior to the nucleus [1]. Such a disc herniation can cause back pain and sciatica.
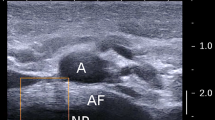
Cadaveric discs were divided into the following regions for testing: nucleus pulposus (NP), anterior annulus (A), anterolateral annulus (AL), lateral annulus (L) and posterolateral annulus (PL). The posterior annulus (P) was generally too thin and disrupted for testing. The inset image shows that small specimens were prepared approximately parallel to one of the annulus fiber directions (indicated by the blue line). Note that the curvature of annulus lamellae in an intact disc is reduced when the disc is first divided into regions, and nucleus pressure is lost. This altered geometry reduces collagen fibre disruption in the small excised specimens
Previous tensile tests of AF have shown that, even though values of ultimate tensile stress (UTS) are normalised for specimen size, UTS nevertheless increases with specimen size, presumably because small excised tissue samples involve greater disruption of the collagen network [2]. Despite this complication, there is consistent evidence that annulus UTS and modulus (normalised stiffness) increase radially outwards, from the inner AF to the disc periphery [3–6]. This can be attributed to the increasing volume fraction of large and strong collagen Type I fibres in the periphery [7]. Tensile properties also increase in a direction parallel to the collagen fibres [8], and are much reduced when lamellae are pulled apart in the radial direction [9, 10] because such delamination is resisted only by a small population of translamellar bridging elements [11].
Radiological features of disc degeneration have been extensively studied, but there is limited understanding of how these features relate to the tensile properties of the AF. There is even less certainty concerning the interacting influences of age and degeneration on AF integrity. Increasing age-related collagen cross-linking [12] makes cartilage stiffer and stronger [13], but degeneration-related collagen denaturation [14] and macroscopic disruptions in lamellar structure [15] would weaken it.
The purpose of the present experiment is to determine how the competing effects of age and degeneration (as imaged by MRI) affect the regional tensile properties of the human AF. Because of the complications mentioned above, it was necessary to test a large number of specimens and to allow for known regional variations in mechanical properties. We hypothesise that degenerative changes evident on MRI (Pfirrmann grade, and the presence of Modic changes) are associated with specific changes in regional tensile properties of the AF. By comparing AF properties with MRI scans of the whole lumbar (cadaver) spine, the study aimed to make it possible, for the first time, to estimate AF integrity in an individual patient.
Materials and methods
Cadaveric material
Lumbar spines (T12–S1) were excised within 24 h of death from 44 cadavers (24 male, 20 female, mean age 46 years, range 25–64). Consent was managed by body donation agreement. Cause of death was either stroke or heart attack, and none of the subjects had a history of back surgery, infection or malignant diseases, or prolonged bed rest before death. Following X-ray and MRI, all intervertebral discs were excised, wrapped in cling film to minimize water loss, and stored at −20 °C.
Preparation of specimens
Each disc was divided with a scalpel into nucleus pulposus (NP), anterior AF, anterolateral AF, lateral AF and posterolateral AF. Each region was further divided into inner, middle and outer parts (Fig. 1). The posterolateral AF was only divided into inner and outer sub-regions because the radius here is relatively small. AF from the posterior midline was excluded because many samples were small, disrupted and dehydrated. The innermost AF was defined by the presence of the first discernible lamellae, and the outer-most AF was defined by the presence of only longitudinal fibers from the longitudinal ligaments. A cutting device with parallel razor blades was used to obtain 1.5 mm-thick slices of AF, from which specimens were cut parallel to one of the fiber directions (Fig. 1). Tissue was partially frozen so the geometry remained regular. Specimens were wrapped in cling film to minimize water loss. Then, cyanoacrylate adhesive was used to fix both ends of each slice to strips of sandpaper with the rough surface outside (Fig. 2) so it could be gripped securely. The width, thickness and length (between sandpaper edges) were designed to be 1.5 mm × 1.5 mm × 5 mm, and the exact dimensions of each specimen were measured after cutting and adhesion using a Vernier caliper (accuracy 0.1 mm). A digital display minimized specimen deformation during measurement. To reduce errors, all dimensions were measured twice (by two investigators) and then averaged.
a Annulus specimen with folded strips of sandpaper glued to both ends. Typical dimensions of specimen (between edges of sandpaper) were 1.5 mm × 1.5 mm × 5 mm. b Annulus specimen after testing showing irreversible (residual) extension, and focal disruption (on the left). Black ink marks were used to reveal any slipping between specimen and sandpaper
Tensile testing
Specimens were secured in the clamps of the computer-controlled test machine with the accuracy of 0.01 mm and 0.001N (Z2.5, Zwick/Roell, Germany). A pre-tension of 0.01N was applied by the test machine to define zero elongation and to keep the specimens equally straight before testing. To minimise dehydration, testing was completed within 3 min, and a vaporizer (using physiologic saline) was used to increase humidity around the specimen. Each specimen was preconditioned by being stretched 4 times to ~20 % strain, and then stretched to failure at 1 mm/s. A digital video camera (AF-S Micro Nikkor 105 mm, D5100, Nikon, Japan) recorded tissue deformation at 25 Hz. Images were used to check the mode of tissue failure, to detect any slipping in sandpaper or clamps, and to record specimen dimensions during testing. Tension was recorded by a load cell, and specimen elongation was calculated from the separation of the clamps. Force–deformation data were converted to stress-strain data automatically using TestXpert II (V1.42, Zwick/Roell, Germany). A typical stress-strain graph (Fig. 3) comprises a ‘toe’ region, a linear region, and an abrupt turning point, which marks the ultimate tensile strength (UTS). Tensile modulus (stiffness) was calculated as the gradient of the linear region. Strain (elongation) was expressed as a percentage of initial length. Calculations were processed using Matlab (MathWorks, Natick, MA).
Typical stress-strain curve obtained when an annulus specimen (Fig. 2) was stretched to failure. Gradient of the linear region indicates the specimen’s tensile modulus (normalised stiffness), and the peak of the graph indicates specimen’s ultimate tensile strength (UTS)
MRI scans
Scanning was performed with a GE Sigma CV/I (1.5T) using a surface coil. Sagittal T1-weighted images were obtained using repetition/echo times of 420/13 ms and a bandwidth of 140 Hz/Px, while T2-weighted images used 2300/105 ms and 160 Hz/Px. For both T1 and T2, the matrix size was 320 × 224 and field of view was 28 × 28 mm. Slice thickness was 4 mm for both sagittal and transverse slices, while the inter-slice gap was 1 mm. For each imaged lumbar spine, there were 9 sagittal slices of T1- and T2-weighted images.
For evaluating disc degeneration and MCs, MR images were independently viewed by an experienced radiologist and an orthopedic surgeon, who were blinded to patient information. A consensus was reached if there was initial disagreement. Disc degeneration was graded initially from 1–5, according to Pfirrmann [16], and further classified as ‘normal’ (grade 1 and 2), ‘mild degeneration’ (grade 3) and ‘severe degeneration’ (grade 4 and 5). MCs were evaluated with the criteria reported by Modic et al. [17].
Statistical analysis
Data were processed in Excel and transferred to SPSS 16.0 (SPSS Inc, Chicago, Ill). Specimens which slipped in the clamps during testing were excluded, and an additional test was performed on adjacent tissue. Spearman rank correlation was used to quantify relationships between (a) average values of stiffness or strength and (b) ordinal variables such as radial location (inner, middle, outer), age range (20–29 years etc.), spinal level, and disc region (anterior to posterolateral). Group t tests were used to compare mean properties of male and female specimens, or those with and without MCs. Analysis of variance (ANOVA) was used to compare tensile properties between different grades of disc degeneration, with differences between each grade being analyzed with least significant difference (LSD). p < 0.05 was defined as significantly different.
Results
Four discs were excluded because they were highly dehydrated during frozen storage. A total of 1969 specimens were tested, from 189 discs from 44 cadavers (Table 1). Most failed in the central region between sandpaper grips (Fig. 2). Average dimensions and tensile properties of all AF specimens are summarised in Table 2. Modulus (stiffness) increased steadily from 4.80 MPa in the inner AF to 13.0 MPa in the outer AF. Similarly, UTS (strength) increased from 1.18 to 3.29 MPa, whereas maximum elongation decreased, from 49 to 38 %. These effects are all significant (p < 0.05).
Sub-group analyses (Table 3) showed that gender had little effect on tensile properties (Tables 3, 5) so male and female data were pooled. Data for each spinal level were so similar that average values are not shown in Table 3. Spearman rank correlation confirmed that spinal level had no significant effect on tensile properties (Table 4), so data were pooled for all levels. A comparison of disc regions showed that strength and stiffness decreased from anterior to posterolateral, although the effects were small (Table 3), and significant only in the outer annulus (Table 4). Age-related changes were small, and apparent differences in younger and older specimens (Fig. 4) may be attributable to small specimen numbers. The only significant age-related change was a fall in UTS in the middle annulus (Table 4).
Bar chart showing how age (in decades) influenced stiffness (modulus) and strength (UTS) in the outer (a), middle (b), and inner (c) annulus. Complementary data from Skrzypiec et al. [6] are shown on the right side of the dotted line. Error bars indicate the SEM
Disc degeneration and Modic changes (MCs) were most common in L4-L5 and L5-S1 discs (Table 1). 10 discs were adjacent to MCs (1 of Type I and 9 of Type II). Modic Type I and II changes probably represent successive phases of a continuous process [18], and differences between them can be affected by MRI field strength [19], so both Types were pooled. MCs and degeneration co-existed in 3 discs, one at L4/L5 and two at L5/S1, and all three had mild degeneration. Increasing grade of disc degeneration was consistently associated with reduced modulus and UTS (Table 3), with the greatest changes seen in severe degeneration (Pfirrmann grades 4 and 5). The outer AF was most affected, with modulus and UTS falling by 29 and 43 % (respectively), in ‘severely’ degenerated discs compared to ‘normal’. Changes in the middle and outer AF were significant (Table 5). Modic changes also were associated with reduced tensile properties, but here the effects were greatest in the inner and middle AF. In the middle AF, modulus and UTS fell by 28 and 38 % (respectively), in discs adjacent to MCs, and in the inner AF, the falls were 20 and 29 %. These changes, depicted in Fig. 5, were all highly significant (Table 5).
Bar chart showing how MRI evidence of disc degeneration influenced annulus tensile properties. a stiffness (modulus) and grade of disc degeneration, b strength (UTS) and grade of disc degeneration, c stiffness (modulus) and modic changes, d strength (UTS) and Modic changes. Significant differences are indicated *(p < 0.05) or **(p < 0.01)
Discussion
Summary of findings
Stiffness and strength increased markedly from the inner to outer AF, whereas maximum elongation decreased. These properties varied little with gender, spinal level or age, but were greatly reduced in severely degenerated discs. Changes associated with Pfirrmann grade of disc degeneration affected primarily the middle and outer AF, whereas those associated with Modic changes affected only the inner and middle AF.
Association with previous studies
Tensile strength of small samples of AF has been reported to vary from 0.6 MPa [3] to 49 MPa [20], depending on sample location, size and orientation, as well as on age and degeneration. Values in the present study range from 0.84 to 3.50 MPa, which is consistent if the smaller specimen size is taken into account. The increase in modulus and UTS from inner to outer AF is also consistent with previous studies [3, 20–22]. Impaired tensile properties in old and degenerated discs have been reported previously [10, 22] but the present study is able to show that degeneration has a greater effect than age. This agrees with Acaroglu et al. [22] who found that age is not significantly correlated with the tensile properties of the AF, and with Skrzypiec et al. [6] who reported age-related weakening of the AF only in the outer AF in males. Some results from this latter study have been combined with our own results in Fig. 4 to suggest that aging probably has a weakening effect on tensile properties after the 6th decade in life (Fig. 3). Our finding that tensile properties decrease from anterior to posterolateral regions (Table 3) agrees with Little et al. [9] who reported that the posterior AF has the highest matrix tensile strength by clinical analysis, and with studies that show degenerative changes are most severe in the posterolateral AF [1]. However, it is not compatible with Lewis et al. [3], who found the lateral AF to have the highest tensile modulus (measured by atomic force microscopy).
Explanation of results
Stiffness and strength increase from inner to outer AF because of increasing density of Type I collagen in the disc periphery [7]. Values are similar for males and females, and for all spinal levels, because modulus and UTS are normalised for specimen size, and so do not reflect increased body size in men, or increased spinal loading at L5-S1. Age probably has little overall effect because of two opposing factors. Firstly, collagen concentration increases with age [7], and individual collagen fibres are strengthened by age-related increases in molecular cross-linking [12]. Secondly, however, these biochemical strengthening effects are opposed by small structural defects in the AF which accumulate with age [15]. This second effect may dominate the first in very old specimens, but the maximum age of specimens in the present study was only 64 years. AF tensile properties decrease in severe disc degeneration because this pathological condition is strongly associated with increasing structural defects in the AF [1, 15] which disturb force transduction and generate stress gradients within the AF [24]. Degeneration is also associated with increased activity of matrix-degrading enzymes [14], which weaken the matrix directly, and reduce collagen cross-linking by increasing collagen turnover [23]. Grade of degeneration may have most effect on the outer AF (Table 3) because this region is more easily disrupted by excessive forwards bending and torsion [1]. Interestingly, modulus and UTS sometimes increased slightly with mild disc degeneration (Table 3) although this was not significant. This could be because reduced hydration in mild degeneration stiffens the AF. Modic changes (MCs) are associated with endplate damage which in turn is linked to decompression of the disc nucleus and increased load-bearing by the middle and inner AF [25]. This could explain why these regions of AF are weakened in discs adjacent to MCs.
Strengths and weaknesses
This is the first study to compare MRI evidence of disc degeneration with tensile properties of the AF. The large number of discs tested, and the restricted age-range (25–64 years) made it possible to distinguish between the effects of ageing and degeneration, and the large number of samples from each disc ensured that results would not be confounded by regional variations in tensile properties. Specimen orientation (parallel to the predominant fiber direction) and size were chosen to enable good spatial resolution of materials properties, but without the excessive degradation of properties which occurs when very small samples are used [2]. A shortcoming of our research is that the number of discs is relatively small compared to clinical studies. Another is that the discs were tested following death and frozen storage. However, these processes have little effect on the mechanical properties of the annulus [1], and frozen specimens are required to obtain precise dimensions. Some specimen dehydration may have occurred during testing, but this was less than 10 % in similar experiments, and considered unlikely to have much effect on tensile properties [6].
Conclusion
Increasing age does not greatly reduce the tensile properties of the AF because the weakening effect of propagating annulus defects is opposed by strengthening effects arising from increased collagen content and cross-linking. With increasing disc degeneration, however, the former effect dominates the latter, and is assisted by enzymatic matrix breakdown, so the AF becomes softer and weaker. Effects are greatest in the outer AF because it is more easily disrupted by excessive forwards bending and torsion. In contrast, Modic changes (MCs) are associated with endplate damage and nucleus decompression, which lead to increased load-bearing by the middle and inner AF, and hence to reduced tensile properties in these regions. Clinical MRI scans can reveal the presence of severe disc degeneration, and also MCs, so they have the potential to predict reduced tensile properties in all regions of the AF.
References
Adams MA, Bogduk N, Burton K, Dolan P (2013) The Biomechanics of Back Pain, 3rd edn. Churchill Livingstone, Edinburgh
Adams MA, Green TP (1993) Tensile properties of the annulus fibrosus. I. The contribution of fibre-matrix interactions to tensile stiffness and strength. Eur Spine J 2(4):203–208
Lewis NT, Hussain MA, Mao JJ (2008) Investigation of nano-mechanical properties of annulus fibrosus using atomic force microscopy. Micron 39(7):1008–1019. doi:10.1016/j.micron.2007.08.009
Skaggs DL, Weidenbaum M, Iatridis JC, Ratcliffe A, Mow VC (1994) Regional variation in tensile properties and biochemical composition of the human lumbar anulus fibrosus. Spine (Phila Pa 1976) 19(12):1310–1319
Umehara S, Tadano S, Abumi K, Katagiri K, Kaneda K, Ukai T (1996) Effects of degeneration on the elastic modulus distribution in the lumbar intervertebral disc. Spine (Phila Pa 1976) 21(7):811–819
Skrzypiec D, Tarala M, Pollintine P, Dolan P, Adams M (2007) When are intervertebral discs stronger than their adjacent vertebrae? Spine (Phila Pa 1976) 32(22):2455–2461
Eyre DR, Muir H (1977) Quantitative analysis of types I and II collagens in human intervertebral discs at various ages. Biochim Biophys Acta 492(1):29–42
Jacobs NT, Smith LJ, Han WM, Morelli J, Yoder JH, Elliott DM (2011) Effect of orientation and targeted extracellular matrix degradation on the shear mechanical properties of the annulus fibrosus. J Mech Behav Biomed Mater 4(8):1611–1619. doi:10.1016/j.jmbbm.2011.03.016
Little JP, Pearcy MJ, Tevelen G, Evans JH, Pettet G, Adam CJ (2010) The mechanical response of the ovine lumbar anulus fibrosus to uniaxial, biaxial and shear loads. J Mech Behav Biomed Mater 3(2):146–157. doi:10.1016/j.jmbbm.2009.09.002
Fujita Y, Duncan NA, Lotz JC (1997) Radial tensile properties of the lumbar annulus fibrosus are site and degeneration dependent. J Orthop Res 15(6):814–819. doi:10.1002/jor.1100150605
Schollum ML, Robertson PA, Broom ND (2009) A microstructural investigation of intervertebral disc lamellar connectivity: detailed analysis of the translamellar bridges. J Anat 214(6):805–816. doi:10.1111/j.1469-7580.2009.01076.x
DeGroot J, Verzijl N, Wenting-van Wijk MJ, Jacobs KM, Van El B, Van Roermund PM, Bank RA, Bijlsma JW, TeKoppele JM, Lafeber FP (2004) Accumulation of advanced glycation end products as a molecular mechanism for aging as a risk factor in osteoarthritis. Arthritis Rheum 50(4):1207–1215. doi:10.1002/art.20170
Kawchuk G, Kaigle Holm A, Ekström L, Hansson T, Holm S (2009) Bulging of the inner and outer annulus during in vivo axial loading of normal and degenerated discs. J Spinal Disord Tech 22(3):214–218
Antoniou J, Steffen T, Nelson F, Winterbottom N, Hollander AP, Poole RA, Aebi M, Alini M (1996) The human lumbar intervertebral disc: evidence for changes in the biosynthesis and denaturation of the extracellular matrix with growth, maturation, ageing, and degeneration. J Clin Invest 98(4):996–1003. doi:10.1172/jci118884
Haefeli M, Kalberer F, Saegesser D, Nerlich AG, Boos N, Paesold G (2006) The course of macroscopic degeneration in the human lumbar intervertebral disc. Spine (Phila Pa 1976) 31(14):1522–1531. doi:10.1097/01.brs.0000222032.52336.8e
Pfirrmann C, Metzdorf A, Zanetti M, Hodler J, Boos N (2001) Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine (Phila Pa 1976) 26(17):1873–1878
Modic MT, Steinberg PM, Ross JS, Masaryk TJ, Carter JR (1988) Degenerative disk disease: assessment of changes in vertebral body marrow with MR imaging. Radiology 166(1 PT 1):193–199
Zhang YH, Zhao CQ, Jiang LS, Chen XD, Dai LY (2008) Modic changes: a systematic review of the literature. Eur Spine J 17(10):1289–1299. doi:10.1007/s00586-008-0758-y
Bendix T, Sorensen JS, Henriksson GA, Bolstad JE, Narvestad EK, Jensen TS (2012) Lumbar modic changes-a comparison between findings at low- and high-field magnetic resonance imaging. Spine (Phila Pa 1976) 37(20):1756–1762. doi:10.1097/BRS.0b013e318257ffce
Ebara S, Iatridis J, Setton L, Foster R, Mow V, Weidenbaum M (1996) Tensile properties of nondegenerate human lumbar anulus fibrosus. Spine (Phila Pa 1976) 21(4):452–461
Elliott DM, Setton LA (2001) Anisotropic and inhomogeneous tensile behavior of the human anulus fibrosus: experimental measurement and material model predictions. J Biomech Eng 123(3):256–263
Acaroglu ER, Iatridis JC, Setton LA, Foster RJ, Mow VC, Weidenbaum M (1995) Degeneration and aging affect the tensile behavior of human lumbar anulus fibrosus. Spine (Phila Pa 1976) 20(24):2690–2701
Sivan SS, Wachtel E, Tsitron E, Sakkee N, van der Ham F, Degroot J, Roberts S, Maroudas A (2008) Collagen turnover in normal and degenerate human intervertebral discs as determined by the racemization of aspartic acid. J Biol Chem 283(14):8796–8801. doi:10.1074/jbc.M709885200
Stefanakis M, Luo J, Pollintine P, Dolan P, Adams MA (2014) ISSLS Prize winner: Mechanical influences in progressive intervertebral disc degeneration. Spine (Phila Pa 1976) 39(17):1365–1372. doi:10.1097/brs.0000000000000389
Dolan P, Luo J, Pollintine P, Landham PR, Stefanakis M, Adams MA (2013) Intervertebral disc decompression following endplate damage: implications for disc degeneration depend on spinal level and age. Spine (Phila Pa 1976) 38(17):1473–1481. doi:10.1097/BRS.0b013e318290f3cc
Acknowledgments
National Natural Science Foundation of China (No. 31270997 and No.81171739) grant funds were received to support this work. The authors wish to express their gratitude to Professor Michael Adams and Dr. Trish Dolan for sharing their data and providing assistance with the article.
Conflict of interest
Authors have no potential conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shan, Z., Li, S., Liu, J. et al. Correlation between biomechanical properties of the annulus fibrosus and magnetic resonance imaging (MRI) findings. Eur Spine J 24, 1909–1916 (2015). https://doi.org/10.1007/s00586-015-4061-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-015-4061-4