Abstract
Purpose
Lateral transpsoas lumbar interbody fusion (LTIF) is an accepted treatment for degenerative lumbar disc disease. Bilateral percutaneous transfacet (TF) fixation is a promising option for stabilization following LTIF. Here, we describe our experience with this technique and assess the clinical outcomes and efficacy.
Methods
Thirty-eight consecutive patients were identified who underwent LTIF followed by bilateral percutaneous transfacet fixation in the lateral position. Preoperative and 1-year postoperative VAS scores, and operative data were prospectively recorded. One-year outcomes were also assessed according to the MacNab criteria. Fusion was assessed at 1 year via computed tomography and dynamic radiography. Two-tailed Student’s t test was used to compare VAS scores.
Results
Twenty-six patients underwent fusion at L4–5, 11 at L3–4, and one at L2–3; two patients were lost to follow-up. Mean operative time was 148.0 ± 47.9 min; mean blood loss was 33.0 ± 26.1 ml; mean hospital stay was 53.5 ± 51.2 h. Mean preoperative VAS scores for back and leg pain were 7.4 ± 3.0 and 7.0 ± 2.9, respectively; mean postoperative VAS scores for back and leg pain were 1.9 ± 2.4 (p < 0.0001) and 2.0 ± 3.0 (p < 0.0001), respectively. Most (89 %) patients had some relief, 72 % good to excellent and 17 % fair outcomes; eleven percent had little to no relief. There was one postoperative complication (pulmonary embolus). All patients had evidence of solid bony fusion.
Conclusions
Percutaneous transfacet fixation in the lateral position is a safe and effective alternative for fixation after LTIF and may be associated with shorter operative time and less blood loss than other posterior fixation techniques.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Minimally invasive lateral lumbar interbody fusion has been shown to be effective in treating symptomatic degenerative disc disease while limiting operative morbidity [1–4]. In patients susceptible to higher rates of nonunion, concomitant posterior fixation is often recommended. Percutaneous transfacet screw fixation may be advantageous compared to traditional posterior pedicle screw fixation because the former requires smaller incisions, less muscular dissection, and less operative time while retaining similar biomechanical resistance in flexion and extension [5–9]. Voyadzis et al. [10] described a technique in which percutaneous transfacet screws are placed while the patient remains in a lateral position following a lateral interbody fusion. This method obviates the need to move the patient to the prone position prior to screw placement, thereby decreasing the overall operative time. In this study the authors seek to assess the safety and efficacy of percutaneous lumbar transfacet screw fixation in the lateral decubitus position following lateral interbody fusion after 1-year follow-up.
Methods
From July 2009 to December 2011, 38 consecutive patients with symptomatic degenerative disc disease between L2 and L5 underwent lateral lumbar interbody fusion followed by bilateral percutaneous transfacet screw fixation in the lateral decubitus position by two primary surgeons. All patients underwent extensive preoperative evaluations including detailed history and neurological examinations, magnetic resonance imaging (MRI), computed tomography (CT), and dynamic X-ray of the lumbosacral spine. Patients were selected if they presented with severe back pain and/or radiculopathy that was refractory to a trial of conservative management, which included physical therapy, narcotic, antispasmodic and nonsteroidal anti-inflammatory medications, and steroid injections. Selection criteria also included single-level lumbar degenerative disc disease with disc space collapse, foraminal stenosis and nerve root impingement. Preoperative visual analog scores (VAS) for both back and leg pain were recorded. Operative time, blood loss, and length of hospitalization were recorded for each patient. At 1-year follow-up, VAS scores for back and leg pain were recorded and outcomes were classified according to the MacNab criteria [11]. Mean preoperative and 1-year VAS scores were compared using the two-tailed Student’s t test. Flexion and extension radiographs and CTs of the lumbosacral spine were obtained and fusion was defined by evidence of contiguous bridging bone between adjacent vertebrae on CT imaging or the absence of malalignment or motion on dynamic radiographs. Exclusion criteria included patients with greater than 6-month preoperative narcotic use, presence of significant degenerative scoliosis, spondylolisthesis or treatment requiring fusion of multiple lumbar segments and worker’s compensation status.
Operative technique
The technique for lateral interbody fusion and transfacet screw fixation has previously been described [10, 12]. The patient is placed in the lateral decubitus position with the hip at the level of the break of the operating table. The leg is flexed to relax the psoas muscle on the side of the approach. Care is taken to properly pad the extremities and the chest, leg and hip areas are secured to the table with tape. Once the patient is secured, the table is flexed to allow optimum access to the disc space of interest. Anteroposterior (AP) and lateral fluoroscopic images are taken and a 2.5-cm lateral incision is marked directly over the disc space. The retroperitoneal space is accessed via blunt dissection through the lateral abdominal wall muscles and pre-peritoneal fat until the psoas muscle is visualized. The psoas is traversed with the first dilator with continuous electromyographic (EMG) monitoring to avoid neural injury. The position of the dilator is confirmed with AP and lateral fluoroscopic images. Once correct placement of the first dilator is achieved, a Kirschner wire (K-wire) is placed through the dilator into the disc space for anchoring. Subsequent dilators are inserted in similar fashion. A retractor is inserted over the dilators and secured to the table or directly to the vertebral bodies. The dilators and K-wire are removed and the exposure is inspected both visually and with a nerve probe for the presence of neural structures. The retractor is expanded to expose the disc and a discectomy is performed in standard fashion taking care to preserve and prepare the endplates and remove the contralateral annulus. An appropriately sized spacer packed with osteogenic material is selected and inserted into the prepared disc space. The retractor is removed and the incision is closed in anatomic layers.
Following the lateral interbody fusion, the patient remains in the lateral decubitus position and the operating table is adjusted back to the neutral position. A midline (1.5 cm) incision is made and extended deep through the fascia on both sides of the spinous process two levels above the target disc space. Using anterior–posterior fluoroscopic guidance, a Jamshidi needle is inserted and docked on the inferior articulating process of the superior vertebra at the level of interest. The entry point is the junction of a vertical line through the medial aspect of the ipsilateral pedicle and the inferior endplate of the superior vertebral body to be fused. A lateral image is used to direct the needle inferiorly through the facet joint and into the pedicle of the inferior vertebra. The needle is aimed laterally such that the screw tip will end at the inferolateral corner of the pedicle on an AP image. The final trajectory should aim the screw approximately 15° laterally and 30° caudally [13]. Once the trajectory is confirmed, the needle is anchored to the facet with a mallet. The stylet is removed and a K-wire is drilled through the facet joint and into the pedicle of the inferior vertebra. Serial dilators are inserted over the wire and the inner dilators are removed. A cannulated drill is inserted over the K-wire followed by a tap and a cannulated transfacet screw (Perpos, Interventional Spine). The screw is then compressed against the facet joint and the pull pin and K-wire are removed. The contralateral transfacet screw is deployed through the same incision in similar fashion.
Case illustration
A 69-year-old woman presented with moderate to severe (5 out of 10) right-sided low back pain without radiations into the groin and thigh refractory to multiple conservative treatment measures. Her physical examination revealed no neurological deficits. Magnetic resonance imaging studies revealed severe degenerative disc disease at L2–3 with right-sided disc space collapse and resulting lateral recess and foraminal stenosis and an early coronal deformity (Fig. 1a–c). The patient underwent a minimally invasive lateral interbody fusion at L2–3 for indirect decompression of her stenosis followed by percutaneous transfacet screw fixation in the lateral position. Surgery time was 81 min; estimated blood loss was 50 ml; and length of hospitalization was 64 h. She enjoyed complete resolution of her symptoms at 6 weeks and 1 year (Figs. 2a, b, 3a–e).
a One-year postoperative coronal CT of the lumbar spine revealing successful fusion (arrow) of L2–3 after lateral interbody fusion and facet screw insertion. b One-year postoperative sagittal CT of the lumbar spine revealing successful fusion of L2–3 (arrow) after lateral interbody fusion and facet screw insertion. c One-year postoperative axial CT of the lumbar spine revealing successful fusion of L3–4 after lateral interbody fusion and facet screw insertion. d One-year postoperative coronal CT of the lumbar spine revealing successful fusion of L3–4 after lateral interbody fusion and facet screw insertion. e Well-healed lateral and posterior incisions at 1 year
Results
Twenty-six patients underwent fusion at L4–5, 11 patients at L3–4, and one at L2–3. Two patients were lost to follow-up. Patient characteristics and outcomes are presented in Table 1. Operative times ranged from 85 to 270 min with a mean of 148.0 ± 47.9 min. Operative blood loss ranged from 10 to 100 ml with a mean of 33.0 ± 26.1 ml. Length of hospitalization ranged from 19 to 337 h with a mean of 53.5 ± 51.2 h. Patient 22 suffered a postoperative pulmonary embolus that required inpatient treatment with therapeutic intravenous heparin and oral warfarin. When this outlier is removed, the mean hospital stay decreases to less than 2 days: 45.8 ± 20.0 h. There were no intraoperative complications encountered or hardware failures.
At 1-year follow-up, all patients exhibited evidence of fusion on dynamic radiographs and/or computed tomography (Figs. 2a, b, 3a–d). Pre- and postoperative VAS scores are illustrated in Table 2. Mean preoperative VAS scores for back and leg pain were 7.4 ± 3.0 and 7.0 ± 2.9, respectively. Postoperatively, mean VAS scores for back and leg pain declined to 1.9 ± 2.4 (p < 0.0001) and 2.0 ± 3.0 (p < 0.0001), respectively (Table 2). Twenty-six out of 36 (72 %) patients enjoyed good or excellent outcomes based on the MacNab criteria; six (17 %) patients had fair improvement but still suffered some pain, and 4 (11 %) patients had little to no relief.
Of these patients with poor outcomes, two had initial improvement, but deteriorated due to untoward events or emergence of other pathologic entities, while the other two had persistence of either back or leg symptoms. Patient 13 had complete resolution of her back pain and her leg pain, but her symptoms reemerged to preoperative levels following a slip and fall after a snowstorm. Patient 14 had significant initial improvement in both back and leg pain but deteriorated within the first year. Her postoperative course was complicated by neck and upper extremity pain from C5 to C6 stenosis eventually requiring C5–6 anterior cervical discectomy and fusion 20 months after the lumbar fusion. Patient 23 had no improvement in back or leg pain and patient 32 had resolution of her back pain but continued to suffer significant legs symptoms postoperatively. Patient 6 suffered an acute exacerbation of pain several weeks after surgery; computed tomography of the lumbar spine (Fig. 4) demonstrated a fracture of the L5 vertebral body with graft subsidence. Her symptoms improved without additional surgical intervention.
Discussion
Degenerative disc disease is strongly correlated with increasing age and results in collapse of disc space height, segmental instability, and central, foraminal and lateral recess stenosis [14]. Degenerative disc disease is also frequently associated with facet arthropathy. These changes can lead to back and leg pain, along with sensory disturbances and weakness. Spondylodesis is the mainstay of surgical treatment for degenerative disc disease and has been shown to be effective in relieving back and leg pain [15–18].
Traditional options for instrumented lumbar fusion include posterolateral fusion with pedicle screw fixation, anterior interbody fusion (ALIF), posterior interbody fusion (PLIF) and transforaminal lumbar interbody fusion (TLIF). Although lumbar fusion in general has been shown to be effective in the setting of degenerative disc disease, these techniques differ in potential complications, fusion rates and biomechanical characteristics [19].
The anterior lumbar interbody fusion was first described by Capener [20]. Through an anterior transperitoneal or retroperitoneal approach, a thorough discectomy is performed followed by the insertion of a large intervertebral graft restoring the disc space height and indirectly decompressing the neural foramina and spinal canal. Operative complications associated with the anterior approach to the lumbar spine include vascular injury, sexual dysfunction from manipulation of the superior hypogastric plexus, deep venous thrombosis, ileus and bowel injury, and sympathetic dysfunction from damage to the lumbar sympathetic chain [21]. The reported incidence of vascular injury ranges from 1.9 to 11 % [22–25]. Quraishi et al. [26] performed a thorough review of complication rates in over 300 patients from a large tertiary referral center undergoing direct anterior lumbar approaches. They found vascular-related complications, at nearly 8 %, to be the most common complication with this approach. Most of these complications were minor and managed by the spinal surgeon.
A minimally invasive alternative to ALIF or posterior fusion is the transpsoas lateral interbody fusion [12]. From a lateral decubitus position, the lumbar spine is approached laterally through the psoas muscle allowing a thorough discectomy and placement of a large intervertebral graft similar to ALIF. Previous radiographic studies demonstrated substantial indirect decompression after successful interbody placement through the lateral approach [27]. Average disc height, foraminal height, and central canal diameter increased by 41.9, 13.5 and 33.1 %, respectively. Unlike a true anterior approach, the risks of major vascular or visceral injuries are reduced and an approach surgeon is unnecessary. Also, the anterior and posterior longitudinal ligaments are preserved preventing iatrogenic destabilization to the spine. Lateral interbody fusion has been consistently associated with decreased operative time, postoperative pain, intraoperative blood loss, and shorter hospital stays compared with traditional open interbody fusions [2–4, 28].
Lateral lumbar interbody fusion does have several inherent limitations. The approach is not an option for L5–S1 fusions and in L4–L5 cases where a high riding iliac crest precludes lateral access. Additionally, in cases of severe central stenosis, indirect decompression with an isolated lateral interbody placement may be insufficient. Reported complication rates associated with this procedure range from 2 to 30.4 % [1–4, 28]. The most common operative complications include postoperative hip flexion weakness due to direct psoas muscle injury and anterior thigh numbness likely secondary to injury to the genitofemoral nerve. The majority of these cases is transient and resolve within the first few weeks. One patient in our current series has chronic but mild dysesthesias of the thigh. We observed no cases of permanent psoas weakness or neuropathic pain.
Stand-alone interbody cages effectively increase the biomechanical stability across the treated segment in flexion, lateral bending, and to a lesser extent, axial rotation with little effect in reducing extension [29, 30]. In select cases, stand-alone lateral interbody fusions have been shown to be clinically effective with a high fusion rate [31]. However, in the setting of instability, additional instrumentation is warranted. Biomechanical studies of interbody cage stabilizations via both anterior and posterior approaches have demonstrated that the addition of pedicle screw and rod fixation decreases segmental range of motion [7, 9, 29]. Anjarwalla et al. [32] found that the addition of pedicle screw stabilization considerably increased the fusion rate with ALIFs on follow-up thin-section computed tomography imaging. While pedicle screw instrumentation following a lateral interbody fusion adds stability, it requires additional incision(s), posterior muscle dissection, and repositioning. Alternatively, pedicle screws can be placed in the lateral position, but this technique can be cumbersome, especially placement of the rod on the dependent or inferior side.
Lateral plates placed following a lateral lumbar interbody fusion confer the advantages of relative ease of insertion and no additional incision or repositioning required. Although a lateral plate provides some stabilization, it may be inferior to transpedicular fixation in flexion, extension and lateral bending [7]. Posterior interspinous fixation devices are also an option to augment the lateral interbody fusion and were shown in a recent biomechanical study to be effective in reducing range of motion, especially in flexion–extension [33].
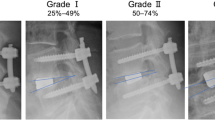
Other posterior fixation options include translaminar and transfacet screws. The use of screw fixation in the spine actually began with transfacet screws innovated by King [34, 35], and modified by Boucher [36] when the facet screw was lengthened to incorporate the ipsilateral pedicle and posterior vertebral body. Translaminar screws were introduced by Magerl [37] and involve placement of a long screw in the lamina at the base of the spinous process crossing transversely in the plane of the contralateral lamina, facet, and transverse process. Both translaminar and transfacet screws confer significant rigidity to the posterior elements. These techniques compare favorably with one another and with pedicle screw fixation in biomechanical studies [5–9]. In a 2013 cadaveric biomechanical study by Kretzer et al. [38], two types of facet screw instrumentation systems were compared with pedicle screw instrumentation following lateral lumbar discectomy and interbody graft placement. Both facet screw constructs were shown to be equally as effective as pedicle screws at reducing segmental range of motion. Furthermore, the increased rigidity conferred by pedicle screw constructs may increase stress shielding on the intervertebral graft, thereby decreasing the likelihood of successful fusion [5, 38]. Conversely, an interbody graft and transfacet screw construct may increase the likelihood of graft subsidence, particularly with inadvertent violation of the endplates during disc space preparation and/or in patients with osteopenia or osteoporosis. Indeed, caution should be exercised in patients with osteopenia, and severe osteoporosis is a relative contraindication to transfacet screw fixation because of the increased likelihood of suboptimal fixation and screw back out. We found a slight degree of graft subsidence in the majority of the cases studied (Fig. 5a, b). None of these cases led to recurrent stenosis from failure of indirect decompression. Careful patient selection and meticulous preparation without violation of the endplates when combined with the insertion of larger interbody grafts should reduce this risk [39].
Transfacet screws are more easily deployed than pedicle screws and largely avoid the risk of central or foraminal breech associated with translaminar screws. Minimally invasive techniques are available for both transfacet and pedicle screws, but percutaneous pedicle screws require more time, incisions, and muscle dissection, while transfacet screws can be deployed in the lateral decubitus position, considerably decreasing operative time in lateral interbody fusion cases. In our current study, the mean operative time was relatively short at less than 2 h and a half (148.0 ± 47.9 min) and intraoperative blood loss was low (33.0 ± 26.1 ml), thus exposing patients to less risk from anesthesia and the need for blood transfusions. Furthermore, the average hospital stay was just over 2 days at 53.5 ± 51.2 h, indicating that patients were able to ambulate early, an important factor in reducing complications related to thromboembolism, pneumonia, urinary tract infection, and others. All of these factors could contribute to increased patient satisfaction and improved cost-effectiveness.
While there are few direct comparisons in the literature, the operative time, blood loss, and hospital stay in our study compare favorably with other circumferential fusion techniques. In studies of MI-TLIF, mean operative time ranged from 100 to 300 min, mean blood loss ranged from 125 to 216 ml, and mean hospital stay range was 4 days [40–43]. Furthermore, the fusion rate and reduction in pain also compare favorably to other fusion techniques. Transfacet screw fixation was utilized in our study to augment interbody fusion, not as a stand-alone method of facet arthrodesis. Indeed, facet arthrodesis was rarely observed on 1-year follow-up CT imaging. Transfacet screws could be used for the treatment of isolated facet disease with the added insertion of bone grafting material during preparation of screw placement, but we are unaware of data to support this indication.
Most patients in our current study had significant reductions in leg and back pain following LLIF and transfacet screw fixation. Seventy-two percent of patients experienced good or excellent outcome as define by the MacNab criteria, and there were significant reductions in the mean VAS scores for leg and back pain. These results are comparable with other methods of circumferential fusion. However, some patients did not experience significant improvement in back and/or leg pain. Six patients experienced fair outcomes, and four had poor outcomes. There were 8 patients who had little to no improvement in postoperative leg pain as reported by VAS scores. Many of these patients were able to tolerate this leg pain with occasional analgesics and other pain management strategies and none required reoperation. The lack of improvement in these patients could be due to several factors including failure of indirect decompression or graft subsidence and recurrence of stenosis, but follow-up imaging failed to demonstrate significant stenosis. Furthermore, many of these patients had chronic long-standing leg pain prior to surgical intervention. The apparent lack of improvement may also highlight limitations of self-reported metrics, and underscores the need to report other quality of life measures. We acknowledge that this is a limitation of the current study. However, in our experience, a great majority of patients treated with LLIF and transfacet screws experience improved quality of life with respect to the need for pain management and ability to return to preoperative activity levels.
In addition to favorable patient outcomes, intraoperative parameters and short hospital stay, there were also no screw-related complications in our current study. There were no peri-operative nerve injuries, incidental durotomies, or cerebrospinal fluid leaks related to screw misplacement. These complications are also relatively rare with percutaneous pedicle screw placement, but do occur 1–2 % of the time. Additionally, there were no delayed screw-related complications such as screw back out, screw fracture, or pseudoarthrosis. These complications could lead to further surgery and continued or worsening pain. These findings indicate that transfacet screw fixation is a safe and effective method for providing increased stabilization to supplement lateral interbody fusion.
Conclusion
We present our experience of 38 patients who underwent single-level lateral interbody fusion followed by percutaneous transfacet screw placement in the lateral decubitus position. There were no operative complications. Mean postoperative VAS scores dropped by 74 and 72 % for back and leg pain, respectively, compared to their preoperative levels. Eighty-nine percent of patients had some improvement in back and leg pain and 72 % had good or excellent outcomes at 1-year follow-up. Percutaneous lumbar transfacet screw fixation in the lateral decubitus position represents a safe and effective adjunct to lateral lumbar interbody fusion. Furthermore, this technique may reduce operative time, blood loss, and length of hospital stay in selected patients who require posterior fixation in addition to interbody fusion.
References
Rodgers WB, Gerber EJ, Patterson J (2011) Intraoperative and early postoperative complications in extreme lateral interbody fusion: an analysis of 600 cases. Spine (Phila Pa 1976) 36:26–32
Isaacs RE, Hyde J, Goodrich JA, Rodgers WB, Phillips FM (2010) A prospective, nonrandomized, multicenter evaluation of extreme lateral interbody fusion for the treatment of adult degenerative scoliosis: perioperative outcomes and complications. Spine (Phila Pa 1976) 35:S322–S330
Dakwar E, Cardona RF, Smith DA, Uribe JS (2010) Early outcomes and safety of the minimally invasive, lateral retroperitoneal transpsoas approach for adult degenerative scoliosis. Neurosurg Focus 28:E8
Youssef JA, McAfee PC, Patty CA, Raley E, De Bauche S, Shucosky E, Chotikul L (2010) Minimally invasive surgery: lateral approach interbody fusion: results and review. Spine (Phila Pa 1976) 35:S302–S311
Ferrara LA, Secor JL, Jin BH, Wakefield A, Inceoglu S, Benzel EC (2003) A biomechanical comparison of facet screw fixation and pedicle screw fixation: effects of short-term and long-term repetitive cycling. Spine (Phila Pa 1976) 28:1226–1234
Jang JS, Lee SH (2005) Clinical analysis of percutaneous facet screw fixation after anterior lumbar interbody fusion. J Neurosurg Spine 3:40–46
Kim SM, Lim TJ, Paterno J, Kim DH (2004) A biomechanical comparison of supplementary posterior translaminar facet and transfaceto pedicular screw fixation after anterior lumbar interbody fusion. J Neurosurg Spine 1:101–107
Mahar A, Kim C, Oka R, Odell T, Perry A, Mirkovic S, Garfin S (2006) Biomechanical comparison of a novel percutaneous transfacet device and a traditional posterior system for single level fusion. J Spinal Disord Tech 19:591–594
Chin KR, Reis MT, Reyes PM, Newcomb AG, Neagoe A, Gabriel JP, Sung RD, Crawford NR (2013) Stability of transforaminal lumbar interbody fusion in the setting of retained facets and posterior fixation using transfacet or standard pedicle screws. Spine J. doi:10.1016/j.spinee.2013.06.103
Voyadzis JM, Anaizi AN (2013) Minimally invasive lumbar transfacet screw fixation in the lateral decubitus position after extreme lateral interbody fusion: a technique and feasibility study. J Spinal Disord Tech 26:98–106
Macnab I (1971) Negative disc exploration. An analysis of the causes of nerve-root involvement in sixty-eight patients. J Bone Joint Surg Am 53:891–903
Ozgur BM, Aryan HE, Pimenta L, Taylor WR (2006) Extreme lateral interbody fusion (XLIF): a novel surgical technique for anterior lumbar interbody fusion. Spine J 6:435–443
Su BW, Cha TD, Kim PD, Lee J, April EW, Weidenbaum M, Albert TJ, Vaccaro AR (2009) An anatomic and radiographic study of lumbar facets relevant to percutaneous transfacet fixation. Spine (Phila Pa 1976) 34:E384–E390
Buckwalter JA (1995) Aging and degeneration of the human intervertebral disc. Spine (Phila Pa 1976) 20:1307–1314
Verbiest H (1954) A radicular syndrome from developmental narrowing of the lumbar vertebral canal. J Bone Joint Surg Br 36:230–237
Matsudaira K, Yamazaki T, Seichi A, Takeshita K, Hoshi K, Kishimoto J, Nakamura K (2005) Spinal stenosis in grade I degenerative lumbar spondylolisthesis: a comparative study of outcomes following laminoplasty and laminectomy with instrumented spinal fusion. J Orthop Sci 10:270–276
Weinstein JN, Tosteson TD, Lurie JD, Tosteson A, Blood E, Herkowitz H, Cammisa F, Albert T, Boden SD, Hilibrand A, Goldberg H, Berven S, An H (2010) Surgical versus nonoperative treatment for lumbar spinal stenosis four-year results of the Spine Patient Outcomes Research Trial. Spine (Phila Pa 1976) 35:1329–1338
Martin CR, Gruszczynski AT, Braunsfurth HA, Fallatah SM, O’Neil J, Wai EK (2007) The surgical management of degenerative lumbar spondylolisthesis: a systematic review. Spine (Phila Pa 1976) 32:1791–1798
Fritzell P, Hagg O, Wessberg P, Nordwall A (2001) 2001 Volvo Award Winner in Clinical Studies: lumbar fusion versus nonsurgical treatment for chronic low back pain: a multicenter randomized controlled trial from the Swedish Lumbar Spine Study Group. Spine (Phila Pa 1976) 26:2521–2532 discussion 2532–2524
Capener N (1932) Spondylolisthesis. Br J Surg 19:374–386
Rajaraman V, Vingan R, Roth P, Heary RF, Conklin L, Jacobs GB (1999) Visceral and vascular complications resulting from anterior lumbar interbody fusion. J Neurosurg 91:60–64
Brau SA, Delamarter RB, Schiffman ML, Williams LA, Watkins RG (2004) Vascular injury during anterior lumbar surgery. Spine J 4:409–412
Hamdan AD, Malek JY, Schermerhorn ML, Aulivola B, Blattman SB, Pomposelli FB Jr (2008) Vascular injury during anterior exposure of the spine. J Vasc Surg 48:650–654
Fantini GA, Pappou IP, Girardi FP, Sandhu HS, Cammisa FP Jr (2007) Major vascular injury during anterior lumbar spinal surgery: incidence, risk factors, and management. Spine (Phila Pa 1976) 32:2751–2758
Sasso RC, Best NM, Mummaneni PV, Reilly TM, Hussain SM (2005) Analysis of operative complications in a series of 471 anterior lumbar interbody fusion procedures. Spine (Phila Pa 1976) 30:670–674
Quraishi NA, Konig M, Booker SJ, Shafafy M, Boszczyk BM, Grevitt MP, Mehdian H, Webb JK (2013) Access related complications in anterior lumbar surgery performed by spinal surgeons. Eur Spine J 22(Suppl 1):S16–S20
Pimenta L, Oliveira L, Schaffa T, Coutinho E, Marchi L (2011) Lumbar total disc replacement from an extreme lateral approach: clinical experience with a minimum of 2 years’ follow-up. J Neurosurg Spine 14:38–45
Oliveira L, Marchi L, Coutinho E, Pimenta L (2010) A radiographic assessment of the ability of the extreme lateral interbody fusion procedure to indirectly decompress the neural elements. Spine (Phila Pa 1976) 35:S331–S337
Lund T, Oxland TR, Jost B, Cripton P, Grassmann S, Etter C, Nolte LP (1998) Interbody cage stabilisation in the lumbar spine: biomechanical evaluation of cage design, posterior instrumentation and bone density. J Bone Joint Surg Br 80:351–359
Oxland TR, Lund T (2000) Biomechanics of stand-alone cages and cages in combination with posterior fixation: a literature review. Eur Spine J 9(Suppl 1):S95–S101
Marchi L, Abdala N, Oliveira L, Amaral R, Coutinho E, Pimenta L (2012) Stand-alone lateral interbody fusion for the treatment of low-grade degenerative spondylolisthesis. Sci World J 2012:456346. doi:10.1100/2012/456346
Anjarwalla NK, Morcom RK, Fraser RD (2006) Supplementary stabilization with anterior lumbar intervertebral fusion–a radiologic review. Spine (Phila Pa 1976) 31:1281–1287
Fogel GR, Parikh RD, Ryu SI, Turner AW (2014) Biomechanics of lateral lumbar interbody fusion constructs with lateral and posterior plate fixation: laboratory investigation. J Neurosurg Spine 20:291–297
King D (1948) Internal fixation for lumbosacral fusion. J Bone Joint Surg Am 30A:560–565
King D (1944) Internal fixation for lumbosacral fusion. Am J Surg 66:357–361
Boucher HH (1959) A method of spinal fusion. J Bone Joint Surg Br 41:248–259
Magerl FP (1984) Stabilization of the lower thoracic and lumbar spine with external skeletal fixation. Clin Orthop Relat Res 189:125–141
Kretzer RM, Molina C, Hu N, Umekoji H, Baaj AA, Serhan H, Cunningham BW (2013) A comparative biomechanical analysis of stand alone versus facet screw and pedicle screw augmented lateral interbody arthrodesis: an in vitro human cadaveric model. J Spinal Disord Tech [Epub ahead of print]
Le TV, Baaj AA, Dakwar E, Burkett CJ, Murray G, Smith DA, Uribe JS (2012) Subsidence of polyetheretherketone intervertebral cages in minimally invasive lateral retroperitoneal transpsoas lumbar interbody fusion. Spine (Phila Pa 1976) 37:1268–1273
Ghahreman A, Ferch RD, Rao PJ, Bogduk N (2010) Minimal access versus open posterior lumbar interbody fusion in the treatment of spondylolisthesis. Neurosurgery 66:296–304 discussion 304
Scheufler KM, Dohmen H, Vougioukas VI (2007) Percutaneous transforaminal lumbar interbody fusion for the treatment of degenerative lumbar instability. Neurosurgery 60:203–212 discussion 212–203
Peng CW, Yue WM, Poh SY, Yeo W, Tan SB (2009) Clinical and radiological outcomes of minimally invasive versus open transforaminal lumbar interbody fusion. Spine (Phila Pa 1976) 34:1385–1389
Adogwa O, Parker SL, Bydon A, Cheng J, McGirt MJ (2011) Comparative effectiveness of minimally invasive versus open transforaminal lumbar interbody fusion: 2-year assessment of narcotic use, return to work, disability, and quality of life. J Spinal Disord Tech 24:479–484
Acknowledgments
The work herein has not been published elsewhere, nor is it under consideration for publication elsewhere. All authors have reviewed this work and consent to its publication. The corresponding author had access to all data and is responsible for the decision to submit this manuscript.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rhee, J.W., Petteys, R.J., Anaizi, A.N. et al. Prospective evaluation of 1-year outcomes in single-level percutaneous lumbar transfacet screw fixation in the lateral decubitus position following lateral transpsoas interbody fusion. Eur Spine J 24, 2546–2554 (2015). https://doi.org/10.1007/s00586-015-3934-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-015-3934-x