Abstract
Purpose
Explore the relationships between preoperative findings and clinical outcome following lumbar disc surgery, and investigate the prognostic value of physical examination findings after accounting for information acquired from the clinical history.
Methods
We recruited 55 adult patients scheduled for first time, single-level lumbar discectomy. Participants underwent a standardized preoperative evaluation including real-time ultrasound imaging assessment of lumbar multifidus function, and an 8-week postoperative rehabilitation programme. Clinical outcome was defined by change in disability, and leg and low back pain (LBP) intensity at 10 weeks. Linear regression models were used to identify univariate and multivariate predictors of outcome.
Results
Univariate predictors of better outcome varied depending on the outcome measure. Clinical history predictors included a greater proportion of leg pain to LBP, pain medication use, greater time to surgery, and no history of previous physical or injection therapy. Physical examination predictors were a positive straight or cross straight leg raise test, diminished lower extremity strength, sensation or reflexes, and the presence of postural abnormality or pain peripheralization. Preoperative pain peripheralization remained a significant predictor of improved disability (p = 0.04) and LBP (p = 0.02) after accounting for information from the clinical history. Preoperative lumbar multifidus function was not associated with clinical outcome.
Conclusions
Information gleaned from the clinical history and physical examination helps to identify patients more likely to succeed with lumbar disc surgery. While this study helps to inform clinical practice, additional research confirming these results is required prior to confident clinical implementation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Lumbar disc herniation is the most common cause of radicular leg pain and sometimes requires surgery [1]. While rates of lumbar disc surgery have increased in the United States [2], clinical outcomes are suboptimal owing to recalcitrant pain, disability, and reduced quality of life [3, 4]. Consequently, failed disc surgery has been described as a major problem, highlighting the importance of appropriate patient selection [5].
Patient selection for lumbar disc surgery is usually based on findings from the history and physical examination. Yet, there is limited evidence to inform clinicians’ knowledge of a patient’s clinical course and prognosis following lumbar disc surgery [6]. Several studies have identified the prognostic value of variables extracted from the patient history. Age [7], sex [8], time to surgery [9], preoperative pain level [10], obesity [11], and time on sick leave [7], are associated with clinical outcome following lumbar disc surgery. There is conflicting evidence regarding the prognostic value of many predictors and even less is known about the role of physical examination findings [6, 12]. Moreover, the few studies that have examined the prognostic value of physical examination outcomes are prone to methodological concerns and conflicting findings [6].
Emerging evidence suggests that lumbar multifidus (LM) function has clinical relevance to patients with lumbar disc herniation being considered for surgery. Lumbar disc herniation is associated with LM atrophy and diminished LM function at the involved spinal level [13, 14], and intraoperative LM injury may contribute to the development of “failed back syndrome” [15].
There is a clear need to better identify factors that predict outcome following lumbar disc surgery. Therefore, the aims of this study were to (1) explore the relationships between preoperative clinical history, physical examination and LM muscle function with clinical outcome following lumbar disc surgery and (2) investigate the prognostic value of physical examination findings after accounting for information acquired from the clinical history.
Methods
Study design
This was a secondary analysis of a parallel group randomized clinical trial comparing two postoperative rehabilitation protocols following lumbar disc surgery [16]. As there were no between-group differences in clinical outcome, patients from both groups were combined into a single cohort for analysis in the current study. All participants underwent a standardized preoperative evaluation by trained study personnel within 2 weeks of surgery and participated in an 8-week postoperative rehabilitation programme starting 2 weeks after surgery. The participants were then re-evaluated at the end of postoperative week 10. The study protocol was approved by the Institutional Review Board of the University of Utah, and all participants provided consent prior to study enrolment.
Participants
Participants were recruited from academic and private neurological and orthopaedic spine surgery settings. We included patients aged 18–60 years, with imaging confirmed lumbar disc herniation, and identified as candidates for single-level lumbar discectomy or microdiscectomy by their spine surgeon. Potential participants were excluded if they had prior lumbar spine surgery, surgical procedures other than discectomy (e.g., fusion), or significant co-morbidities or perioperative complications representing a contraindication to exercise.
Postoperative rehabilitation
The full details of the rehabilitation programmes used in this study have been reported elsewhere [16]. Briefly, at postoperative week 2, all participants underwent an 8-week exercise programme comprising weekly supervised exercise sessions and daily home exercises. Treatment consisted of a walking programme, range of motion, and trunk muscle stability exercises as well as advice about activities of daily living and health behaviours.
Potential predictors of clinical outcome
Demographic and historical variables
Demographic data included age, sex, and body mass index (BMI). Smoking status was classified as current smoking behaviour or a lifetime history of smoking at least 100 cigarettes. Potential for secondary gain was explored by asking whether the participant was currently represented by an attorney or receiving workers compensation. Additionally, we inquired about five aspects of the clinical history pertinent to their current pain episode: (1) time from episode onset to surgery, (2) previous physical therapy treatment, (3) current pain medication use, (4) previous injection therapy (e.g., epidural steroid injection) and (5) proportion of leg pain to low back pain (LBP) calculated using reports of pain intensity from numeric pain rating scales [leg pain intensity/(LBP intensity + leg pain intensity)].
Physical examination variables
Physical examinations were performed as part of the preoperative evaluation and involved tests related to neurologic status, posture and movement, as well as procedures purported to assess spinal stability. We examined participants’ lower extremity sensation, strength, and muscle stretch reflexes and performed the straight leg raise [17] and cross straight leg raise [18] manoeuvres to assess for lower extremity neural tension.
Standing posture was visually evaluated for postural deformity [19] and judged to be normal or abnormal. Abnormal standing posture was defined by the presence of excessive lumbar kyphosis, or frontal plane deviation of the pelvis to the right or left. The patient’s response to end-range loading was evaluated by monitoring for pain centralization and peripheralization during sustained extension in the prone position, and single and repeated repetitions of lumber extension, flexion, and side-gliding while standing. We defined centralization as occurring when the position or movement caused an individual’s symptoms to move proximally toward the midline of the spine. Peripheralization was considered to occur when symptoms moved more distally away from the midline of the spine. The identification of centralization and peripheralization with these procedures has excellent interrater agreement [20].
We examined a collection of tests associated with muscular instability of the spine. During lumbar flexion testing, the presence or absence of at least one of four aberrant movement patterns were identified: instability catch, Gower sign, reversal of lumbopelvic rhythm, painful arc of motion [21]. Additionally, we examined participant’s response to the prone instability test [22].
Muscle function was assessed by measuring the percent change in LM thickness from rest to submaximal contraction. We acquired brightness-mode, real-time ultrasound images using a Sonosite MicroMaxx (Sonosite Inc. Bothell, WA) and a 60-mm, 2–5 MHz curvilinear array. The contraction task involved a contralateral arm lift while the participant held a hand weight normalized to body mass. This task results in approximately 30 % of the maximum voluntary isometric contraction for the LM [23]. Three images of each muscle, in each state, were acquired on the left and right sides of the operative spinal segment [24]. Additional details have been previously reported [25] and this approach has been demonstrated to have good rater reliability [25, 26] and concurrent validity [27].
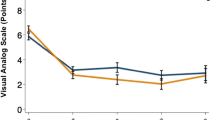
Measures of clinical outcome
Clinical outcomes were defined by change in disability and pain intensity from the preoperative assessment to the completion of the rehabilitation programme after 10 postoperative weeks. LBP related disability was assessed using the modified Oswestry Disability Questionnaire (OSW). This questionnaire has demonstrated good test–retest reliability, responsiveness, and a minimum clinically important difference (MCID) between six and ten points [28, 29]. Low back and leg pain intensity were reported on an 11-point numeric pain rating scale (NPRS) with possible scores ranging from 0 (“no pain”) to 10 (“worst imaginable pain”). We measured current pain intensity as well as the “best” and “worst” pain intensity in the preceding 24 h [30] and averaged the three scores to estimate pain intensity. The NPRS has been demonstrated to have good reliability, responsiveness, criterion validity, and an MCID of two points [28, 30].
Statistical analyses
Data management and statistical analyses were performed using IBM SPSS version 21.0 software (IBM Corp, Armonk, NY). The relationships between potential predictors and clinical outcome were explored with univariate and multivariate analyses. We calculated unstandardized beta coefficients (b) from separate univariate linear regressions between the potential predictors and 10-week change scores for each clinical outcome (disability, leg pain intensity, LBP intensity). Potential predictors included clinical history, physical examination, and muscle function variables.
Variables associated with clinical outcome at the univariate stage were then entered into separate hierarchical linear regression models. To control for the variance in clinical outcome explained by information gained from the patient history, historical variables identified by the univariate analyses (p < 0.05) were force entered in the first step. In addition, to control for the effect of baseline clinical status on the change in outcome, the baseline score of the relevant outcome variable was also entered into the model at this point. To investigate the prognostic value of the physical examination, beyond information gained from the clinical history, physical examination variables identified by the univariate analyses (p < 0.10) were introduced to the model with stepwise entry. This hierarchical approach was used to determine if the presence of the physical examination variables would further improve model fit after accounting for the variance explained by historical information. Adjusted R 2 values were calculated at each step, reflecting the variance in the dependent variable explained by the independent variables and adjusted for the number of independent variables entered into the regression model. Standardized beta coefficients (β) were generated for each variable included in the final model and adjusted R 2 values were calculated at each step. Alpha was 0.05 and missing data were handled with pairwise deletion.
Results
We were unable to acquire muscle function measures from 10 participants at the preoperative assessment. The expected bony landmarks could not be visualized in 6 participants and 4 participants were unable to tolerate the test position. Thus, clinical history and physical examination data were available from 55 participants and muscle function data from 45 participants (Fig. 1). Baseline descriptive statistics and measures of clinical outcome are presented in Tables 1 and 2, respectively.
The results of the univariate analyses between the historical and physical variables and each clinical outcome are presented in Table 3. Greater baseline leg pain relative to LBP was associated with more improvement in disability (b = 0.28, p = 0.004), and leg pain intensity (b = 0.06, p < 0.001), but less improvement in low back pain intensity (b = −0.04, p = 0.005). Longer time to surgery was associated with more improvement in disability (b = 0.03, p = 0.030) and more improvement in leg pain intensity was reported among participants who had received pain medication (b = 1.97, p = 0.042). Conversely, less improvement in leg pain intensity was associated with preoperative physical (b = −1.54, p = 0.026) and injection therapy (b = −1.41, p = 0.049).
Several physical examination variables were associated with clinical outcome in the univariate analyses. The presence of preoperative postural deformity was associated with greater improvement in disability (b = 13.99, p = 0.029), leg pain intensity (b = 2.09, p < 0.023), and LBP intensity (b = 2.32, p < 0.003). Greater improvement in disability was associated with the presence of a positive straight leg raise test (b = 14.88, p < 0.010), cross straight leg raise test (b = 14.31, p < 0.042), pain peripheralization (b = 14.76, p < 0.036), as well as diminished reflexes (b = 14.10, p < 0.004), sensation (b = 12.44, p < 0.012) or strength (b = 11.87, p < 0.016) prior to surgery. Finally, having a positive straight leg raise test (b = 2.43, p < 0.003), or strength deficit (b = 1.54, p < 0.031) was associated with more improvement in leg pain intensity. There were no relationships between LM function and clinical outcome.
The results of the multivariate analyses are presented in Tables 4, 5 and 6. After controlling for the variance attributable to the baseline outcome score and significant historical predictors from the univariate analyses, the presence of pain peripheralization at baseline was associated with greater improvement in both disability (β = 0.24, p = 0.044) and low back pain intensity (β = 0.33, p = 0.002) after 10 postoperative weeks. Physical examination variables were not associated with change in leg pain intensity after controlling for the variance explained by baseline leg pain intensity and information from the clinical history. The total variance in clinical outcome explained by each of the final models (adjusted R 2 values) ranged from 31 to 61 % (p < 0.05).
Discussion
This was the first study to investigate the value of physical examination findings, beyond the information gained from the patient history, as well as the role of preoperative LM function among patients undergoing lumbar disc surgery and postoperative rehabilitation. We identified several preoperative variables from the clinical history and physical examination with evidence of prognostic importance, as demonstrated by their relation to clinical outcome. The multivariate analyses indicated that the presence of preoperative pain peripheralization was associated with improved disability and low back pain intensity, even after accounting for the variance explained by information from the patient’s clinical history. Preoperative LM function demonstrated no relationship with clinical outcome following lumbar disc surgery and postoperative rehabilitation.
Previous studies have not examined the prognostic value of pain peripheralization among patients undergoing lumbar disc surgery. However, one previous study reported that among patients with low back pain and sciatica, the presence of pain peripheralization was associated with improved outcome following therapeutic lumbar traction and exercise [31]. While pain centralization has been shown in several previous studies to be a positive prognostic indicator for patients with lumbar spine disorders undergoing non-operative therapy [32], it was not associated with outcome following surgery in the current study. Traditional methods of identifying change in leg pain location in response to changes in spinal movement or position have been reported to have unacceptable rater agreement [33]. We assessed pain peripheralization using a simplified approach with excellent interrater agreement. Therefore, this method may be of value to clinicians evaluating patients being considered for lumbar disc surgery.
From a clinical perspective, it is reassuring that many of the physical examination predictors of clinical outcome included findings thought to be typical of patients with lumbar disc herniation. While this finding accords with several previous studies [34–36], it conflicts with others [37, 38]. A more consistent predictor of outcome following lumbar disc surgery has been the presence of predominant leg pain [36, 37], a finding which agrees with our results.
The current study results should be considered in light of several limitations. We explored the associations of preoperative predictors with 10-week clinical outcomes, thus their relevance to long-term outcome is unknown. Nonetheless, previous research indicates that 2-month outcomes following lumbar disc surgery are strongly associated with clinical status after 14 postoperative months, therefore the value of these predictors may extend to longer duration follow-up [39]. While there was some variation of predictors between the different outcome measures, this is consistent with previous research indicating that most patients report inconsistent outcomes following lumbar spine surgery when multiple measures are implemented [40]. Finally, the sample size relative to the number of predictor variables in some analysis may have resulted in suboptimal statistical power and model overfit.
Information gleaned from the clinical history and physical examination was associated with clinical outcome following lumbar disc surgery and postoperative rehabilitation. After accounting for the variance explained by the clinical history, the presence of preoperative pain peripheralization predicted a better clinical outcome. While this study may inform clinical practice, additional research confirming these results should be carried out prior to confident implementation by clinicians.
References
Gibson JN, Waddell G (2007) Surgical interventions for lumbar disc prolapse: updated Cochrane Review. Spine 32:1735–1747. doi:10.1097/BRS.0b013e3180bc2431
Deyo RA, Mirza SK (2006) Trends and variations in the use of spine surgery. Clin Orthop Relat Res 443:139–146. doi:10.1097/01.blo.0000198726.62514.75
Carragee EJ, Kim DH (1997) A prospective analysis of magnetic resonance imaging findings in patients with sciatica and lumbar disc herniation. Correlation of outcomes with disc fragment and canal morphology. Spine 22:1650–1660
Hakkinen A, Kautiainen H, Sintonen H, Ylinen J (2005) Health related quality of life after lumbar disc surgery: a prospective study of 145 patients. Disabil Rehabil 27:94–100. doi:10.1080/09638280400007430
Carragee EJ, Han MY, Suen PW, Kim D (2003) Clinical outcomes after lumbar discectomy for sciatica: the effects of fragment type and anular competence. J Bone Joint Surg Am 85-A:102–108
Mannion AF, Elfering A (2006) Predictors of surgical outcome and their assessment. Eur Spine J 15(Suppl 1):S93–S108. doi:10.1007/s00586-005-1045-9
Silverplats K, Lind B, Zoega B, Halldin K, Rutberg L, Gellerstedt M, Brisby H (2010) Clinical factors of importance for outcome after lumbar disc herniation surgery: long-term follow-up. Eur Spine J 19:1459–1467. doi:10.1007/s00586-010-1433-7
Peul WC, Brand R, Thomeer RT, Koes BW (2008) Influence of gender and other prognostic factors on outcome of sciatica. Pain 138:180–191. doi:10.1016/j.pain.2007.12.014
Rothoerl RD, Woertgen C, Brawanski A (2002) When should conservative treatment for lumbar disc herniation be ceased and surgery considered? Neurosurg Rev 25:162–165
Junge A, Dvorak J, Ahrens S (1995) Predictors of bad and good outcomes of lumbar disc surgery. A prospective clinical study with recommendations for screening to avoid bad outcomes. Spine 20:460–468
Rihn JA, Kurd M, Hilibrand AS, Lurie J, Zhao W, Albert T, Weinstein J (2013) The influence of obesity on the outcome of treatment of lumbar disc herniation: analysis of the Spine Patient Outcomes Research Trial (SPORT). J Bone Joint Surg Am 95:1–8. doi:10.2106/JBJS.K.01558
Birkmeyer NJ, Weinstein JN, Tosteson AN, Tosteson TD, Skinner JS, Lurie JD, Deyo R, Wennberg JE (2002) Design of the Spine Patient outcomes Research Trial (SPORT). Spine (Phila Pa 1976) 27:1361–1372
Yoshihara K, Nakayama Y, Fujii N, Aoki T, Ito H (2003) Atrophy of the multifidus muscle in patients with lumbar disk herniation: histochemical and electromyographic study. Orthopedics 26:493–495
Yoshihara K, Shirai Y, Nakayama Y, Uesaka S (2001) Histochemical changes in the multifidus muscle in patients with lumbar intervertebral disc herniation. Spine 26:622–626
Sihvonen T, Herno A, Paljarvi L, Airaksinen O, Partanen J, Tapaninaho A (1993) Local denervation atrophy of paraspinal muscles in postoperative failed back syndrome. Spine 18:575–581
Hebert JJ, Fritz JM, Thackeray A, Koppenhaver SL, Teyhen D (2015) Early multimodal rehabilitation following lumbar disc surgery: a randomised clinical trial comparing the effects of two exercise programmes on clinical outcome and lumbar multifidus muscle function. Br J Sports Med 49:100–106. doi:10.1136/bjsports-2013-092402
Majlesi J, Togay H, Unalan H, Toprak S (2008) The sensitivity and specificity of the Slump and the straight leg raising tests in patients with lumbar disc herniation. J Clin Rheumatol 14:87–91. doi:10.1097/RHU.0b013e31816b2f99
Kosteljanetz M, Bang F, Schmidt-Olsen S (1988) The clinical significance of straight-leg raising (Lasegue’s sign) in the diagnosis of prolapsed lumbar disc. Interobserver variation and correlation with surgical finding. Spine (Phila Pa 1976) 13:393–395
Kilpikoski S, Airaksinen O, Kankaanpaa M, Leminen P, Videman T, Alen M (2002) Interexaminer reliability of low back pain assessment using the McKenzie method. Spine (Phila Pa 1976) 27:E207–E214
Fritz JM, Delitto A, Vignovic M, Busse RG (2000) Interrater reliability of judgments of the centralization phenomenon and status change during movement testing in patients with low back pain. Arch Phys Med Rehabil 81:57–61
Hebert JJ, Koppenhaver SL, Magel JS, Fritz JM (2010) The relationship of transversus abdominis and lumbar multifidus activation and prognostic factors for clinical success with a stabilization exercise program: a cross-sectional study. Arch Phys Med Rehabil 91:78–85. doi:10.1016/j.apmr.2009.08.146
Hicks GE, Fritz JM, Delitto A, Mishock J (2003) Interrater reliability of clinical examination measures for identification of lumbar segmental instability. Arch Phys Med Rehabil 84:1858–1864
Kiesel KB, Uhl TL, Underwood FB, Rodd DW, Nitz AJ (2007) Measurement of lumbar multifidus muscle contraction with rehabilitative ultrasound imaging. Man Ther 12:161–166. doi:10.1016/j.math.2006.06.011
Koppenhaver SL, Parent EC, Teyhen DS, Hebert JJ, Fritz JM (2009) The effect of averaging multiple trials on measurement error during ultrasound imaging of transversus abdominis and lumbar multifidus muscles in individuals with low back pain. J Orthop Sports Phys Ther 39:604–611. doi:10.2519/jospt.2009.3088
Koppenhaver SL, Hebert JJ, Fritz JM, Parent EC, Teyhen DS, Magel JS (2009) Reliability of rehabilitative ultrasound imaging of the transversus abdominis and lumbar multifidus muscles. Arch Phys Med Rehabil 90:87–94. doi:10.1016/j.apmr.2008.06.022
Hebert JJ, Koppenhaver SL, Parent EC, Fritz JM (2009) A Systematic review of the reliability of rehabilitative ultrasound imaging for the quantitative assessment of the abdominal and lumbar trunk muscles. Spine 34:E848–E856
Koppenhaver SL, Hebert JJ, Parent EC, Fritz JM (2009) Rehabilitative ultrasound imaging is a valid measure of trunk muscle size and activation during most isometric sub-maximal contractions: a systematic review. Aust J Physiother 55:153–169
Ostelo RWJG, Deyo RA, Stratford P, Waddell G, Croft P, Von Korff M, Bouter LM, De Vet HCW (2008) Interpreting change scores for pain and functional status in low back pain: towards international consensus regarding minimal important change. Spine 33:90–94
Fritz JM, Irrgang JJ (2001) A comparison of a modified Oswestry Disability Questionnaire and the Quebec Back Pain Disability Scale. Phys Ther 81:776–788
Jensen MP, Turner JA, Romano JM, Fisher LD (1999) Comparative reliability and validity of chronic pain intensity measures. Pain 83:157–162
Fritz JM, Lindsay W, Matheson JW, Brennan GP, Hunter SJ, Moffit SD, Swalberg A, Rodriquez B (2007) Is there a subgroup of patients with low back pain likely to benefit from mechanical traction? Results of a randomized clinical trial and subgrouping analysis. Spine 32:E793–E800. doi:10.1097/BRS.0b013e31815d001a
Werneke M, Hart DL (2001) Centralization phenomenon as a prognostic factor for chronic low back pain and disability. Spine 26:758–765
Werneke MW, Deutscher D, Hart DL, Stratford P, Ladin J, Weinberg J, Herbowy S, Resnik L (2014) McKenzie lumbar classification: inter-rater agreement by physical therapists with different levels of formal McKenzie postgraduate training. Spine (Phila Pa 1976) 39:E182–E190. doi:10.1097/BRS.0000000000000117
Junge A, Frohlich M, Ahrens S, Hasenbring M, Sandler A, Grob D, Dvorak J (1996) Predictors of bad and good outcome of lumbar spine surgery. A prospective clinical study with 2 years’ follow up. Spine (Phila Pa 1976) 21:1056–1064 (discussion 1064–1055)
Kohlboeck G, Greimel KV, Piotrowski WP, Leibetseder M, Krombholz-Reindl M, Neuhofer R, Schmid A, Klinger R (2004) Prognosis of multifactorial outcome in lumbar discectomy: a prospective longitudinal study investigating patients with disc prolapse. Clin J Pain 20:455–461
Abramovitz JN, Neff SR (1991) Lumbar disc surgery: results of the Prospective Lumbar Discectomy Study of the Joint Section on Disorders of the Spine and Peripheral Nerves of the American Association of Neurological Surgeons and the Congress of Neurological Surgeons. Neurosurgery 29:301–307 (discussion 307–308)
Pearson A, Lurie J, Tosteson T, Zhao W, Abdu W, Mirza S, Weinstein J (2012) Who should have surgery for an intervertebral disc herniation? Comparative effectiveness evidence from the spine patient outcomes research trial. Spine (Phila Pa 1976) 37:140–149. doi:10.1097/BRS.0b013e3182276b2b
Woertgen C, Rothoerl RD, Breme K, Altmeppen J, Holzschuh M, Brawanski A (1999) Variability of outcome after lumbar disc surgery. Spine (Phila Pa 1976) 24:807–811
Hakkinen A, Ylinen J, Kautiainen H, Airaksinen O, Herno A, Kiviranta I (2003) Does the outcome 2 months after lumbar disc surgery predict the outcome 12 months later? Disabil Rehabil 25:968–972. doi:10.1080/0963828031000122258
Copay AG, Martin MM, Subach BR, Carreon LY, Glassman SD, Schuler TC, Berven S (2010) Assessment of spine surgery outcomes: inconsistency of change amongst outcome measurements. Spine J. doi:10.1016/j.spinee.2009.12.027
Acknowledgments
We wish to thank Dr. Faris Al-Odaibi and Dr. Nathan Savage for their valuable assistance with data collection. This study received funding from the Orthopaedic Section of the American Physical Therapy Association. The funding source had no role in the planning, conduct, or reporting of this study.
Conflict of interest
The authors declare no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hebert, J.J., Fritz, J.M., Koppenhaver, S.L. et al. Predictors of clinical outcome following lumbar disc surgery: the value of historical, physical examination, and muscle function variables. Eur Spine J 25, 310–317 (2016). https://doi.org/10.1007/s00586-015-3916-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-015-3916-z