Abstract
Purpose
Image-based navigational patient-specific templates (PSTs) for pedicle screw (PS) placement have been described. With recent advances in three-dimensional computer-aided designs and additive manufacturing technology, various PST designs have been reported, although the template designs were not optimized. We have developed a novel PST design that reduces the contact area without sacrificing stability. It avoids susceptibility to intervening soft tissue, template geometric inaccuracy, and difficulty during template fitting.
Methods
Fourteen candidate locations on the posterior aspect of the vertebra were evaluated. Among them, locations that had high reproducibility on computed tomography (CT) images and facilitated accurate PS placement were selected for the final PST design. An additive manufacturing machine (EOSINT M270) fabricated the PSTs using commercially pure titanium powder. For the clinical study, 36 scoliosis patients and 4 patients with ossification of the posterior longitudinal ligament (OPLL) were treated with thoracic PSs using our newly developed PSTs. We intraoperatively and postoperatively evaluated the accuracy of the PS hole created by the PST.
Results
Based on the segmentation reproducibility and stability analyses, we selected seven small, round contact points for our PST: bilateral superior and inferior points on the transverse process base, bilateral inferior points on the laminar, and a superior point on the spinous process. Clinically, the success rates of PS placement using this PST design were 98.6 % (414/420) for scoliosis patients and 100 % (46/46) for OPLL patients.
Conclusion
This study provides a useful design concept for the development and introduction of patient-specific navigational templates for placing PSs.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The accuracy of pedicle screw (PS) placement is essential for successful spinal reconstructive surgery. Authors of several previous studies have described the use of patient-specific image-based navigational templates (PSTs) for PS placement [1–12]. These templates were designed based on bone morphology reconstructed by preoperative computed tomographic (CT) images and were expected to fit into a unique position on the individual’s bone. They possess holes to guide the drill or the pedicle probe to make holes for pedicle screw placement according to the preplanned orientation. The ability to customize the placement of each screw based on the unique shape of each vertebra is an attractive concept.
The concept of the PST is not new. It was originally reported during the 1990s by Radermacher et al. [9]. They reported PSTs made of polycarbonate using milling machines for lumbar spine, hip, and knee surgery [8, 9]. Clinical application of PST, however, came into more popular use only recently after advances in computer technology and manufacturing methods. Additive manufacturing techniques—such as selective laser sintering, melting, and stereolithography—are appropriate for PST because of their ability to reproduce complex designs [3–7, 10, 11].
Although promising results have been reported [3, 5, 6, 10], PST still has some sources of potential error that preclude proper fit of the template on the bone. One of them is soft tissue intervention between the template and bone. This problem must be addressed by meticulous preparation for fitting the template on the surface of the bone. Another potential source of error is an inaccurately fabricated template that may be caused by inaccurate recognition of the bony construct on the CT image because of its low image quality or by a manufacturing error when fabricating the template. Accurate recognition of the bony construct may be difficult when the bone density is low, metallic implants are present causing artifacts, or the reproducibility of the targeted landmark is poor.
With the exception of manufacturing errors, a refined design of the template may be able to prevent those problems from arising. A template with reduced contact surface can avoid excessive soft tissue dissection. We could address problems associated with poor image quality by ensuring that only a reliable bony surface with high reproducibility on CT images is selected as the contact area. However, these approaches involve the risk of the template losing stability on the bone. Consequently, the location and size of the contact surface of the template is open to discussion. The current study was conducted to optimize the navigational template design and establish a design concept that ensures safe, accurate thoracic PS placement.
Materials and methods
Analyses for creating the template design
Candidate locations of the contact points for the template
Fourteen candidate locations of the contact points on the posterior aspect of the vertebra were selected. They were bilateral sites at the top of the transverse process (TPT), bilateral sites on the superior base of the transverse process (TBS), bilateral sites on the inferior base of the transverse process (TBI), bilateral sites on the superior part of the lamina (LS), bilateral sites on the inferior part of the lamina (LI), bilateral sites on the medial part of the lamina (LM), a site at the top of the spinous process (SPS), and a site on the spinous process superior (SPS). Each candidate round contact point (6 mm diameter) was placed on each candidate location, and its segmentation reproducibility on the CT image was evaluated (Fig. 1a).
Selection of contact points for a patient-specific template (PST). a Initial candidate contact locations on the posterior aspect of the thoracic vertebra. b After segmentation reproducibility analysis, TPTs and SPT were excluded from the contact points. We then excluded the LS and LM contact points (red) because they were inside the polygonal area (outlined by the green line) surrounded by other contact points and were thought to contribute little to stability. TPT top of the transverse process, TBS base of the transverse process superior, TBI base of the transverse process inferior, LS superior part of the lamina, LI inferior part of the lamina, LM medial part of the lamina, SPS spinous process superior, SPT top of the spinous process
Reproducibility analysis of bony segmentation
As the first step, we analyzed CT image reproducibility for the process of segmentation between bone and soft tissue. For this purpose, thin-section CT scans (1-mm slice thickness, 0.21–0.27 mm in-plane resolution) were obtained from four female spinal surgery patients including two with adolescent idiopathic scoliosis (AIS), one with thoracic ossification of the posterior longitudinal ligament (OPLL), and one with degenerative scoliosis. The CT image data were then transferred to image-processing software (VGStudio MAX 2.2; Volume Graphics, Heidelberg, Germany) and were used to reconstruct a three-dimensional (3D) model of the bony structures. This software facilitates segmentation at each CT value (in Hounsfield units, HU), 3D volume reconstruction, and 3D structural wall thickness analysis.
For the preliminary analysis for segmentation, the optimal threshold value was always 100–350 HU. Thus, we defined the segmented surface at threshold values of 100 and 350 HU (recorded as 100-HU surface and 350-HU surface, respectively). Visually, an ideal bony segmentation surface (Ideal surface) always existed between the 100-HU surface and the 350-HU surface in all four patients (Fig. 2a–c). Therefore, when the 3D bone model is reconstructed by the segmentation process at a threshold value of 100–350 HU, the geometric error of the 3D bone model is less than the distance between the 350-HU surface and the 100-HU surface. Based on this theory, the distance between the 100-HU surface and 350-HU surface was measured using the wall thickness analysis function of VGStudio MAX 2.2. The two-dimensional and three-dimensional views were colored with respect to each distance (Fig. 2d, e). To search locations with high segmentation reproducibility, we calculated the distance of each candidate point on all thoracic vertebrae of each patient, which were expressed as the mean ± standard deviation. The data were analyzed by one-way analysis of variance followed by the Tukey–Kramer multiple-comparison post hoc tests. A value of p < 0.05 was considered to indicate significance (JMP8; SAS Institute, Cary, NC, USA).
Segmentation reproducibility analysis. 100-HU surface is the segmentation surface at a threshold value of 100 HU (blue lines in a, c). 350-HU surface is that at a threshold value of 350 HU (green lines in b, c). An ideal surface is a visually ideal segmentation surface (yellow line in c). Ideal surface always exists inside the 100-HU surface and outside the 350-HU surface (c). In a two-dimensional view (d) and a three-dimensional view (e) of wall thickness analysis, each location where the distance between 100-HU surface and 350-HU surface is more than 1.5 mm is shown in red. The red locations, such as the transverse processes and spinous processes, are at high risk for low segmentation reproducibility (e)
Reducing contacting points while securing PST stability
As a result of the segmentation analysis, several candidate points were excluded because of low segmentation reproducibility. To reduce the number of contacting points as much as possible, we excluded the candidate points that contributed less than others to the stability of the template (Fig. 1b). At the end of this process, we had identified the seven most advantageous contact points for the PST.
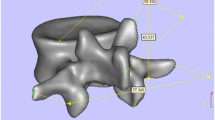
Designing the PST
The CT data were transferred to image-processing software (VG Studio) and were used to reconstruct a 3D model of the bone shape and define PS trajectories in the multiplanar reconstruction view. We identified an axial plane for each vertebra that had the most robust view of the both pedicles. On this axial plane, PS trajectories were defined and reconstructed into 3D images (Fig. 3a). Next, we reconstructed the 3D vertebral shape via a segmentation process for which the optimal threshold value was selected by visual inspection. The 3D data of the bony shape and PS trajectories were then converted into a stereolithography (STL) format file and transferred to 3D computer-assisted design (3D-CAD) software (FreeForm; SensAble Technologies, Woburn, MA, USA) to obtain the template design (Fig. 3b).
Design methods, fabricated PSTs, and special instruments for surgery. a Pedicle screw (PS) trajectories were defined on the axial plane of each vertebra. b Three-dimensional data of the bone shape and PS trajectories were transferred to the three-dimensional computer-assisted design software. c Straight tubes with a hole to guide the drill or the pedicle probe were defined according to the direction of the PS trajectories. Seven contact points were also defined on the posterior aspect of the referred vertebra. Note that the contact point on the spinous process is small so as to reduce the risk of morphological error. d Two guide tubes and contact points were then connected with curved supports. Each guide was numbered according to its level to avoid wrong-site use. e Fabricated PSTs and the bone model. PSTs were made of titanium metal, and the bony model was made of gypsum. In this case, PSTs were fabricated for the vertebrae from T1 to L3. Each rib end is connected by supports in the bone model. f–h Photographs of a specially designed cylindrical chisel (f, h) and pedicle probe (g, i)
Each PST had two straight tubes with a tunnel parallel to the tube that guided a pedicle probe or a drill. The direction of the tunnel was determined based on the CT image of the targeted pedicle so the PS could gain purchase in the bone efficiently without perforation. The seven small, round contact points (4 mm diameter for SPS and 6 mm diameter for the others) were also determined on the posterior aspect of the referred vertebra. The two guide tubes and seven contact points were then connected with curved supports (Fig. 3c, d). Each PST was numbered according to its level to avoid wrong-site use (Fig. 3d, e). Finally, the STL format files of the PST were transferred to the selective laser-melting (SLM) machine (EOSINT M270; Electro Optical Systems GmbH, Krailling, Germany). Nominal dimensional accuracy of this additive manufacturing machine is under 200 µm.
Fabrication of the PST and bony models
PSTs were fabricated by an SLM method (EOSINT M270) using commercially pure titanium powder [13]. After the slice data were obtained from the STL data, titanium powder (grade 2, particle size <45 µm; Osaka Titanium Technologies, Amagasaki, Japan) was melted using an ytterbium fiber laser beam in an argon gas atmosphere. A selected slice of the product was then solidified. The top of the previously melted surface was recoated with a layer of titanium powder (thickness 45 µm). Subsequently, selective irradiation was again carried out using the laser beam. These steps were repeated until the final geometry was achieved. Bony models were then made using a gypsum-based 3D printer (ZPrinter 450; Z Corporation, Burlington, MA, USA).
We confirmed that each titanium template on the plaster model was designed with adequate adaptation, stability, and proper PS guide hole direction (Fig. 3e). Each template was sterilized in an autoclave and then used for making PS holes during surgery.
Clinical evaluation of the accuracy of PS placement
The clinical study was performed based on the principles of the Declaration of Helsinki and good clinical practice. The study was registered on the University Hospital Medical Information Network Clinical Trials Registry (UMIN000004618). In accordance with protocols approved by the Institutional Ethics Committee, written informed consent was obtained from all patients. When the patient was younger than 20 years old, written informed consent was obtained from the patient’s parents.
The 40 patients who were treated with thoracic PSs using our newly developed PST between July 2010 and August 2013 were included in this study. Revision cases were excluded. There were 36 patients with scoliosis (Lenke type 1, 19 cases; type 2, 6 cases; type 3, 7 cases; type 4, 1 case; type 5, 1 case, type 6, 2 cases) and four patients with OPLL. Except for two patients with Marfan syndrome, the etiology of the scoliosis patients was idiopathic.
The scoliosis group included 6 male and 30 female patients with a mean age of 15.0 ± 1.9 years (range 11–19 years) at the time of surgery. The mean Cobb angle of the main curve was 66.6° ± 13.5° (range 43–110°). All four OPLL patients were women with a mean age of 55.3 ± 16.5 years (range 43–77 years) at the time of surgery.
During the surgery, the spinous process, lateral margin of the transverse process, and lamina were exposed, and the paravertebral muscle was retracted laterally. The template was then press fitted to the surface of the lamina and held by the surgical assistant. The entry hole was made using a specially designed cylindrical chisel (Fig. 3f, h). A straight pedicle probe (diameter 3 mm) was then used to make the screw hole (Fig. 3g, i).
The accuracy of the PS hole created using the PST was evaluated intraoperatively and postoperatively. The intraoperative evaluation was performed using the commonly applied image guidance techniques (e.g., CT-based navigation or intraoperative fluoroscopy) and manual palpation with a small ball-tip probe. When the pedicle wall perforation was recognized using these methods, the PS hole was recorded as a “failure.” When a PS hole was regarded as a failure intraoperatively, we had two surgical options for this pedicle, according to the surgeon’s preference. One was to create another screw hole using a common method, thereby continuing screw placement. The other was to cancel the screw placement. Postoperatively, CT scans at the PS insertion levels were obtained from all patients. The slices were accessed regarding the presence of PS perforation. When a perforation was found, it was evaluated according to Neo’s classification [14] (grade 0: no perforation; grade 1: perforation <2 mm; grade 2: perforation ≥2 mm but <4 mm; grade 3: perforation ≥4 mm).
Results
Reproducibility analysis of bony segmentation
The results of the reproducibility analysis are shown in Fig. 4. When the threshold value of the segmentation was changed from 100 to 350 HU, the morphologic changes amounted to about 2 mm at the top of transverse process (TPT) and less than 1 mm at the base of the transverse process (TBS, TBI) and the lamina (LS, LI, LM) in all four cases. These results indicate that TPT is not suitable as a contact point. There was a tendency to have greater morphologic changes in the spinous process (SPS, SPT) than in the other candidate locations, except TPT. There was less morphologic change in the superior part (SPS) of the spinous process than in the top part (SPT). Considering these limitations, we adopted the SPS as a smaller contact point.
Results of segmentation reproducibility analysis. Error bar means standard deviation. In all patients, TPT had statistically higher values than those at other locations (asterisk). SPT in two patients with adolescent idiopathic scoliosis (AIS1 and AIS2) and a posterior longitudinal ligament (OPLL) showed statistically higher values than those at other locations except TPT (double asterisk). SPS in AIS2 showed a statistically larger value than those at other locations except TPT and SPT (triple asterisk). SPT in patients with degenerative lumbar scoliosis (DLS) showed statistically higher values than those at other locations except TPT and SPS (four asterisks). See Fig. 1 for definitions of other abbreviations
Reducing the number of contact points while securing PST stability
As shown in Fig. 2, LS and LM were deleted from the original contact points because they were inside the polygonal area surrounded by other contact points and thus considered to contribute little to stability of the PST. We finally selected only seven contact points (bilateral TBSs, bilateral TBIs, bilateral LIs, SPS) for the final PST design, as shown in Fig. 3.
Clinical study
During surgery, positioning the PST manually was easy, with a proper fit for the PSs. We were able to place the PSs with confidence. No intraoperative vascular or neurologic injuries occurred during PS placement. There were also no postoperative complications (e.g., infection).
A total of 420 PS holes were created using PST in 36 scoliosis patients. Among them, five pedicle wall perforations were recognized intraoperatively and were recorded as “failures.” In all, 415 PSs were placed in the scoliosis patients using PST. The PS placements were classified postoperatively as grade 0 in 408 (98.4 %), grade 1 in 6 (1.4 %), and grade 2 in 1 (0.2 %). There were no grade 3 PS placements. No failures were recognized intraoperatively for the 46 PS holes created in the four OPLL patients, and all of the 46 PS placements were classified as grade 0 postoperatively (Fig. 5).
As a result, 414 PSs for 36 scoliosis patients were placed successfully (i.e., grade 0 or grade 1 in the postoperative CT evaluation) in the 420 holes created using PST. Also, all PSs were placed successfully in the 46 holes created for four OPLL patients (success rates were 98.6 and 100 %, respectively).
Discussion
We developed a new PST design concept for pedicle screw placement. The point of our concept is that this PST has reduced the contact area on the bone without sacrificing stability of the template. With the recent advances in 3D image acquisition, 3D-CAD, and additive manufacturing technology, PSTs of various designs have been reported [1–11]. The template designs, however, were not fully optimized and many had a large contact area on the bone surface [2, 3, 5–10]. Template designs with a large contact area appear to increase the template’s stability on the bone, although it might be more arduous to fit it completely to the local anatomy. It is also susceptible to intervening soft tissue and geometric inaccuracy. In addition, templates with a larger contact area are sometimes more difficult to handle during the fitting step. Hence, in this study, we decided to use only certain reliable points that have high reproducibility on CT images and facilitate accurate PS placement.
During segmentation, the morphologic reproducibility of the spinous process (SPS and SPT) and TPT was inferior. Furthermore, a PST with a contact point on the TPT would be too large for easy handling during surgery. Therefore, we deleted the TPT from the contact points. The spinous process was employed as a contact point because of its large contribution to the stability of the PST, easy exposure of the anatomy, and relatively high morphologic reproducibility of its superior part (SPS). We took care to place a contact point on the SPS and placed a smaller one (4 mm diameter compared with 6 mm for the others) on the point where the segmentation was carried out correctly.
PSTs with a small contacting area have also been reported [1, 4, 11]. Although these reports were on mainly preliminary studies, their PSTs also have the potential to reduce the problems of intervening soft tissue and poor image quality. Goffin et al. [11] developed a PST with knife-edge support for posterior transarticular fixation (Magerl screw) and reported a small clinical case series of two patients. Berry et al. [1] reported a cadaver study of their PST with small contact points or knife-edge support. However, the failure rate of their PST for thoracic PS was reported to be up to 44 %. The reason of their low accuracy was mainly poor stability. They proposed to improve the design by additional supports. However, few screws were used in the improved design (two screws for thoracic surgery and four screws for cervical surgery) [1]. In this study, we created 466 screw holes in clinical patients using our PST, with successful pedicle screw placement rates for scoliosis and OPLL patients at 98.6 % (414/420) and 100 % (46/46), respectively. These rates are extremely high in comparison with those for other techniques, such as free-hand technique (85 %) or even a navigated technique (94 %) [15], validating the superiority of our PST.
The materials to be used also merit discussion. In contrast to our titanium PST, all previously reported PSTs were constructed of nonmetallic materials [2–10]. These materials are generally additive-manufacturing material approved by the United States Pharmacopeia (USP) for use in the human body for 24 h (USP level VI). Examples are polyamide (Duraform® polyamide) [1] and acrylate resin (Stereocol®) [8]. When we consider the possible residual material that accumulates during drilling or probing, however, titanium metal, which is approved for permanent implantation, may be safer than USP level VI materials. Additionally, titanium metal is stiffer and more stable than the above-mentioned materials, thereby facilitating PS insertion in the intended direction. Thus, titanium metal seems to be one of the best materials for PST, although other low-cost materials, such as stainless steel and nonmetallic USP level VI materials are less expensive than titanium metal. The cost for 10 PSTs for 20 pedicles in one patient is $1000 USD when they are made of titanium metal versus $200 USD when made of polyamide. These low-cost materials will be ready for use in our PST in the near future.
Our PST has a wide range of applications. Not only can the designed PST be used for thoracic PSs, as in this study, a variation of it can be used for lumbar (Fig. 3e) and cervical PSs by simply selecting the optimal contact points. This technique would be most suited for patients with complicated anatomy, such as atlanto-axial fixation or congenital scoliosis. We can also apply this technology to various orthopedic procedures. For example, for hip surgery, we have developed a guide for curved periacetabular osteotomy by selecting contact points for this limited surgical field [16]. In addition, we believe that our method has the potential to overcome low-quality CT images in patients with osteoporosis or in those undergoing revision surgery with previous metallic implantation by carefully selecting adequate contact points at the locations where image quality is relatively reliable. We did not have such cases in the present study, so clinical validation is necessary.
One of the limitations of this technology is that it requires extra time, labor, and cost for preparation. It takes about 2–3 h to design 10–15 PSTs for a single scoliosis patient, 1 day for manufacturing, and 1 day for cleaning and sterilizing the manufactured PSTs. In the future, advances in computer technology and manufacturing methods are expected to reduce the preparatory time, labor, and cost. In addition, because the use of CT is mandatory for this technique, its application should be carefully evaluated in terms of invasiveness, as well as cost-effectiveness.
In conclusion, for the PST for thoracic PSs, seven small, round contact points were selected on each lamina. The points were chosen to reduce the contact area without sacrificing accuracy and provide a high success rate for placing PSs without perforation (98.6 % success rate in scoliosis patients and 100 % in those with OPLL). Unlike conventional PSTs, a large contact surface was not necessary. This study provides a useful design concept for the development and introduction of patient-specific navigational templates for placing PSs and for other orthopedic surgery.
References
Berry E, Cuppone M, Porada S, Millner PA, Rao A, Chiverton N, Seedhom BB (2005) Personalised image-based templates for intra-operative guidance. Proc Inst Mech Eng [H] 219:111–118. doi:10.1243/095441105X9273
Ma T, Xu YQ, Cheng YB, Jiang MY, Xu XM, Xie L, Lu S (2012) A novel computer-assisted drill guide template for thoracic pedicle screw placement: a cadaveric study. Arch Orthop Trauma Surg 132:65–72. doi:10.1007/s00402-011-1383-5
Kawaguchi Y, Nakano M, Yasuda T, Seki S, Hori T, Kimura T (2012) Development of a new technique for pedicle screw and Magerl screw insertion using a 3-dimensional image guide. Spine 37:1983–1988. doi:10.1097/BRS.0b013e31825ab547
Yang JC, Ma XY, Lin J, Wu ZH, Zhang K, Yin QS (2010) Personalised modified osteotomy using computer-aided design-rapid prototyping to correct thoracic deformities. Int Orthop. doi:10.1007/s00264-010-1155-9
Lu S, Xu YQ, Zhang YZ, Li YB, Xie L, Shi JH, Guo H, Chen GP, Chen YB (2009) A novel computer-assisted drill guide template for lumbar pedicle screw placement: a cadaveric and clinical study. Int J Med Robot 5:184–191. doi:10.1002/rcs.249
Ryken TC, Owen BD, Christensen GE, Reinhardt JM (2009) Image-based drill templates for cervical pedicle screw placement. J Neurosurg Spine 10:21–26. doi:10.3171/2008.9.SPI08229
Lu S, Xu YQ, Lu WW, Ni GX, Li YB, Shi JH, Li DP, Chen GP, Chen YB et al (2009) A novel patient-specific navigational template for cervical pedicle screw placement. Spine 34:E959–E966. doi:10.1097/BRS.0b013e3181c09985
Birnbaum K, Schkommodau E, Decker N, Prescher A, Klapper U, Radermacher K (2001) Computer-assisted orthopedic surgery with individual templates and comparison to conventional operation method. Spine (Phila Pa 1976) 26:365–370
Radermacher K, Portheine F, Anton M, Zimolong A, Kaspers G, Rau G, Staudte HW (1998) Computer assisted orthopaedic surgery with image based individual templates. Clin Orthop Relat Res 354:28–38
Sugawara T, Higashiyama N, Kaneyama S, Takabatake M, Watanabe N, Uchida F, Sumi M, Mizoi K (2013) Multistep pedicle screw insertion procedure with patient-specific lamina fit-and-lock templates for the thoracic spine: clinical article. J Neurosurg Spine 19:185–190. doi:10.3171/2013.4.SPINE121059
Goffin J, Van Brussel K, Martens K, Vander Sloten J, Van Audekercke R, Smet MH (2001) Three-dimensional computed tomography-based, personalized drill guide for posterior cervical stabilization at C1-C2. Spine (Phila Pa 1976) 26:1343–1347
Lu S, Xu YQ, Zhang YZ, Xie L, Guo H, Li DP (2009) A novel computer-assisted drill guide template for placement of C2 laminar screws. Eur Spine J 18:1379–1385. doi:10.1007/s00586-009-1051-4
Pattanayak DK, Fukuda A, Matsushita T, Takemoto M, Fujibayashi S, Sasaki K, Nishida N, Nakamura T, Kokubo T (2011) Bioactive Ti metal analogous to human cancellous bone: fabrication by selective laser melting and chemical treatments. Acta Biomater 7:1398–1406. doi:10.1016/j.actbio.2010.09.034
Neo M, Sakamoto T, Fujibayashi S, Nakamura T (2005) The clinical risk of vertebral artery injury from cervical pedicle screws inserted in degenerative vertebrae. Spine 30:2800–2805
Shin BJ, James AR, Njoku IU, Härtl R (2012) Pedicle screw navigation: a systematic review and meta-analysis of perforation risk for computer-navigated versus freehand insertion. J Neurosurg Spine 17:113–122. doi:10.3171/2012.5.SPINE11399
Otsuki B, Takemoto M, Kawanabe K, Awa Y, Akiyama H, Fujibayashi S, Nakamura T, Matsuda S (2013) Developing a novel custom cutting guide for curved peri-acetabular osteotomy. Int Orthop. doi:10.1007/s00264-013-1873-x
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Takemoto, M., Fujibayashi, S., Ota, E. et al. Additive-manufactured patient-specific titanium templates for thoracic pedicle screw placement: novel design with reduced contact area. Eur Spine J 25, 1698–1705 (2016). https://doi.org/10.1007/s00586-015-3908-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-015-3908-z