Abstract
Purpose
Lumbar epidural injection is a popular treatment for degenerative lumbar disease. Although post-procedural epidural infection is rare, meningitis and epidural abscess are life-threatening conditions, and need additional medical and surgical intervention. The purpose of this article is to report a patient with fatal whole cerebrospinal axis infection after lumbar epidural injections.
Methods
A 64-year-old female patient presented with septic shock and quadriparesis. In the past, this patient had received lumbar epidural injections several times for degenerative spondylolisthesis at L4-5 in another hospital. The magnetic resonance imaging showed epidural abscess, a compressed dura and spinal cord from C1 to S2, and cerebral meningitis. We performed laminectomies and removal of the abscesses. Her mental status was diminished to a deep, drowsy state after three postoperative weeks. Brain computed tomography scans revealed hydrocephalus. Therefore, ventriculoperitoneal shunting was performed.
Results
Methicillin resistant Staphylococcus epidermidis was cultured from blood samples. The patient’s infection was completely controlled and her mental status improved to alert; however, her quadriparesis remained.
Conclusions
Although lumbar epidural injection is an effective procedure to treat lumbar radicular pain, this procedure can induce fatal complications such as sepsis and epidural abscess.
Level of evidence
5.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Spinal pain block procedures such as interlaminar or transforaminal epidural injections are common and popular treatments for spinal radicular pain [1–3]. In degenerative lumbar disease, lumbar epidural steroids and local anesthesia injections can improve patients’ symptoms significantly without surgical intervention [1, 3]. However, there are complications associated with pain block procedures. Although the majority of complications are minor morbidities, post-procedural infections such as meningitis, epidural abscess, spondylitis, and discitis may need additional surgical intervention and long-term use of antibiotics [2]. Moreover, infection can induce motor weakness and fatal morbidities. We have treated and observed patients with fatal whole cerebrospinal axis infection that developed after lumbar epidural injection.
Case report
A 64-year-old female patient in the department of infection was referred to our department of neurosurgery for weakness in both legs (G2 of 5). Over the past 11 months, in a different regional hospital, the patient had received lumbar epidural injections once a month for a diagnosis of degenerative spondylolisthesis at L4-5. Her most recent epidural injection was approximately 3 weeks previously. With the exception of hypertension, the patient’s medical history was unremarkable. Six days prior to admission to our department, the patient was admitted to the infectious disease department due to a fever of unknown origin (39.1 °C) that started 1 day prior. Initial laboratory tests indicated that the erythrocyte sedimentation rate (ESR) was 68 mm/h (normal range: 1–20 mm/h), and the C-reactive protein (CRP) level was 26.34 mg/dL (normal range: 0–0.3 mg/dL). White blood cell (WBC) and neutrophil counts were 13,290/mcL (normal range: 3,700–9,700/mcL) and 11,828/mcL (normal range: 1,800–7,700/mcL), respectively. The patient had been receiving daily intravenous ceftriaxone 2 g, metronidazole 500 mg, and amikacin 500 mg since initial admission time. Although she was administered empirical intravenous antibiotics and intravenous fluids, her fever remained uncontrolled, hypotension developed (blood pressure systolic/diastolic, 89/56 mmHg), and the strength of both legs was decreased to grade 2/5. There were several ecchymoses on both thighs. The deep tendon reflexes in both knees and ankles were diminished. Hyperesthesia was present below the T9 dermatome and anal sphincter tone and sensation were decreased. A thoracolumbar magnetic resonance imaging (MRI) was taken immediately after development of bilateral lower extremity weakness. Thoracolumbar MRI showed epidural abscesses and a compressed dura and spinal cord from T9 to S2 (Fig. 1a). In addition, a muscular abscess was detected in the lumbar multifidus area (Fig. 1b).
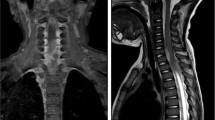
Intermittent laminectomies and removal of abscesses were performed from T9 to S1. However, the bilateral lower extremity weakness did not improve. Furthermore, the strength of both upper extremities decreased to a grade 3/5 at 2 hours postoperative. A cervical MRI was taken immediately after the development of upper extremity weakness and showed a ventral epidural abscess in the cervicothoracic area. The ventral epidural abscess seriously compressed the spinal cord at C1-2 area. In addition, there was cerebral meningeal enhancement, which suggested cerebral infectious meningitis (Fig. 2). We performed C1-2 hemi-laminectomies and removal of the abscess immediately after interpreting the cervical MRI. Her mental status was diminished to a deep drowsy state after three postoperative weeks. Brain computed tomography (CT) scan images revealed hydrocephalus (Fig. 3a). Ventriculoperitoneal shunting was performed (Fig. 3b) 2 weeks after extra-ventricular drainage of cerebrospinal fluid (CSF). WBC and red blood cell (RBC) counts of initial CSF were 5 and 100/μL, respectively. The CSF protein content was increased at 124 mg/dL (normal range; 15–50 mg/dL), and the CSF glucose content was within normal limits at 90 mg/dL (normal range: 40–100 mg/dL). Methicillin resistant Staphylococcus epidermidis (MRSE) was detected, not in the CSF and epidural abscess, but in initial blood culture at admission. She was treated with intravenous vancomycin for 8 weeks until CRP level was normalized. Finally, the infection was completely controlled and her mental status improved to alert. The patient’s quadriparesis improved to arm grade 4/5 and leg grade 3/5.
Discussion
Transforaminal or interlaminar epidural spinal injections have been performed to treat pain in patients with lumbar degenerative disease [2, 3]. Since anesthesiologists, radiologists, physiatrists, and spine surgeons all perform these procedures, the number of pain block procedures performed is high [2]. However, there is the possibility of complications such as epidural hematoma, nerve injury, infection, CSF leakage, fistula due to dura puncture, and embolism [1, 4]. These epidural procedure-related complications can induce morbility and mortality [2]. Among these complications, infections develop in 0.01–2 % of patients. Discitis, epidural abscess, spondylitis, and meningitis can occur after epidural injections [4]. If spinal epidural abscesses are not controlled by the administration of antibiotics, and induce neurological compromise, additional surgical interventions should be considered. Surgical removal of spinal epidural abscesses can decompress neural structures and reveal infectious microorganisms. On the other hand, CT-guided biopsy with abscess drainage is a less invasive technique that may be considered in less severe cases without symptoms of neurologic compromise [5].
Pathogenic microorganisms are detected and cultured in epidural pus, CSF, and blood [6]. Blood culture is a highly sensitive and cost-effective investigation for detecting pathogenic microorganisms. However, nearly 40 % of epidural abscess cultures are negative even without prior antibiotic therapy [5, 7]. Therefore, blood cultures should be performed in patients with spinal epidural abscesses [5]. In this case, MRSE was detected, not in epidural pus, but in initial blood cultures from admission. Since empirical antibiotic administration may interfere with results of culture studies, we recommend that initial blood culture should be taken before antibiotic treatment, if infection is suspected. Most pathogenic microorganisms in intervention-related infections are Gram-positive cocci such as Staphylococcus aureus and Staphylococcus epidermidis, as seen in this patient [2, 4]. Therefore, empirical antibiotic therapy must include antibiotics against Gram-positive cocci, such as vancomycin. However, infection from Gram-negative anaerobes must also be considered [5]. For this reason, we prefer combination empirical antibiotic therapy for patients with spinal infections.
MRIs are the cornerstone of the diagnosis of spinal epidural abscesses. Epidural abscesses can spread to other sites from the cervical to sacral area. Furthermore, delayed diagnosis of remote skip epidural abscesses can induce fatal complications including uncontrolled infection. Although many patients have focal epidural abscesses, we recommend obtaining whole spine MRIs to avoid these severe negative outcomes.
In this patient, there were concomitant multifidus muscle abscesses. These findings suggest that epidural abscesses may result in procedurally related infections. Aseptic and atraumatic conditions are important during procedures. Further, procedure times are important for prevention of infection. Glucocorticoid injections compromise immune responses and increase the risk of infection [8]. Therefore, pain societies recommend a maximum of six injections in a year. Frequent epidural injections also contribute to the development and aggravation of infection. Finally, both epidural abscesses and meningitis were developed after epidural injections. Moreover, the epidural abscesses aggressively spread throughout the whole spine area, and the meningitis induced hydrocephalus.
Although the incidence of epidural abscess and meningitis is very low, these complications can induce life-threatening conditions such as sepsis and weakness.
Conclusion
Although lumbar epidural block is an effective procedure to treat lumbar radicular pain, there are fatal complications such as meningitis and epidural abscess associated with this procedure. Aseptic conditions, glucocorticoid use, and number of procedures should be considered.
References
Landa J, Kim Y (2012) Outcomes of interlaminar and transforaminal spinal injections. Bull NYU Hosp Jt Dis 70(1):6–10
Epstein NE (2013) The risks of epidural and transforaminal steroid injections in the Spine: commentary and a comprehensive review of the literature. Surg Neurol Int 4(Suppl 2):S74–S93
Manchikanti L, Datta S, Gupta S, Munglani R, Bryce DA, Ward SP, Benyamin RM, Sharma ML, Helm S, Fellows B, Hirsch JA (2010) A critical review of the American Pain Society clinical practice guidelines for interventional techniques: part 2. Therapeutic interventions. Pain physician 13(4):E215–E264
Goodman BS, Posecion LW, Mallempati S, Bayazitoglu M (2008) Complications and pitfalls of lumbar interlaminar and transforaminal epidural injections. Curr Rev Musculoskelet Med 1(3–4):212–222
Guerado E, Cervan AM (2012) Surgical treatment of spondylodiscitis. An update. Int Orthop 36(2):413–420
Hooten WM, Kinney MO, Huntoon MA (2004) Epidural abscess and meningitis after epidural corticosteroid injection. Mayo Clin Proc 79(5):682–686
Radcliffe R, Meites E, Briscoe J, Gupta R, Fosheim G, McAllister SK, Jensen B, Noble-Wang J, del Rosario M, Hageman J, Patel PR (2012) Severe methicillin-susceptible Staphylococcus aureus infections associated with epidural injections at an outpatient pain clinic. Am J Infect Control 40(2):144–149
Manchikanti L (2002) Role of neuraxial steroids in interventional pain management. Pain Physician 5(2):182–199
Conflict of interest
None of the authors has any potential conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Noh, S.H., Heo, D.H. Whole cerebrospinal axis infection after lumbar epidural injection: a case report. Eur Spine J 24 (Suppl 4), 525–528 (2015). https://doi.org/10.1007/s00586-014-3667-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-014-3667-2