Abstract
Purpose
Thoracic adolescent idiopathic scoliosis (AIS) curves (Lenke 1–4) are often characterized by hypokyphosis. Sagittal alignment remains challenging to correct, even with recent posterior segmental instrumentation. Some authors recommend anterior endoscopic release (AER) to reduce anterior column height, and facilitate thoracic kyphosis correction. The aim of this study was to assess the contribution of AER to sagittal correction in hypokyphotic AIS.
Methods
Fifty-six hypokyphotic (T4T12<20°) AIS patients were included. In group 1 (28 patients), patients first underwent AER, followed by posterior instrumentation and correction 5–7 days later. In group 2 (28 patients), patients underwent the same posterior procedure without AER. Posterior correction was performed in all cases using posteromedial translation and hybrid constructs consisting of lumbar pedicle screws and thoracic sublaminar bands. From radiological measurements performed using low-dose EOS radiographs, the correction of thoracic kyphosis was compared between the two groups.
Results
Groups 1 and 2 were comparable regarding demographic data and preoperative thoracic kyphosis (group 1: 11.7° ± 6.9° vs group 2: 12.1° ± 6.3°, p = 0.89). Postoperative thoracic kyphosis increase averaged 18.3° ± 13.6° in group 1 and 15.2° ± 9.0° in group 2. The benefit of anterior release was not statistically significant (p = 0.35).
Conclusion
Although previous studies have suggested that thoracoscopic release improved correction compared to posterior surgery alone, the current study did not confirm this finding. Moreover, results of the current series showed that no significant benefit can be expected from AER in terms of sagittal plane improvement when the posteromedial translation technique is used, even in challenging hypokyphotic patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Adolescent idiopathic scoliosis (AIS) is a progressive three-dimensional deformity, often responsible for flattening of sagittal curves. Lenke 1–4 AIS patients often present with thoracic hypokyphosis, which has been associated with pulmonary function impairment [1, 2]. The aim of surgery is to restore a physiological trunk shape through three-dimensional correction of the deformity [2–4].
Correction of AIS can be achieved using various techniques. Practically all posterior surgical techniques for treatment of Lenke 1–4 AIS include use of pedicle screws. In early reports, these pedicle screws were combined with hooks, wiring or cables in the proximal, thoracic portion of the constructs. In 1995, Suk et al. [5] proposed the use of pedicle screws throughout the posterior construct including the thoracic portion. Although all-screw constructs are still widely used, these have some limitations, such as the sagittal correction of the thoracic spine, that have been recently emphasized in Lenke 1 AIS [6, 7]. In addition, the smaller pedicle size and the vertebral dystrophy frequently observed in the concavity of the deformity increase the risk of potential pedicle screw-related complications, such as neurologic and vascular injuries or pleural tears [8]. On the other hand, some surgeons now prefer hybrid constructs with sublaminar bands not only for the low complication rate, but also because posteromedial translation mediated by periapical sublaminar bands provides better sagittal correction than all-screw instrumentation, while the coronal correction is equivalent [7, 9].
Nonetheless, in hypokyphotic AIS, correcting sagittal malalignment remains challenging. Some authors have proposed a preliminary anterior endoscopic release (AER), to reduce the anterior column height and, therefore, facilitate improvement of thoracic kyphosis [10, 11]. Originally, the indication for combining AER to posterior correction in the treatment of spinal deformity was severe or stiff curves (Cobb > 60˚, reducibility < 50 %). Subsequently, some authors proposed AER to optimize the postoperative sagittal alignment [12, 13, 16]. Recent studies have reported promising sagittal results with hybrid constructs using thoracic sublaminar bands [7, 9]. In this series, however, indications for and rate of anterior release varied. Consequently, it was difficult to assess the relative contributions of posteromedial translation and anterior release to the observed improvement of thoracic kyphosis.
The aim of the present study was to assess the influence of anterior endoscopic release on sagittal correction in hypokyphotic AIS patients treated using posteromedial translation.
Methods
Patients
Following institutional review board approval, 56 consecutive patients were included between 2008 and 2011 in this retrospective study involving two different centers. Inclusion criteria were thoracic AIS patients treated surgically and presenting a thoracic hypokyphosis, corresponding to a sagittal T4T12 Cobb angle <20° and who had reducibility of the main coronal curve below 50 % on bending films. A minimum 2-year follow-up was required. All patients were evaluated before surgery, in the early postoperative period, at 6 months and 1 year after surgery, and at last follow-up. None of the patients have had prior spinal surgery.
Radiographic measurements
All patients underwent biplanar radiographs in a standing position using the EOS system (EOS imaging, Paris, France) following a previously described acquisition protocol [14, 15]. The EOS system is used instead of conventional X-rays in these units for routine clinical workups. Patients maintained their arms folded at 45° to avoid superposition with the spine. All images included the base of the skull and the upper third of the femurs. Parameters assessed in the sagittal plane were lumbar lordosis, measured from the upper endplate of L1 to the upper endplate of S1; thoracic kyphosis (TK), measured from the upper endplate of T4 to the lower endplate of T12; and cervical lordosis, measured from the lower endplate of C2 to the lower endplate of C7 (the values were negative in cases of lordosis and positive in cases of kyphosis). Pelvic parameters included pelvic incidence (PI), pelvic tilt (PT) and sacral slope (SS) [16]. Radiographic analysis in the coronal plane included Cobb angle measurements and frontal C7 tilt.
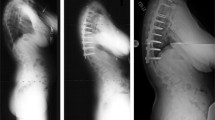
Operative procedures
Patients were divided into two groups based on the type of surgical approach. In the first institution (group 1, 28 patients), patients underwent AER followed by posterior correction 5–7 days later. In this center, the indication for thoracoscopy was a stiff main curve with reducibility below 50 % on bending films and only hypokyphotic patients were included as described above. In the second center (28 patients), patients were treated during a single posterior procedure and AER was never performed. Three experienced senior surgeons were involved: two in the first center and one in the second center. In both centers, the posterior correction technique was exactly the same, in all cases: posteromedial translation using hybrid constructs combining lumbar pedicle screws, thoracic sublaminar bands (Universal Clamps, Zimmer Spine, Bordeaux, France), and 5.5 titanium alloy rods. Fusion levels were selected following the same criteria in the two groups during the study period [17, 18]. During the posterior procedures, spinal cord function was monitored by means of somatosensory/motor-evoked potentials. AER was performed as previously described: patients were operated in the lateral position, with two endoscopic ports on the convex side of the deformity [22]. The release included the apex of the deformity as well as two discs above and two discs below the apical vertebra [19] (Fig. 1). No bone graft or instrumentation was applied during the thoracoscopy procedure. As recommended by Suk et al. [20], thoracoplasty was performed in patients with a rib hump greater than 15°.
Statistical analysis
Paired t tests were used to analyze differences between preoperative and postoperative curves within each group. All variables were normally distributed and comparisons between the two groups were performed using unpaired t tests. Statistical significance was defined as p < 0.05. Statistical analysis was performed using SPSS version 20.0 (SPSS Inc., Chicago, IL, USA).
Results
Patients’ presentation and surgical procedure
Demographic data of the two groups are summarized in Table 1. According to the AIS classification described by Lenke et al. [21], there were 29 patients with type 1 AIS (51 %), 19 with type 2 (34 %), 8 with type 3 (15 %) and none with type 4. Patients from center 1 and 2 were comparable in terms of preoperative T4–T12 kyphosis, cervical alignment (which was kyphotic) and pelvic parameters, the values of which are provided in Table 2. However, the preoperative main Cobb angle was significantly greater in group 1 (p = 0.01). The average number of instrumented levels was 12.7 (±1.1) with an average of 4.6 (±1.7) screws and 7.2 (±1.8) sublaminar bands. No difference was found between groups in terms of level fused and number of implants used for correction. The anterior release included a mean of 4.5 (±0.9) discs.
Curve correction
Results obtained in the frontal and sagittal plane are reported in Tables 3 and 4. In the sagittal plane, TK significantly increased postoperatively in both groups (p < 0.001). At last follow-up, 75 % of the patients had a TK greater than 20° in group 1 and 85 % in group 2. Comparative analysis revealed that the benefit of anterior release was not statistically significant in terms of hypokyphosis correction. The mean thoracic kyphosis gain in the thoracoscopy group was 18.3° (±13.6) compared to 15.2° (±9.1) in the group without AER (p = 0.33). Cervical lordosis was increased in both groups (change in group 1: −9.7° (±13.1), p = 0.005, change in group 2: −8.9° (±14.5), p = 0.006). In the coronal plane, the main Cobb angle corrections were significant in both groups (change in group 1: 38.6° (±14.6), p = 0.01 and change in group 2: 38.2° (±14.2), p < 0.001). The contribution of anterior release was not statistically significant in terms of main Cobb angle correction, with a mean coronal correction of 38.6° (±14.6) in group 1 and 38.3° (±14.2) in group 2 (p = 0.94) (Table 5). At last follow-up, the main curve correction was 56.4 % in group 1 and 63.4 % in group 2 without significant difference between groups (p = 0.10).
Hospital stay and complications
The mean length of hospital stay was 5 days longer in group 1, due to the treatment protocol, with an average of 5.4 ± 3.4 days between the AER and the posterior correction. No intraoperative complication related to the posterior correction was reported in either group. In particular, no significant change in the monitored somatosensory/motor-evoked potential was observed. After surgery, there was no transient or permanent dysesthesia, paresthesia or paraplegia. After 2 years, there was no loss of sagittal correction in either group and none of the patients had a severe loss of the major curve correction.
Four complications related to the thoracoscopic release were observed, including severe pneumothorax requiring evacuation in two patients and pleural effusion treated with physiotherapy in two other patients. Two infections in group 1 and one in group 2 were treated by surgical debridement (p > 0.05).
Discussion
Sagittal plane improvement
In spinal deformity surgery, recent literature has highlighted the importance of sagittal plane analysis and the potential impact of spino-pelvic alignment on pain and disability later in life [22–24].
As suggested by Winter et al. [4] and Kim et al. [3], restoring physiologic TK should reduce the risk of progressive junctional kyphosis at the extremities of the fused spine. In 2013, Clément et al. [25] found a significant correlation between thoracic kyphosis and proximal lordosis in AIS suggesting that sagittal improvement might better ensure long-term results and decrease the rate of long-term decompensation by proximal kyphosis.
Nonetheless, correcting hypokyphosis in AIS remains challenging. Some authors previously reported that pedicle screw constructs provided a better correction of the sagittal kyphosis associated with coronal deformity [26]. However, Vora et al. [7] recently concluded from a multicenter retrospective study that pedicle screw constructs tend to lordose the thoracic spine. Others have also reported the difficulty of restoring physiologic TK in AIS patients treated by selective posterior thoracic fusion with all-screw constructs [27, 28]. Moreover, Senaran et al. and Upendra et al. [29, 30] reported a 10 and 18 % rate of unacceptable pedicle screws placement, respectively. In the present study, hypokyphosis was effectively corrected in each group with a mean increase of 15° in one group and 18° in the other, similar to the best results of previous studies, and no proximal junctional kyphosis was observed at final follow-up [6, 7, 27, 28, 31] (Tables 3, 4) Fig. 1.
Hypokyphosis and pulmonary function
Recent studies showed that thoracic volume is positively correlated with TK (r = 0.31, p = 0.006) and that forced vital capacity and forced expiratory volume in 1 s are significantly lower in hypokyphotic patients (p = 0.04 and p = 0.03, respectively) and correlated with thoracic volume and T4–T12 kyphosis [2]. Johnston et al. [1] previously reported that preoperative pulmonary tests were clinically impaired in 19 % of AIS patients and correlated significantly with the main thoracic curve and sagittal plane deformity severity. These findings reinforce the importance of sagittal alignment improvement.
Posteromedial translation technique
The posteromedial translation technique using sublaminar bands has been widely described, with successful results in both AIS and neurological scoliosis [18, 32]. Previously, Mazda [33] demonstrated that posteromedial translation could reduce cervical and thoracic flattening in AIS. A similar improvement in cervical lordosis was found in the present study with a mean gain of 9°. Sales de Gauzy et al. [34] and Ilharreborde et al. [18] have also confirmed that hybrid constructs including sublaminar bands improved both sagittal and coronal correction compared to hook hybrid constructs. Their results confirmed that there was no significant loss of either immediate postoperative sagittal improvement or coronal correction achieved by sublaminar band hybrid constructs, consistent with the results of the current study at 2-year follow-up. The current study revealed an effective correction of hypokyphosis in AIS patients: 56.4 and 63.4 % of the patients had a postoperative kyphosis greater than 20° postoperatively, respectively, in the group with and without AER. This suggests that AER does not provide additional sagittal correction when posteromedial translation with sublaminar bands is used for AIS correction. These findings could be explained by the deformity correction technique mediated by sublaminar bands, which progressively translate the spine toward the rods present in the sagittal plane [14]. A similar successful correction was achieved in the coronal plane by the two techniques (Fig. 1). In the group without AER, mean coronal correction of 63.4 % was similar to that obtained in previous series [27, 35]. In the group with AER, mean coronal correction was 56.4 %. In the latter group, the preoperative Cobb angle was significantly greater. The larger Cobb angle in group 1 could be associated with stiffer main curve which probably contributed to the greater residual Cobb angle observed in group 1 despite the AER.
Anterior endoscopic release
The first reports of AER were published in the 1990s [36]. Previously, the primary indications for performing anterior release in addition to posterior instrumentation and fusion were the treatment of severe stiff curves or to prevent the crankshaft phenomenon [37, 38]. Some authors reported that thoracoscopic release improves correction compared to posterior surgery alone, and reduces morbidity compared to thoracotomy [39, 40]. Nevertheless, AER is a surgeon-dependent procedure with a learning curve that contributes to morbidity [12, 41]. Moreover, most studies on AER for scoliosis have focused only on coronal correction [39, 42, 43]. Although previous studies have shown that thoracoscopic release improved correction compared to posterior surgery alone, results of the current study did not find a significantly better improvement in Cobb correction with AER. It might be due to use of new posterior implants and techniques such as posteromedial translation [14, 18, 31]. Recently, Longis et al. [44] and Burton et al. [45] studied rigid scoliosis correction with or without anterior release and also reported no differences in frontal correction either postoperatively or at final follow-up. However, to date no study compared AER and posteromedial translation technique in stiff scoliosis curves correction. Moreover, in the current study, 4 (14 %) thoracoscopy-related complications were observed and the length of stay was longer in this group due to the treatment protocol. If indicated, however, thoracoplasty was performed during the same anesthesia as the AER [46].
Limitations of the study
There are several limitations in this study. This is a retrospective study with no functional assessment, but at the time of these surgeries, the SRS 22 questionnaire had not yet been validated in French [47]. The flexibility in the sagittal plane was not routinely assessed preoperatively. However, it could be interesting to analyze the relationship between the preoperative sagittal flexibility and the postoperative kyphosis improvement using a formula similar to the Cincinnati Index [7]. Although the follow-up period was short (a minimum of 2-year follow-up), it is now accepted that almost all loss of coronal correction after fusion in AIS occurs during the first two postoperative years, while the immediate postoperative value of TK tends to improve during follow-up regardless of the posterior construct used [48].
Conclusion
Although previous studies have suggested that thoracoscopic release improved correction compared to posterior surgery alone, the current study did not confirm this finding. Moreover, results of the current series show that no additional significant benefit can be expected in the sagittal plane from AER when the posteromedial translation technique with sublaminar bands is used, even in challenging hypokyphotic patients. The posteromedial translation technique with sublaminar bands is an efficacious and reliable treatment for hypokyphotic AIS, both in the frontal and sagittal planes. Moreover, in patients who underwent AER, more complications occurred with a longer average hospital stay.
References
Johnston CE, Richards BS, Sucato DJ, Bridwell KH, Lenke LG, Erickson M et al (2011) Correlation of preoperative deformity magnitude and pulmonary function tests in adolescent idiopathic scoliosis. Spine 36(14):1096–1102
Ilharreborde B, Dubousset J, Skalli W, Mazda K (2013) Spinal penetration index assessment in adolescent idiopathic scoliosis using EOS low-dose biplanar stereoradiography. Eur Spine J 22(11):2438–2444
Kim YJ, Lenke LG, Bridwell KH, Kim J, Cho SK, Cheh G et al (2007) Proximal junctional kyphosis in adolescent idiopathic scoliosis after 3 different types of posterior segmental spinal instrumentation and fusions: incidence and risk factor analysis of 410 cases. Spine 32(24):2731–2738
Winter RB, Lonstein JE, Denis F (2007) How much correction is enough? Spine 32(24):2641–2643
Suk SI, Lee CK, Kim WJ, Chung YJ, Park YB (1995) Segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis. Spine 20(12):1399–1405
Lowenstein JE, Matsumoto H, Vitale MG, Weidenbaum M, Gomez JA, Lee FY-I et al (2007) Coronal and sagittal plane correction in adolescent idiopathic scoliosis: a comparison between all pedicle screw versus hybrid thoracic hook lumbar screw constructs. Spine 32(4):448–452
Vora V, Crawford A, Babekhir N, Boachie-Adjei O, Lenke L, Peskin M et al (2007) A pedicle screw construct gives an enhanced posterior correction of adolescent idiopathic scoliosis when compared with other constructs: myth or reality. Spine 32(17):1869–1874
Vaccaro Garfin (1995) Pedicle-screw fixation in the lumbar spine. J Am Acad Orthop Surg 3(5):263–274
Cheng I, Kim Y, Gupta MC, Bridwell KH, Hurford RK, Lee SS et al (2005) Apical sublaminar wires versus pedicle screws—which provides better results for surgical correction of adolescent idiopathic scoliosis? Spine 30(18):2104–2112
Sucato DJ, Agrawal S, O’Brien MF, Lowe TG, Richards SB, Lenke L (2008) Restoration of thoracic kyphosis after operative treatment of adolescent idiopathic scoliosis: a multicenter comparison of three surgical approaches. Spine 33(24):2630–2636
Bullmann V, Halm HFH, Schulte T, Lerner T, Weber TP, Liljenqvist UR (2006) Combined anterior and posterior instrumentation in severe and rigid idiopathic scoliosis. Eur Spine J 15(4):440–448
Newton PO, Shea KG, Granlund KF (2000) Defining the pediatric spinal thoracoscopy learning curve: sixty-five consecutive cases. Spine 25(8):1028–1035
King AG, Mills TE, Loe WA Jr, Chutkan NB, Revels TS (2000) Video-assisted thoracoscopic surgery in the prone position. Spine 25(18):2403–2406
Ilharreborde B, Sebag G, Skalli W, Mazda K (2013) Adolescent idiopathic scoliosis treated with posteromedial translation: radiologic evaluation with a 3D low-dose system. Eur Spine J 22(11):2382–2391
Ilharreborde B, Steffen JS, Nectoux E, Vital JM, Mazda K, Skalli W et al (2011) Angle measurement reproducibility using EOS three-dimensional reconstructions in adolescent idiopathic scoliosis treated by posterior instrumentation. Spine 36(20):E1306–E1313
Legaye J, Duval-Beaupère G, Hecquet J, Marty C (1998) Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J 7(2):99–103
Ilharreborde B, Even J, Lefevre Y, Fitoussi F, Presedo A, Souchet P et al (2008) How to determine the upper level of instrumentation in Lenke types 1 and 2 adolescent idiopathic scoliosis: a prospective study of 132 patients. J Pediatr Orthop 28(7):733–739
Ilharreborde B, Even J, Lefevre Y, Fitoussi F, Presedo A, Penneçot G-F et al (2010) Hybrid constructs for tridimensional correction of the thoracic spine in adolescent idiopathic scoliosis: a comparative analysis of universal clamps versus hooks. Spine 35(3):306–314
Lefevre Y, Ilharreborde B, Huot O, Morel E, Fitoussi F, Presedo A et al (2011) Thoracoscopy in children less than 20 kg for the management of spinal disorders: efficacy at long-term follow-up. J Pediatr Orthop 31(2):170–179
Suk S-I, Kim J-H, Kim S-S, Lee J-J, Han Y-T (2008) Thoracoplasty in thoracic adolescent idiopathic scoliosis. Spine 33(10):1061–1067
Lenke LG, Betz RR, Harms J, Bridwell KH, Clements DH, Lowe TG et al (2001) Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis. J Bone Joint Surg Am 83-A(8):1169–1181
Lafage V, Schwab F, Patel A, Hawkinson N, Farcy J-P (2009) Pelvic tilt and truncal inclination: two key radiographic parameters in the setting of adults with spinal deformity. Spine 34(17):E599–E606
Schwab F, Lafage V, Patel A, Farcy J-P (2009) Sagittal plane considerations and the pelvis in the adult patient. Spine 34(17):1828–1833
Kim YJ, Bridwell KH, Lenke LG, Rhim S, Cheh G (2006) Sagittal thoracic decompensation following long adult lumbar spinal instrumentation and fusion to L5 or S1: causes, prevalence, and risk factor analysis. Spine 31(20):2359–2366
Clément J-L, Geoffray A, Yagoubi F, Chau E, Solla F, Oborocianu I et al (2013) Relationship between thoracic hypokyphosis, lumbar lordosis and sagittal pelvic parameters in adolescent idiopathic scoliosis. Eur Spine J 22(11):2414–2420
Suk SI, Kim WJ, Kim JH, Lee SM (1999) Restoration of thoracic kyphosis in the hypokyphotic spine: a comparison between multiple-hook and segmental pedicle screw fixation in adolescent idiopathic scoliosis. J Spinal Disord 12(6):489–495
Kim YJ, Lenke LG, Kim J, Bridwell KH, Cho SK, Cheh G et al (2006) Comparative analysis of pedicle screw versus hybrid instrumentation in posterior spinal fusion of adolescent idiopathic scoliosis. Spine 31(3):291–298
Steib J-P, Dumas R, Mitton D, Skalli W (2004) Surgical correction of scoliosis by in situ contouring: a detorsion analysis. Spine 29(2):193–199
Senaran H, Shah SA, Gabos PG, Littleton AG, Neiss G, Guille JT (2008) Difficult thoracic pedicle screw placement in adolescent idiopathic scoliosis. J Spinal Disord Tech 21(3):187–191
Upendra BN, Meena D, Chowdhury B, Ahmad A, Jayaswal A (2008) Outcome-based classification for assessment of thoracic pedicular screw placement. Spine 33(4):384–390
Clément J-L, Chau E, Vallade M-J, Geoffray A (2011) Simultaneous translation on two rods is an effective method for correction of hypokyphosis in AIS: radiographic results of 24 hypokyphotic thoracic scoliosis with 2 years minimum follow-up. Eur Spine J 20(7):1149–1156
Mazda K, Ilharreborde B, Even J, Lefevre Y, Fitoussi F, Penneçot G-F (2009) Efficacy and safety of posteromedial translation for correction of thoracic curves in adolescent idiopathic scoliosis using a new connection to the spine: the universal clamp. Eur Spine J 18(2):158–169
Ilharreborde B, Vidal C, Skalli W, Mazda K (2012) Sagittal alignment of the cervical spine in adolescent idiopathic scoliosis treated by posteromedial translation. Eur Spine J 22:330–337
Sale de Gauzy J, Jouve J-L, Accadbled F, Blondel B, Bollini G (2011) Use of the universal clamp in adolescent idiopathic scoliosis for deformity correction and as an adjunct to fusion: 2-year follow-up. J Child Orthop 5(4):273–282
Suk S-I, Lee S-M, Chung E-R, Kim J-H, Kim S-S (2005) Selective thoracic fusion with segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis: more than 5-year follow-up. Spine 30(14):1602–1609
Mack MJ, Regan JJ, Bobechko WP, Acuff TE (1993) Application of thoracoscopy for diseases of the spine. Ann Thorac Surg 56(3):736–738
Ogilvie JW (1996) Anterior and posterior spinal surgery: same-day, staged, anterior first, posterior first, or simultaneous? Instr Course Lect 45:99–100
Delécrin J, Brossard D, Takahashi S, Passuti N, Nguyen J-M (2007) Correction of stiff thoracic idiopathic adult scoliosis. Prediction from the traction radiograph. Rev Chir Orthop Reparatrice Appar Mot 93(8):783–788
Newton PO, Marks M, Faro F, Betz R, Clements D, Haher T et al (2003) Use of video-assisted thoracoscopic surgery to reduce perioperative morbidity in scoliosis surgery. Spine 28(20):S249–S254
Reddi V, Clarke DV Jr, Arlet V (2008) Anterior thoracoscopic instrumentation in adolescent idiopathic scoliosis: a systematic review. Spine 33(18):1986–1994
Regan JJ, Guyer RD (1997) Endoscopic techniques in spinal surgery. Clin Orthop Relat Res 335:122–139
Picetti GD 3rd, Pang D, Bueff HU (2002) Thoracoscopic techniques for the treatment of scoliosis: early results in procedure development. Neurosurgery 51(4):978–984 (Discussion 984)
King AG, Mills TE, Loe WA Jr, Chutkan NB, Revels TS (2000) Video-assisted thoracoscopic surgery in the prone position. Spine 25(18):2403–2406
Longis P-M, Odri G, Passuti N, Brossard D, Delécrin J (2011) Does thoracoscopic anterior release of rigid idiopathic scolioses associated with correction by posterior instrumentation result in better long-term frontal and sagittal balance? Orthop Traumatol Surg Res 97(7):734–740
Burton DC, Sama AA, Asher MA, Burke SW, Boachie-Adjei O, Huang RC et al (2005) The treatment of large (>70 degrees) thoracic idiopathic scoliosis curves with posterior instrumentation and arthrodesis: when is anterior release indicated? Spine 30(17):1979–1984
Karami M, Ilharreborde B, Morel E, Fitoussi F, Penneçot G-F, Mazda K (2007) Video-assisted thoracoscopic surgery (VATS) for the treatment of scolioticrib hump deformity. Eur Spine J 16(9):1373–1377
Lonjon G, Ilharreborde B, Odent T, Moreau S, Glorion C, Mazda K (2014) Reliability and validity of the French Canadian version of the Scoliosis Research Society 22 questionnaire in France. Spine 39(1):E26–E34
Remes V, Helenius I, Schlenzka D, Yrjönen T, Ylikoski M, Poussa M (2004) cotrel-dubousset (CD) or universal spine system (USS) instrumentation in adolescent idiopathic scoliosis (AIS): comparison of midterm clinical, functional, and radiologic outcomes. Spine 29(18):2024–2030
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ferrero, E., Pesenti, S., Blondel, B. et al. Role of thoracoscopy for the sagittal correction of hypokyphotic adolescent idiopathic scoliosis patients. Eur Spine J 23, 2635–2642 (2014). https://doi.org/10.1007/s00586-014-3566-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-014-3566-6