Abstract
Purpose
A self-control study was designed to compare the process of creeping substitution between allograft bone and local bone grafting in lumbar interbody fusion.
Methods
From December 2011 to July 2012, 81 patients (mean age: 56.4) were included in this study and randomly allocated to two groups. Leopard cages were using in unilateral instrumentation transforaminal lumbar interbody fusion. In group 1, the cages were filled with the local bone on the side of the instrumentation and allograft bone on the other side. In group 2, they were totally filled with the local bone chips. Then, the special CT-reconstructions were made at 6- and 12-month follow-up. On the sagittal section, the sections of CT-reconstructions were perpendicular to the lateral axis of the cage from the side of the cage to the other side. Similarly, they were parallel to the lateral axis of the cage on the coronal section and intervertebral space on the cross section. The mean area size of bone mass on both sides of the cage was calculated, respectively, using image analysis software (Osirix, version 3.3.2) on each section in two groups.
Results
In group 1, at 6- and 12-month follow-up, significant differences were observed in the mean area size of bone mass between allograft bone and local bone grafting on the coronal, cross, and sagittal section. In group 2, the mean area size of local bone on both sides of the cage had no significant differences at 6- and 12-month follow-up on each section.
Conclusions
The results of our study showed a superiority of local bone grafting over allograft bone.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Transforaminal lumbar interbody fusion (TLIF) augmented with unilateral pedicle screw instrumentation as a minimally invasive technique has become a favored surgical treatment for management of lumbar degenerative disease and spondylolisthesis. Successful clinical outcome often correlates with good bony fusion [1, 2]. Using the cages filled with cancellous bone graft from the iliac crest has been very common, with an excellent clinical outcome. Thereafter, use of cages filled with iliac crest cancellous bone becomes quite popular. However, harvesting autologous bone graft from the iliac crest often requires an additional incision and is associated with a significant morbidity that can reaches 30–40 % [3, 4], which includes hematoma, infection, prolonged chronic pain, and sensory deficit [5–7]. To avoid complications associated with harvesting iliac crest bone autograft, allograft bone has progressively become more and more widespread for substituting iliac crest autograft [8]. The advantages of an allograft lie both in its availability and in the prevention of a second operation coupled with the associated complication rate. Another advantage is the long shelf life of the graft [9]. There is also a markable risk of infectious disease transmission, infection, and immunologic response [10]. Based on the above reasons, using local bone grafting obtained from the lamina and facet joint is a good option. Up until now, the literature has not yielded a quantitative study comparing the use of local bone grafting with the use of allograft bone by radiographic evaluation. The goal of this present study was to report whether the process of creeping substitution differs between local bone grafting and allograft bone by the methods of a self-control study.
Materials and methods
Patient demographics
From December 2011 to July 2012, 40 men and 41 women with a mean age of 56.4 years (range 24–89 years) were included in this study and randomly allocated to two groups. The follow-up averaged 1.3 years (range 1.0–1.5 years). All 81 patients had one-level lumbar disk herniation (LDH) and had a unilateral instrumentation TLIF. Detailed demographics for the patients were given in Table 1.
Surgical method
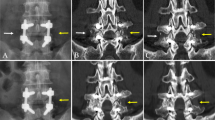
Unilateral instrumentation TLIF was performed using the same technique by one surgeon at the same hospital. The site for incision was based on preoperative symptoms. If a disk herniation or foraminal stenosis was present and predominantly one-sided, then that side was chosen. In general anesthesia, the patient was placed in a prone position. On the paramidline incision, the posterior elements of the spine were exposed to the bases of the transverse processes. After unilateral pedicle screw insertion, the ipsilateral superior and inferior articular processes of one facet joint were resected and the disk was exposed in the neuroforamen. The local bone chips were obtained from resected facet joint and were devoid of all soft tissue attachments. The local bone chips were prepared into the size of 3–5 mm in all dimensions. After discectomy, the endplates were cleared of the cartilage. Then, a Leopard cage (Depuy Spine Inc, Raynham, USA) was inserted in the intervertebral space using a funnel. In group 1, the cages were filled with the local bone chips on the side of the instrumentation and allograft bone on the other side (Fig. 1). In group 2, they were totally filled with the local bone chips obtained by facetectomy, during spinal decompression. No further material was inserted around the cages in either group. The incision was closed in standard fashion.
Radiographic assessment
Each of the patients were given clinical and radiological examinations; preoperatively; postoperatively; and then 2, 4, 6, and 12 months subsequently. For radiographic evaluation, a helical CT scan with sagittal and coronal reconstructions at 6 and 12 months postoperatively was examined by a radiologist specialized in spinal imaging not involved in the treatment, and another radiologist checked CT-reconstruction results. The special CT-reconstructions of vertebral levels addressed in the surgeries were made (Fig. 2). On the sagittal section, the sections of CT-reconstructions with a 1-mm slice thickness were perpendicular to the lateral axis of the cage from the side of the cage to the other side. Similarly, the sections of CT-reconstructions were parallel to the lateral axis of the cage on the coronal section and parallel to intervertebral space on the cross section. Then, the mean area size of bone mass on both sides of the cage was calculated, respectively, using image analysis software (Osirix, version 3.3.2) on each section. In group 1, the mean area size of local bone and allograft bone was compared. In group 2, the mean area size of local bone on both sides of the cage was compared to eliminate the effect of different stress levels on the process of creeping substitution in unilateral instrumentation TLIF. The CT-reconstructions were evaluated independently and blinded by both a radiologist specialized in spinal imaging and two orthopedic surgeons. In this study, fusion was defined as the presence of continuous trabeculae of bone bridging the superior and inferior vertebral endplates on sagittal and coronal reconstructions of CT scan.
Statistical analysis
The data from this study were analyzed through the use of the SPSS 14.0 statistics software program (SPSS Inc., Chicago, USA). A paired t test was used for comparisons of the results. The significance level for all the statistical tests was P = 0.05.
Results
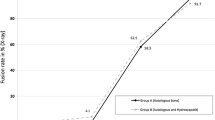
In group 1 (Fig. 3).
At 6-month follow-up, on the coronal section, the mean area size of allograft bone was 474.3 ± 44.77 pix2, while the mean area size of local bone was 723.5 ± 44.79 pix2 (P < 0.05). On the cross section, allograft bone was 416.7 ± 39.05 pix2; local bone was 643.2 ± 45.93 pix2 (P < 0.05). On the sagittal section, allograft bone was 452.3 ± 44.56 pix2; local bone was 703.6 ± 51.03 pix2 (P < 0.05). At 12-month follow-up, on the coronal section, allograft bone was 781.7 ± 50.05 pix2 and local bone was 1,080.5 ± 56.23 pix2 (P < 0.05). On the cross section, allograft bone was 723.8 ± 40.12 pix2 and local bone was 1,015.0 ± 50.76 pix2 (P < 0.05). On the sagittal section, allograft bone was 782.2 ± 48.73 pix2 and local bone was 1,112.7 ± 50.34 pix2 (P < 0.05).
In group 2 (Fig. 4).
At 6-month follow-up, on the coronal section, the mean area size of local bone on both sides of the cage was 745.7 ± 45.12 pix2 (the side of instrumentation) and 705.3 ± 41.57 pix2 (the other side), respectively (P > 0.05). On the cross section, it was 697.5 ± 48.46 pix2 (the side of instrumentation) and 652.3 ± 46.13 pix2 (the other side) respectively (P > 0.05). On the sagittal section, it was 782.6 ± 44.67 pix2 (the side of instrumentation) and 689.2 ± 43.67 pix2 (the other side), respectively (P > 0.05). At 12-month follow-up, on the coronal section, the mean area size of local bone on both sides of the cage was 1,104.5 ± 57.67 pix2 (the side of instrumentation) and 1,023.0 ± 53.34 pix2 (the other side), respectively (P > 0.05). On the cross section, it was 1,134.0 ± 56.79 pix2 (the side of instrumentation) and 1,056.4 ± 53.12 pix2 (the other side), respectively (P > 0.05). On the sagittal section, it was 1,066.0 ± 52.25 pix2 (the side of instrumentation) and 1,005.0 ± 48.45 pix2 (the other side), respectively (P > 0.05). Detailed data for the patients were given in Table 2.
Discussion
The present study was the first in conducting a quantitative comparison of the clinical application of local bone grafting with allograft bone, which could provide an objective presentation about the process of creeping substitution. Lumbar fusion was increasingly performed for management of degenerative lumbar spine diseases. Despite technological advances in instrumentation techniques in spine surgery, achieving solid bony fusion remained important for optimal clinical outcome [1, 2, 11]. In group 1, the results at 6 and 12 months postoperatively revealed that local bone grafting had an obvious advantage over allograft bone in the process of creeping substitution (Figs. 3, 5). Figure 5 showed the visible results that the mean area size of local bone was bigger than the mean area size of allograft bone at 6 and 12 months postoperatively. Similarly, conducted animal experiments also had shown a superiority of autogenous over allogenic cancellous bone [12]. The different process of creeping substitution was possibly attributable to a lower biological competence of allograft bone, taking into account the osteoinductivity and osteogenic potential. Biologically, allograft bone appeared to be inferior in terms of a lack of osteoinductivity and osteogenic potential. The results of group 2 showed that the mean area of both sides of local bone grafting had no significant differences. In unilateral instrumentation TLIF, the stress levels of two sides might be different, which could affect the process of creeping substitution on both sides. Through group 2, the effect of different stress levels on the process of creeping substitution in unilateral instrumentation TLIF could be eliminated, which could further illustrate the reliability of the results of group 1. Therefore, the results of group 1 were convincing. By contrast, Putzier et al. [13] demonstrated that using autogenous cancellous bone could attain similar clinical results comparing with allograft bone. Obviously, this was not consistent with our conclusion. It was maybe attributable to the different evaluation methods and evaluation index that we compared the different process of creeping substitution through the quantifiable area size of bone mass. In addition, the method of experimental design we performed was a self-control study, which could exclude the influence of many factors unrelated to the experiment such as age, gender, and physical status.
The radiological evaluation of fusion must be viewed critically. Beside surgical exploration, it currently represented the only way of obtaining an objective assessment of fusion. Consensus regarding the definition of successful radiographic fusion and the best diagnostic imaging modality to assess lumbar fusions did not exist [14]. A helical CT scan with sagittal and coronal reconstructions had become the preferred imaging to assess lumbar interbody fusion [15]. Most of the studies used plain radiographs to assess the fusion. It had been shown that plain radiographic findings might not be very accurate in demonstrating fusion, which might account for a fairly high fusion rate in various studies and use of CT-reconstructions correlated better with absence of fusion [16]. In this study, fusion was defined as the presence of continuous trabeculae of bone bridging the superior and inferior vertebral endplates on sagittal and coronal reconstructions of CT scan (Fig. 6). In group 1, fusion rate of local bone we achieved was 69 %, which compared favorably with the study by Manish et al. [17], who reported a fusion rate of 67 % with local bone, but it was lower than most other reports using local bone for fusion [17–21] (Table 3). Fusion rate of allograft bone was 62 %. The lower fusion rate in this study can be attributed to a variety of reasons. Although many studies had reported higher fusion rates, the means to assess fusion had also varied. Few studies used thin-slice CT-reconstruction to assess fusion that was often based on chart review and the surgeon’s perception of plain radiograph results, which might lead to an overestimation of fusion rates. Assessment of fusion at a relatively shorter follow-up of 1 year might be another reason for a lower fusion rate in our study. Assessment of fusion at a longer follow-up (up to 2 years) might be more appropriate, but some studies had reported no difference in fusion rate between 1- and 2-year follow-up and had suggested that even 1 year was adequate for assessment of lumbar fusion [22]. Fischgrund et al. [23] in a landmark article found no significant difference in good clinical outcomes in patients with or without fusion, as was seen in this study. To our knowledge, fusion was an important parameter for long-term clinical success. Although it could be argued that successful fusion was not a must for a good outcome, the presence of consistent reports indicated that long-term outcomes were better in patients with fusion than with pseudoarthrosis.
In addition, bone bridging around the cage was observed in most of the cases despite not placing graft at this position. Maybe, this observation was attributable to the hematoma resulting from preparation of the endplates, which served as a primary callus in a bone defect. Bone grafting fell out of the cage when a cage was inserted in the intervertebral space, which may be another reason.
During the production of allograft bone, the osteoconductivity of allograft bone dropped when compared to that of local bone. Whether the reduced osteoconductivity or the lack of both, osteoinductivity and osteogenic potential of allograft bone ultimately lead to a delayed radiological spondylodesis, remained a matter for future research work. We would follow up the follow-up study, and 2-year follow-up results would also be published.
In conclusion, the results of our study showed a superiority of local bone grafting over allograft bone in unilateral instrumentation TLIF. Additionally, local bone grafting had a significant cost savings, taking into account the additional cost of allograft bone. Under the premise of ensuring sufficient disk decompression, using local bone grafting was a wise choice.
References
Bridwell KH, Sedgewick TA, O’Brien MF, Lenke LG, Baldus C (1993) The role of fusion and instrumentation in the treatment of degenerative spondylolisthesis with spinal stenosis. J Spinal Disord 6:461–472
KornblumMB FJ, DA HerkowitzHN A-h, Berkower DL, Ditkoff JS (2004) Degenerative lumbar spondylolisthesis with spinal stenosis: a prospective long-term study comparing fusion and pseudoarthrosis. Spine 29:726–733
Banwart JC, Asher MA, Hassanein RS (1995) Iliac crest bone graft harvest donor site morbidity. A statistical evaluation. Spine 20:1055–1060
Sasso RC, LeHuec JC, Shaffrey C, Spine Interbody Research Group (2005) Iliac crest bone graft donor site pain after anterior lumbar interbody fusion: a prospective patient satisfaction outcome assessment. J Spinal Disord Tech 18:S77–S81
Younger EM, Chapman MW (1989) Morbidity at bone graft donor sites. J Orthop Trauma 3:192–195
Keller EE, Triplett WW (1987) Iliac bone grafting: review of 160 consecutive cases. J Oral Maxillofac Surg 45:11–14
Summers BN, Eisenstein SM (1989) Donor site pain from the ilium: a complication of lumbar spine fusion. J Bone Joint Surg Br 71:677–680
Janssen ME, Lam C (2001) Outcomes of allogenic cages in anterior and posterior lumbar interbody fusion. EurSpine J 10:S158–S168
Pelker RR, Friedlaender GE (1987) Biomechanical aspects of bone autografts and allografts. Orthop Clin North Am 18:235–239
Buck BE, Malinin TI, Brown MD (1989) Bone transplantation and human immunodeficiency virus. An estimate of risk of acquired immunodeficiency syndrome (AIDS). Clin Orthop Relat Res 240:129–136
Zdeblick TA (1993) A prospective, randomized study of lumbar fusion: preliminary results. Spine 18:983–991
Xue Q, Li H, Zou X, Bunger M, Egund N, Lind M, Christensen FB, Bunger C (2005) Healing properties of allograft from alendronate-treated animal in lumbar spine interbody cage fusion. Eur Spine J 14:222–226
Putzier M, Strube P, Funk JF, Gross C (2009) Allogenic versus autologous cancellous bone in lumbar segmental spondylodesis: a randomized prospective study. Eur Spine J18:687–695
McAfee PC, BodenSC BJ (2001) Symposium: a critical discrepancy—a criteria of successful arthrodesis following interbody spinal fusions. Spine 26:320–324
Carreon LY, Glassman SD, Schwender JD (2008) Reliability and accuracy of finecut computed tomography scans to determine the status of anterior interbody fusions with metallic cages. Spine J 8:998–1002
Resnick DK, Choudhri TF, Dailey AT, Groff MW, Khoo L, Matz PG, Mummaneni P, Watters WC, Wang J, Walters BC, Hadley MN (2005) American Association of Neurological Surgeons/Congress of Neurological Surgeons. Guidelines for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 4: radiographic assessment of fusion. J Neurosurg Spine 2:653–657
Kasliwal MK, Deutsch H (2012) Clinical and radiographic outcomes using local bone shavings as autograft in minimally invasive transforaminal lumbar interbody fusion. World Neurosurg 78:185–190
Csécsei GI, Klekner AP, Dobai J, Lajgut A, Sikula J (2000) Posterior interbody fusion using laminectomy bone and transpedicular screw fixation in the treatment of lumbar spondylolisthesis. SurgNeurol 53:2–7
Okuyama K, Kido T, Unoki E, Chiba M (2007) PLIF with a titanium cage and excised facet joint bone for degenerative spondylolisthesis—in augmentation with a pedicle screw. J Spinal Disord Tech 20:53–59
Xiao Y, Li F, Chen Q (2010) Transforaminal lumbar interbody fusion with one cage and excised local bone. ArchOrthop Trauma Surg 130:591–597
Lee JH, Jeon DW, Lee SJ, Chang BS, Lee CK (2010) Fusion rates and subsidence of morselized local bone grafted in titanium cages in posterior lumbar interbody fusion using quantitative three-dimensional computed tomography scans. Spine 35:1460–1465
Singh K, Smucker JD, Gill S, Boden SD (2006) Use of recombinant human bone morphogenetic protein-2 as an adjunct in posterolateral lumbar spine fusion: a prospective CT-scan analysis at one and 2 years. J Spinal Disord Tech 19:416–423
Fischgrund JS, Mackay M, Herkowitz HN, Brower R, Montgomery DM, Kurz LT (1997) Degenerative lumbar spondylolisthesis with spinal stenosis: a prospective, randomized study comparing decompressive laminectomy and arthrodesis with and without spinal instrumentation. Spine 22:2807–2812
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Hui Huang and Chun Jiang have contributed equally to this experiment.
Rights and permissions
About this article
Cite this article
Huang, H., Jiang, C., Feng, Z. et al. Comparing the process of creeping substitution between allograft bone and local bone grafting in lumbar interbody fusion. Eur Spine J 23, 2068–2074 (2014). https://doi.org/10.1007/s00586-014-3388-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-014-3388-6