Abstract
Study design
Retrospective study.
Objective
For successful multilevel correction and stabilization of degenerative spinal deformities, a rigid basal construct to the sacrum is indispensable. The primary objective of this study was to compare the results of two different sacropelvic fixation techniques to conventional stabilization to the sacrum in patients with multilevel degenerative spine disease.
Methods
A total of 69 patients with multisegmental fusion surgery (mean number of stabilized functional spinal units: 7.0 ± 3.3) with a minimum of 1-year follow-up were included. 32 patients received fixation to the sacrum (S1), 23 patients received S1 and iliac screw fixation (iliac) and 14 patients were treated with iliosacral plate fixation (plate). Primary outcome parameters were radiographic outcome concerning fusion in the segment L5–S1, rate of screw loosening, back and buttock pain reduction [numeric rating scale for pain evaluation: 0 indicating no pain, 10 indicating the worst pain], overall extent of disability after surgery (Oswestry Disability Index) and the number of complications.
Results
The three groups did not differ in body mass index, ASA score, the number of stabilized functional spinal units, duration of surgery, the number of previous spine surgeries, or postoperative complication rate. The incidence of L5–S1 pseudarthrosis after 1 year in the S1, iliac, and plate groups was 19, 0, and 29 %, respectively (p < 0.05 iliac vs. plate). The incidence of screw loosening after 1 year in the S1, iliac, and plate groups was 22, 4, and 43 %, respectively (p < 0.05 iliac vs. plate). Average Oswestry scores after 1 year in the S1, iliac, and plate groups were 40 ± 18, 42 ± 20, and 58 ± 18, respectively (p < 0.05 both S1 and iliac vs. plate).
Conclusion
The surgical treatment of multilevel degenerative spine disease carries a significant risk for pseudarthrosis and screw loosening, mandating a rigid sacropelvic fixation. The use of an iliosacral plate resulted in an inferior surgical and clinical outcome when compared to iliac screws.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The number of elderly patients with adult spinal scoliotic deformities with the need for multilevel spinal stabilization is growing. This is one of the reasons for the increasing number of lumbosacropelvic fusion surgeries in the past decade [1]. Because of the complexity of the regional anatomy of the lumbosacropelvic junction and the large prying effect due to the length of the lever, the results after multilevel spinal stabilization in degenerative spine disease are often hampered by inadequate fixation of the basal construct. Pseudarthrosis at L5/S1 and loosening of the S1 pedicle screws are common problems. In previous studies, the pseudarthrosis rates after stabilization to the sacrum varied widely (3–83 %) [2, 3]. This high complication rate can be explained by the poor bone quality in elderly patients and the substantial biomechanical forces at the lumbosacropelvic junction [3–6].
In order to take this into account, various strategies have been recently introduced to improve the rigidity of the basal construct [4–7]. Previous studies could demonstrate the increased risk for postoperative complications with long-level fusions ending at the sacrum [8]. A solution to that problem was an extension of the stabilization construct to the pelvis. One of the first surgical techniques that showed a significant improvement concerning the pseudarthrosis and complication rate was the Galveston technique, which was later replaced by the insertion of iliac screws that are connected to the regular rod system [9, 10].
From the biomechanical standpoint, the insertion of additional iliac screws is superior to the Galveston technique due to the increased pullout strength, and from the surgical standpoint it is superior due to easier handling [11]. One of the limitations of this technique is the high rate of instrumentation prominence and associated pain that led to screw removal in 22 % of the patients after 2 years in one publication [12]. As a valid alternative to the iliac screws, the implantation of a sacroiliac plate device has been introduced. It has proven to be an elegant and solid sacroiliac fixation technique. However, although conceptually appealing, the experience with the sacroiliac plate is limited to young patients with good bone quality [13].
The aim of this retrospective analysis was to compare the effectiveness and early complication rates for distinct basal fixation techniques applied to multilevel deformity correction in the treatment of degenerative scoliosis. To this end, we focused (1) on a comparison of conventional iliosacral fixation with regular fixation to the sacrum, as well as (2) on a comparison of sacroiliac plate fixation to the established screw techniques. We hypothesized that a solid sacropelvic fixation would reduce the high rates of pseudarthrosis and screw loosening due to its high pullout force [14]. We further hypothesized that the use of a sacropelvic plate provides a more solid basal fixation and more rigid construct than S1/iliac screws [4].
Materials and methods
Clinical data were collected by a chart review. A total of 69 patients were included in this retrospective analysis. All patients had the diagnosis of multilevel degenerative spine disease. Indications for multisegmental spinal fusion were the following: severe adult scoliosis, progression (clinically and radiographically) of the deformity, multisegmental instability, and adjacent segment disease after previous surgeries.
Patient characteristics
We included patients who were treated between 2009 and 2012 at a single institution with a minimum follow-up of 1 year. The surgeries were performed by five senior spine surgeons. When the patient received sacropelvic stabilization it was the surgeon's choice of which technique (iliac screws vs. sacropelvic plate) was used.
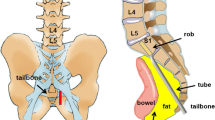
We identified 37 patients who were treated with sacropelvic stabilization (iliac screw 23 patients, sacropelvic plate 14 patients), as a control we used 32 consecutive patients who were stabilized only to S1 (Fig. 1).
In this study, we did not include patients under 18 years, patients with neuromuscular disease or juvenile scoliosis or patients with previous history of spinal metastases. Details of the patient demographics are shown in Table 1.
Surgical parameters
Of the 69 patients, 37 patients were stabilized using TLIF technique and 14 patients were stabilized in PLIF technique (Medtronic CD Horizon Legacy Spinal System™, Medtronic CD Horizon Solera Spinal System™, Medtronic Colorado 2 Titan Spinal System™, Aesculap S4® Spinal System). Ten patients received TLIF and PLIF cages in different segments due to previous spine surgeries. The remaining eight patients were either stabilized from ventral (6 patients in ALIF technique) or without any disk replacement (2 patients). 38 patients were stabilized using PEEK cages (Aesculap T-Space PEEK™, Aesculap Pro-Space PEEK™), 14 patients received titan cages (Aesculap T-Space Titan™, Aesculap Pro-Space Titan™) and 15 patients had a combination of PEEK and titan cages. The extent of the ventral support is shown in the Fig. 2.
Nine patients underwent Smith Peterson osteotomy due to severe sagittal imbalance (7 patients in L4, and 2 patient in L3 or L5). Because of osteoporotic bone quality, we augmented the vertebral bodies with bone cement in 16 patients to further prevent screw loosening.
The rod diameter in all three groups was 5.5 mm. If the patient was treated with iliac screws, we used screws with a diameter of 8.5 mm and a length of 90 mm (Medtronic Legacy Iliac MAS Titan™ Art. No. 70468590). In the iliosacral plate group, an iliac screw with a diameter of 7 mm and a length of 80 mm was used (Medtronic Colorado 2 Titan™ Art. No. 8632080). The iliosacral plate system (Medtronic Colorado 2 Titan™ Art. No. 8638210, 8638220) does not lock the iliac screw at the plate in comparison to the sacropelvic screws that can be secured. Pedicle screw sizes and diameters were chosen dependent on the pedicle anatomy, which was evaluated on the preoperative CT scans. Details of the surgical parameters are shown in Table 2.
Follow-up parameters
The follow-up timepoints were 3 and 12 months after surgery. For assessing the radiographic outcome, every patient had either radiographs (a.p. and lateral) or a CT scan. The fusion rate was evaluated using the criteria that were previously reported by Hyun et al. [15]. If a pathological finding was diagnosed on a radiograph, the patient received additional CT scans.
The complication rate was evaluated according to the chart review, and was divided into minor complications and neurological complications. Demographic data including the ASA score were evaluated by the chart review. The ASA score is a grading system developed to assess the fitness and health status of patients before surgery, ranging from 1 = healthy patient to 5 = moribund patient [16].
Patients were asked to complete one questionnaire (Oswestry Disability Index: ODI) at the 12-month follow-up. Additional questions included the numeric rating scale for pain evaluation concerning back pain before surgery and after 12 months (NRS, 0 indicating no pain, 10 indicating the worst pain). To evaluate the overall satisfaction, the patient was asked if he or she would undergo the same surgery again, had the result been known ahead.
The data collection and analysis did not involve any of the operating surgeons. Statistical analysis was performed using SPSS 20.0. p values below 0.05 were defined as significant.
The retrospective chart review was approved by the local ethics committee (reference number: EA2/093/13).
Results
Between the three groups there were no significant differences concerning the demographics: age (S1: 63.6 ± 9.2 years; iliac: 67.1 ± 11.1 years; plate: 69.5 ± 9.9 years; p = 0.20), body mass index (S1: 27.1 ± 4.8; iliac: 26.1 ± 3.2; plate: 27.2 ± 4.5; p = 0.35), the physical status of the patients before surgery assessed with the ASA classification system (S1: 1.6 ± 1.1; iliac: 2.1 ± 0.9; plate: 1.9 ± 0.7; p = 0.17) or the number of previous spine surgeries (S1: 1.9 ± 1.6; iliac: 2.0 ± 1.7; plate: 1.9 ± 1.4; p = 0.96) (Table 1). Comparing the surgical parameters there were likewise no differences between the groups (Table 2). The postoperative complication rate concerning minor complications, i.e., wound infections, re-bleeding or cerebrospinal fluid fistulas was comparable among the three groups (Table 3). In total, 17 patients (24.6 %) underwent early surgical revision.
In total, we had a neurological complication rate of 8.7 % over all three groups. 5 out of the 69 patients had a temporary muscle palsy that was absent at the 12-month follow-up. One patient had a new postoperative incontinence (bowel and bladder) which did not improve after 1 year. A postoperative spinal epidural hematoma, that was immediately removed after diagnosis, could be identified as the cause for the new symptom. The neurological complication rate between the groups was without a statistical difference (Table 3).
In total, we had ten cases of pseudarthrosis in the segment L5–S1 after 1 year (average over all groups 14.5 %). Of those, six patients had undergone regular stabilization to the sacrum (19 %) and four patients received iliosacral plate fixation (29 %). In the group that received iliac screws we had no case of pseudarthrosis (0 %). The difference in the incidence of L5/S1 pseudarthrosis between the two sacropelvic fixation groups was significant (p = 0.033). In parallel, 14 patients required revision surgeries due to screw loosening or material dislocation (in total 20.3 %): n = 7 in the S1 group (22 %), n = 6 in the iliosacral plate fixation group (43 %), and n = 1 in the iliac screw group (4 %). Again, the difference between the two sacropelvic fixation groups was significant (p = 0.048).
One-year improvement in back pain, evaluated with the numeric rating scale (S1: 4.0 ± 2.5; iliac: 4.1 ± 1.8; plate: 3.6 ± 3.5; p = 0.86) was not statistically different between the groups. All patients improved by around 4 points on the NRS scale after surgery, after 1 year. We could also not show any difference in the patients decision undergoing the same surgery again, had the result been known ahead (S1: 0.31 ± 0.64; iliac: 0.38 ± 0.65; plate: 0.29 ± 0.61; p = 0.76). Average Oswestry scores after 1-year follow-up were significantly worse in the iliosacral plate fixation group (57.8 ± 17.5) when compared to the iliac screw group (41.7 ± 19.9; p = 0.041), as well as the control group (40.3 ± 17.6; p = 0.017).
Discussion
The principal findings of this retrospective analysis of three different basal fixation techniques for longstanding constructs in the treatment of multilevel degenerative spine disease are that (1) the incidence of L5/S1 pseudarthrosis using transforaminal interbody fusion techniques seems to be reduced by primary addition of iliac screws to regular sacral fixation, (2) the use of a sacroiliac plate with its current design is associated with a higher incidence of pseudarthrosis and hardware failure than classic S1/iliac screw fixation, (3) the clinical short- to mid-term outcome when using a sacroiliac plate is inferior to both conventional S1 and S1/iliac screw fixation.
Due to the increasing number of elderly patients with multilevel degenerative spine disease, surgical treatment options for adult spinal deformity are gaining an increasing attention. Several studies have proven superiority of multilevel surgical spondylodesis over conservative treatment in the past, given that patients are selected carefully [17–21]. In this retrospective study, we compared three different surgical treatment options for patients with multilevel degenerative spine disease. Additional iliac fixation has already been proven to be more effective than secondary sacropelvic fixation points in the biomechanical laboratory [14, 22]. In the clinical setting, the benefit of additional iliac screws could be shown in patients with neuromuscular spinal deformities [23]. Sponseller et al. [24, 25] could also show in the pediatric population that a solid distal “foundation” with pelvic fixation can improve the deformity correction in terms of improving the coronal and sagittal balance significantly in comparison to regular sacral fixation. One group found an evidence that the use of iliac screws can be beneficial when it comes to a revision surgery in failed lumbosacropelvic fixation. Here, an increased rate of successful fusion in the segment L5–S1 could be demonstrated [26].
One common general problem in lumbosacropelvic fusion surgery in the treatment of multilevel degenerative disease is the high rate of pseudarthrosis, especially in the aging population [10, 22, 27, 28]. Pseudarthrosis rates between 3 and 83 % can be found in the literature [2, 3, 29]. In our patient cohort, we had, based on our radiographic evaluation, a primary non-fusion in the segment L5–S1 after 1 year in 15 % of the cases. Unexpectedly, the worst result was achieved in the iliosacral plate device group. Intuitively, we had expected that the addition of a plate to sacroiliac plate fixation would represent the strongest basal construct. However, in this group, the rate of pseudarthrosis was as high as 29 %. In contrast, the regular iliac screws proved to be statistically superior with a pseudarthrosis rate of 0 % after the first year.
As previously described in other studies, we experienced a significant number of hardware failure (20 % over all estimated groups) [2, 15]. Again, the worst results were obtained when using the iliosacral plate fixation technique. This result may reflect the fact that the iliac screws in the sacropelvic plate device are shorter and of lower diameter and cannot be locked into the sacropelvic plate. In five cases, the iliac screws backed out of the plate early after surgery (Fig. 3a, b).
a Postoperative CT scan showing the loosening of the right iliac screw (green arrow) with a dorsal displacement of 29 mm in a patient with iliosacral plate device. b Postoperative radiographs in the a.p. and lateral view showing the loosening of both iliac screws (green arrows) in a patient with iliosacral plate device
It is known that a number of iliac screws will need to be removed because of prominence of the material and the associated problems of constant pain and the unability to sit on hard components [2, 7]. We had one patient who was readmitted and had one iliac screw removed because of prominence of the screw head. There was no need for reinsertion of the screw, the segments were already successfully fused. Recent papers have shown promising new minimally invasive approaches and techniques to prevent hardware prominence and to reduce morbidity showing the loosening of the right [30–32].
The total rate of almost 25 % of minor complications after surgery shows the increased perioperative risk in elderly patients receiving long-level spinal stabilization procedures. Our results are consistent with previous published complication rates [21, 33]. Most studies, however, show that the total rate of minor perioperative complications does not influence the patient outcome in the long run [34]. Accordingly, in our study, we also did not find any correlation between the minor complication rate and the outcome parameters after 1 year.
The increased complexity of stabilizing patients with multilevel degenerative spine disease is also reflected in the neurological complication rate. In total, we had a complication rate of 8.7 % over all three groups. Only one of the patients showed a permanent neurological deficit in the 1-year follow-up (1.4 %). A recent study evaluated the postoperative neurological complication rate in a patient cohort undergoing surgery for fixed sagittal imbalance with pedicle substraction osteotomy. This patient cohort is resembling our patient cohort concerning the complexity of underlying spine disease. Here, the complication rates were 10.7 % for short-term deficits and 2.1 % for permanent deficits [35]. Our neurological complication rate is in the regular to be expected range.
Despite the high rates of screw loosenings and minor complications, around 60 % of all the patients were satisfied and would not hesitate to repeat the surgery if they had the choice again. There was no difference between the groups. Only, when the patients were evaluated with the Oswestry score we did find a difference between the groups. Here, the sacroiliac plate device group was significantly worse with an average score of 57.8 compared to the iliac screw group with an average score of 41.7 and the S1 group with an average score of 40.3.
Conclusion
In this study, we could show that there are no changes in morbidity, mortality or the incidence of postoperative back pain by additionally placing iliac screws to create a rigid basal construct when compared to the regular stabilization technique to the sacrum. The iliac screws were superior to the implantation of the sacral plate regarding postoperative disability, screw loosening and pseudolisthesis in the segment L5/S1. Our first results with the sacropelvic plate device in the current design are rather disappointing. The initial assumption that the iliosacral plate fixation is superior to regular iliac screws could not be corroborated. We have changed our implantation policy and have abandoned the use of the sacroiliac plate.
We still feel, that the concept of a rigid basal plate fixation might be worthwhile pursuing if there are a few changes in the plates design. Improvements might include a locking mechanism for the iliac screws and the possibility to use longer screws with a bigger diameter.
In this study, we only evaluated a small patient cohort in a retrospective fashion. What is needed in the future is a randomized trial that prospectively compares iliac screw placement with standard sacropelvic fixation in an aged patient group.
But knowing the limitations of this study we still think that we can prove that the placement of regular iliac screws is an effective technique that provides added structural support to S1 screws in long-segment spinal fusions in appropriately selected patients.
References
Deyo RA, Nachemson A, Mirza SK (2004) Spinal-fusion surgery—the case for restraint. N Engl J Med 350:722–726
Tsuchiya K, Bridwell KH, Kuklo TR, Lenke LG, Baldus C (2006) Minimum 5-year analysis of L5-S1 fusion using sacropelvic fixation (bilateral S1 and iliac screws) for spinal deformity. Spine 31:303–308
Kim YJ, Bridwell KH, Lenke LG, Rhim S, Cheh G (2006) Pseudarthrosis in long adult spinal deformity instrumentation and fusion to the sacrum: prevalence and risk factor analysis of 144 cases. Spine 31:2329–2336
Early S, Mahar A, Oka R, Newton P (2005) Biomechanical comparison of lumbosacral fixation using Luque-Galveston and Colorado II sacropelvic fixation: advantage of using locked proximal fixation. Spine 30:1396–1401
Tomlinson T, Chen J, Upasani V, Mahar A (2008) Unilateral and bilateral sacropelvic fixation result in similar construct biomechanics. Spine 33:2127–2133
Kebaish KM (2010) Sacropelvic fixation: techniques and complications. Spine 35:2245–2251
Kuklo TR, Bridwell KH, Lewis SJ, Baldus C, Blanke K, Iffrig TM, Lenke LG (2001) Minimum 2-year analysis of sacropelvic fixation and L5-S1 fusion using S1 and iliac screws. Spine 26:1976–1983
Charosky S, Guigui P, Blamoutier A, Roussouly P, Chopin D, Study Group on S (2012) Complications and risk factors of primary adult scoliosis surgery: a multicenter study of 306 patients. Spine 37:693–700
Allen BL Jr, Ferguson RL (1982) The Galveston technique for L rod instrumentation of the scoliotic spine. Spine 7:276–284
Allen BL Jr, Ferguson RL (1984) The Galveston technique of pelvic fixation with L-rod instrumentation of the spine. Spine 9:388–394
Schwend RM, Sluyters R, Najdzionek J (2003) The pylon concept of pelvic anchorage for spinal instrumentation in the human cadaver. Spine 28:542–547
Emami A, Deviren V, Berven S, Smith JA, Hu SS, Bradford DS (2002) Outcome and complications of long fusions to the sacrum in adult spine deformity: luque-galveston, combined iliac and sacral screws, and sacral fixation. Spine 27:776–786
D C (1991) A new device for pelvic fixation for spinal surgery: the sacral block. In: 8th proceeding of the international congress of cotrel-dubousset instrumentation. Minneapolis, MN
Lebwohl NH, Cunningham BW, Dmitriev A, Shimamoto N, Gooch L, Devlin V, Boachie-Adjei O, Wagner TA (2002) Biomechanical comparison of lumbosacral fixation techniques in a calf spine model. Spine 27:2312–2320
Hyun SJ, Rhim SC, Kim YJ, Kim YB (2010) A mid-term follow-up result of spinopelvic fixation using iliac screws for lumbosacral fusion. J Korean Neurosurg Soc 48:347–353
Mak PH, Campbell RC, Irwin MG, American Society of A (2002) The ASA physical status classification: inter-observer consistency. American Society of Anesthesiologists. Anaesth Intensive Care 30:633–640
Crawford CH 3rd, Carreon LY, Bridwell KH, Glassman SD (2012) Long fusions to the sacrum in elderly patients with spinal deformity. Eur Spine J 21:2165–2169
Bridwell KH, Glassman S, Horton W, Shaffrey C, Schwab F, Zebala LP, Lenke LG, Hilton JF, Shainline M, Baldus C, Wootten D (2009) Does treatment (nonoperative and operative) improve the two-year quality of life in patients with adult symptomatic lumbar scoliosis: a prospective multicenter evidence-based medicine study. Spine 34:2171–2178
Li G, Passias P, Kozanek M, Fu E, Wang S, Xia Q, Li G, Rand FE, Wood KB (2009) Adult scoliosis in patients over sixty-five years of age: outcomes of operative versus nonoperative treatment at a minimum two-year follow-up. Spine 34:2165–2170
Smith JS, Shaffrey CI, Berven S, Glassman S, Hamill C, Horton W, Ondra S, Schwab F, Shainline M, Fu KM, Bridwell K, Spinal Deformity Study G (2009) Improvement of back pain with operative and nonoperative treatment in adults with scoliosis. Neurosurgery 65:86–93 (discussion 93–84)
Smith JS, Shaffrey CI, Glassman SD, Berven SH, Schwab FJ, Hamill CL, Horton WC, Ondra SL, Sansur CA, Bridwell KH, Spinal Deformity Study G (2011) Risk-benefit assessment of surgery for adult scoliosis: an analysis based on patient age. Spine 36:817–824
Alegre GM, Gupta MC, Bay BK, Smith TS, Laubach JE (2001) S1 screw bending moment with posterior spinal instrumentation across the lumbosacral junction after unilateral iliac crest harvest. Spine 26:1950–1955
Peelle MW, Lenke LG, Bridwell KH, Sides B (2006) Comparison of pelvic fixation techniques in neuromuscular spinal deformity correction: galveston rod versus iliac and lumbosacral screws. Spine 31:2392–2398 (discussion 2399)
Akbarnia BA, Breakwell LM, Marks DS, McCarthy RE, Thompson AG, Canale SK, Kostial PN, Tambe A, Asher MA, Growing Spine Study G (2008) Dual growing rod technique followed for three to eleven years until final fusion: the effect of frequency of lengthening. Spine 33:984–990
Sponseller PD, Yang JS, Thompson GH, McCarthy RE, Emans JB, Skaggs DL, Asher MA, Yazici M, Poe-Kochert C, Kostial P, Akbarnia BA (2009) Pelvic fixation of growing rods: comparison of constructs. Spine 34:1706–1710
Harimaya K, Mishiro T, Lenke LG, Bridwell KH, Koester LA, Sides BA (2011) Etiology and revision surgical strategies in failed lumbosacral fixation of adult spinal deformity constructs. Spine 36:1701–1710
Leong JC, Lu WW, Zheng Y, Zhu Q, Zhong S (1998) Comparison of the strengths of lumbosacral fixation achieved with techniques using one and two triangulated sacral screws. Spine 23:2289–2294
Stovall DO Jr, Goodrich JA, Lundy D, Standard SC, Joe C, Preston CD (1997) Sacral fixation technique in lumbosacral fusion. Spine 22:32–37
Kim YJ, Bridwell KH, Lenke LG, Cho KJ, Edwards CC 2nd, Rinella AS (2006) Pseudarthrosis in adult spinal deformity following multisegmental instrumentation and arthrodesis. J Bone Joint Surg Am 88:721–728
Wang MY (2012) Percutaneous iliac screws for minimally invasive spinal deformity surgery. Minim Invasive Surg 2012:173685
Wang MY, Williams S, Mummaneni PV, Sherman JD (2012) Minimally invasive percutaneous iliac screws: initial 24 case experience with CT confirmation. J Spinal Disord Tech. doi:10.1097/BSD.0b013e3182733c43
Tumialan LM, Mummaneni PV (2008) Long-segment spinal fixation using pelvic screws. Neurosurgery 63:183–190
Pateder DB, Gonzales RA, Kebaish KM, Cohen DB, Chang JY, Kostuik JP (2008) Short-term mortality and its association with independent risk factors in adult spinal deformity surgery. Spine 33:1224–1228
Glassman SD, Hamill CL, Bridwell KH, Schwab FJ, Dimar JR, Lowe TG (2007) The impact of perioperative complications on clinical outcome in adult deformity surgery. Spine 32:2764–2770
Kim KT, Lee SH, Suk KS, Lee JH, Jeong BO (2012) Outcome of pedicle subtraction osteotomies for fixed sagittal imbalance of multiple etiologies: a retrospective review of 140 patients. Spine 37:1667–1675
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Finger, T., Bayerl, S., Onken, J. et al. Sacropelvic fixation versus fusion to the sacrum for spondylodesis in multilevel degenerative spine disease. Eur Spine J 23, 1013–1020 (2014). https://doi.org/10.1007/s00586-014-3165-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-014-3165-6