Abstract
Purpose
To determine the postoperative temporal course of the forces acting on a vertebral body replacement (VBR) for two well reproducible activities.
Methods
A telemeterised VBR was implanted in five patients. It allows the measurement of six load components. Implant loads were measured in up to 28 measuring sessions for different activities, including standing and walking.
Results
The postoperative temporal course of the resultant implant forces measured during standing and walking was similar in each patient, but the patterns varied strongly from patient to patient. In one patient, the forces decreased in the first year and then increased in the following 4 years. In another patient, the forces increased in the first few months and then decreased. In a third patient, the forces varied only slightly in the postoperative time. In two patients, there was a strong drop of the implant force in the first two postoperative months. The force was on average approximately 100 N or 71 % higher for walking than for standing.
Conclusions
The strong force reduction in the first 2 months is most likely caused by implant subsidence, and the force reduction over a period of more than 6 months is most likely caused by fusion of the vertebrae adjacent to the VBR. The short-term force increase could be attributed to bone atrophy at the index level, and the long-term force increase could be attributed to an increase in the thoracic spine kyphosis angle.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Severe compression fractures of a vertebral body are often stabilised posteriorly with internal spinal fixation devices and anteriorly with a vertebral body replacement (VBR). Autologous bone material is usually added to enhance the fusion process between the adjacent vertebrae. The temporal course of the spinal loads acting on a VBR during the initial fusion phase and the subsequent post fusion phase is completely unknown. With increasing postoperative time, it is assumed that the added bone material stiffens and thus takes over a larger part of the spinal loads [1]. However, no reliable data exist regarding the real long-term temporal course of forces on the VBR. Such data are important for the following purposes:
-
designing and testing fusion implants,
-
a better understanding of the fusion and remodelling processes,
-
the validation of in silico fusion simulation,
-
the understanding of the load sharing within the instrumented spine, and
-
advising patients regarding the activity level necessary to reduce the risk for implant subsidence, especially in elderly patients with osteoporosis.
Only a few in vivo load measurements exist. Intradiscal pressure measurements have been collected by several groups [2–4] to gain essential information of the internal spinal loads for selected body positions and activities. These measurements provide valuable information on healthy subjects. However, they cannot be used to understand basic clinical questions concerning the fusion of vertebral bodies. Furthermore, they are not able to assess the huge variability of the spinal loading, which differs from measuring session to session in realistic daily activities because of the great number of factors involved. These factors include the relative positions of the upper body segments (including the head) and the relaxation state of the muscles. Elfstrom and Nachemson [5] measured the axial forces in inductively powered, telemeterised Harrington distraction rods in 11 patients with scoliosis for a 2-week period. They found that the axial force decreased rapidly within the first 3 days and reached a steady state after 11 days. This force decrease is most likely caused by relaxation of some tissues and has nothing to do with fusion.
Instrumented spinal implants allow the in vivo load measurement in many sessions and can, therefore, be used for a differentiated analysis of the factors that influence spinal loading. Although the transfer of the results to healthy persons has to be handled with care, its conformity with short-term measurements in healthy subjects has been shown several times [6, 7]. In addition to basic science, in vivo measurements from implants are a unique way to obtain clinically relevant information within a patient during the fusion process.
The loads on a telemeterised bisegmental internal spinal fixation device were monitored up to 21 months in ten patients by Rohlmann et al. [8]. They found an increase in fixator loads shortly after anterior interbody fusion with one or two autologous iliac-crest bone grafts but without an anterior implant. In most patients, the loads retained the same high level even after fusion had taken place. From the spinal fixator loading curves, the time of fusion could not be pinpointed.
The loads on a VBR have been measured by Rohlmann et al. [9–11] for several activities such as sitting, standing, physiotherapy, whole-body vibration, and lifting up and laying down a weight. The long-term load changes on a VBR, however, have not been studied.
The aim of this study was to determine the loads on a VBR in the postoperative temporal course for standing and walking. We hypothesised that the force on the VBR remains constant in the first few postoperative months, gradually decreases over a period between 6 and 12 months, and then remains constant afterwards.
Materials and methods
Telemeterised implant and patients
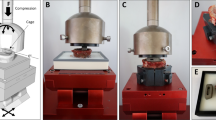
A clinically established VBR (Synex, Synthes, Bettlach, Switzerland) was modified. Six strain gauges, a telemetry unit, and a coil for the inductive power supply were integrated in a hermetically closed cylinder (Fig. 1). Screwed-on endplates of various heights allowed intraoperative adapting of the implant height to the defect dimensions. The instrumented VBR allows the measurement of all force and moment components. Prior to implantation, the implants were extensively calibrated. Compressive and shear forces were applied on the implant at 21 points causing defined combinations of forces and moments of up to 3,000 N and 20 Nm. The measurement accuracy was better than 2 % for forces and 5 % for moments relative to the calibration ranges. The sensitivity of the measuring implant is smaller than 1 N for the force components and smaller than 0.01 Nm for the moments. The implant has been described in detail elsewhere [12].
Sectioned image of the instrumented vertebral body replacement (from Rohlmann et al. [10])
Instrumented VBRs were implanted in five patients (WP1–WP5) who had A3 type compression fractures (classification after Magerl et al. [13]) of a vertebral body. In four patients, the L1 vertebral body was fractured, and in one patient (WP5) the L3 vertebral body was fractured. Detailed information about the patients is provided in Table 1. In a first surgery, the fracture was stabilised from the posterior using an internal spinal fixation device. In a second surgery, parts of the fractured vertebral body and the adjacent intervertebral discs were removed, and the VBR was inserted in the corpectomy defect. To enhance the interbody fusion process, autologous bone material was added.
For the measurements, a coil was placed around the patient’s trunk at the level of the implant to supply power. An antenna on the patient’s back received the signals from the telemetry and transmitted them to a notebook. The patients were videotaped during the measurements, and the load-dependent telemetry signals were stored on the same videotape. The load components on the VBR were calculated from the telemetric signals, and the force and moment curves were displayed simultaneously on a notebook monitor. The telemetry and the external equipment have been described in detail elsewhere [14].
The Ethics Committee of our hospital approved implantation of the instrumented implant in the patients (Reference Number 213-01/225-20). Before surgery, the procedure was explained to the patients, and they gave their written, informed consent to the implantation of the telemeterised VBR, taking load measurements, and publication of their images.
Exercises
Initial measurements started 3–7 days after surgery and were repeated 15–28 times in follow-up sessions taking place for up to 65 months. In 97 measuring sessions, the loads for approximately 1,000 different activity and parameter combinations were measured. During most of the sessions, the patient stood relaxed and walked at a self-chosen speed (Table 1). Compared to other exercises such as bending the upper body in different directions, twisting the upper body, and sitting on different seating furniture, the exercises chosen for the current study are well reproducible. Therefore, standing relaxed and walking were the two exercises evaluated in this study.
Evaluation
For the described exercises, the measured moments and the shear forces were mostly small. Thus, mainly the resultant forces (geometrical sum of the three force components) on the implant are reported here.
During each measuring session, the patients stood relaxed an average of nine times for several seconds. For each of these nine trials, the median resultant force was recorded. From the medians of these nine measurements, the median value for that day was determined. The data from the first postoperative days, when the patients still had wound pain and could not stand without support, were not considered in this study. Overall, approximately 730 trials were used to determine the temporal course of the force of standing. The average force for the following time periods was calculated for each patient: 1–2, 3–6, 7–12, 13–24, 25–36, and more than 36 months. These values were then compared with the value from the first time period. In addition, the average values for all patients were determined.
For walking, the maximum force of approximately five typical steps was determined for several trials of a measuring session, and their median and range are presented.
For better interpretation of the temporal course of the implant loads, X-rays and CTs (taken routinely) were evaluated by an independent spine surgeon (P.S.). Furthermore, the shape of the spine was estimated using rasterstereography (Formetric, Germany).
Results
For relaxed standing, the resultant forces on the implant were not constant during the investigated time period but varied within a patient on average by 180 N (range 77–261 N). The loading direction remained almost constant and in a nearly axial direction. The average resultant shear forces between the implant endplate and the vertebra varied by only 48 N (32–63 N). The measured bending moment in a patient varied on average by 0.9 Nm (0.4–1.0 Nm) and the torsional moment varied by 0.7 Nm (0.3–1.7 Nm) throughout the postoperative time.
Figure 2 shows the postoperative temporal courses of the resultant forces on the VBR for relaxed standing. The curves for the five patients differ strongly and display completely different characteristics. In patient WP1, the force decreased during the first 12 months from approximately 225–100 N and then increased to approximately 330 N at five postoperative years. In patient WP2, the implant force increased in the first 10 postoperative months from 300 N to approximately 370 N. Afterwards, the force decreased to approximately 200 N at 21 months. Patient WP3 showed a force decrease from approximately 170–70 N in the first 3 months. At 11 months, a force of 210 N was measured. However, this value decreased within 6 months to approximately 80 N and was then nearly constant for the measurements taken in the following 3 years. In patient WP4, the average force was nearly unchanged for all measurements. Over 49 months, it varied only between 180 and 235 N without a clear trend. In patient WP5, the median of the measured force dropped within the first 6 weeks from 250 N to approximately 100 N and was then constant for nearly 2 years. In the last 20 months, there was a gradual increase in the median by approximately 50 N.
The average resultant force of the five patients decreased for the different time periods studied relative to the value measured in the first 2 months (Fig. 3). On average, it was 12 % lower at three to six postoperative months, 4 % lower at 6–12 postoperative months, 17 % lower in the second year, 22 % lower in the third year, and 11 % lower thereafter. However, there was a great inter-individual variation.
For walking, the forces changed postoperatively in a similar way as those for relaxed standing in all five patients (Fig. 4). Their magnitudes, however, were higher than when standing. The differences in the forces between these two activities were less than 100 N for each patient in the temporal course, except for the first two measuring sessions of patient WP2. This suggests that there is just an offset between the curves for walking and standing. Relative to standing, the resultant force was on the average approximately 100 N or 71 % higher for walking (Fig. 5). However, there is also a large variation in these forces between the patients.
Discussion
The loads on VBR during standing and walking have been monitored postoperatively for up to 65 months. The postoperative force pattern varied considerably between patients and showed no consistent trend. Thus, our hypothesis that the VBR force will generally be constant in the first few postoperative months and then decrease gradually over a period of 6–12 months could not be confirmed. Relative to standing, the force magnitudes for walking had a nearly constant offset, which demonstrate the consistency of our findings for two of the most important activities of daily life.
Effect of global and local factors on the forces
At the level of the VBR, the spinal load is shared by the VBR, the spinal fixation device, the remaining bony structures, and the added bone material. The VBR force is affected by local factors (fusion, pedicle screw loosening, implant subsidence, and bone atrophy) as well as global factors (body weight and change in the upper body centre of mass).
Fusion of the vertebral bodies adjacent to the VBR is a local factor that reduces the loads on the implant. Bony fusion usually requires several months. In a finite element simulation, the compressive force on the VBR decreased by approximately 140 N when the stiffness of the fused bone increased [15]. Loosening of a pedicle screw also reduces the force transferred by the dorsal implant, and thus, it usually leads to an increase in the VBR force. However, if the VBR is prestressed by the fixators, screw loosening reduces the VBR forces. Subsidence of the VBR reduces the implant loads. This usually happens within a short period of time. Atrophy of the non-removed bone during surgery increases VBR forces.
Increased body weight is a global factor that will lead to a force increase on the implant while losing weight will decrease the force [2]. The body weight of each patient varied by no more than 10 % within the measuring period. Thus, this variation can only partly explain the large force changes that occur in the postoperative time. An increase in the kyphosis angle of the thoracic spine leads to an anterior shift of the centre of mass [16]. Therefore, higher back-muscle forces are required to stabilise the upper body. Higher muscle forces also increase the force on the bridged joints and consequently the force on the VBR as well. One has to keep in mind that the patients were between 62 and 71 years old at the time of surgery.
So then in theory, it can be concluded that VBR forces increase by an increase in body weight, by an anterior shift in the body’s centre of mass, by pedicle screw loosening, and by atrophy of the bone remaining at the implant level. The VBR forces are decreased by VBR subsidence, bony fusion, reduced body weight, and pedicle screw loosening (if the VBR is prestressed).
In addition to the afore-mentioned systematic effects on the VBR load, there are some parameters that randomly affect the implant loads during a measurement. The performance of the exercise may vary, e.g. the relative position of arms and head is not always perfectly the same. The inclination of the upper body may also vary slightly. Furthermore, the muscle tonus may differ depending on how relaxed the person is during the measurement [11].
The measured load pattern alone surely cannot explain what actually happened in a patient. Therefore, routinely taken X-rays and CTs were used in addition to load measurements to better interpret and consider the loading on the implant. Furthermore, the body weight was checked several times, and the back shape was measured using a rasterstereographic method.
Discussion of the curves for the different patients
Patient WP1
The force decrease by approximately 120 N for standing within the first 12 months can be explained by fusion of the adjacent vertebrae. This could be confirmed radiologically. The subsequent force increase is most likely caused by an increase in the kyphosis angle. This was confirmed by rasterstereographic measurements. The kyphosis angle increased by 12° between the 30th and 63rd month.
Patient WP2
The force increase within the first few months could be due to bone atrophy of the bone that was not removed during surgery and degeneration of the remaining disc material adjacent to the index level. The force decrease by approximately 150 N between the 10 and 19th months suggests that fusion occurred in this period and that the added bone material took over a larger part of the spinal load. No routine X-ray was available for this time period. The patient died 22 months after surgery because of heart failure that was unrelated to the spinal fracture and the load measurements.
Patient WP3
The force decrease within the first 2 months can be explained by a slight implant subsidence, and the subsequent small force increase can be explained by pedicle screw loosening. The loose screws in combination with pain led to new dorsal instrumentation. Loosening of the screws was confirmed during the surgery. The high force at 11 months is caused by this posterior reinstrumentation. The gradual force decrease by approximately 130 N thereafter until the 17th postoperative month is most likely caused by bony fusion. This was confirmed radiologically.
Patient WP4
The implant loads did not change significantly. An X-ray taken after more than five postoperative years revealed that bony fusion had occurred, but the exact time point could not be pinpointed from the force pattern.
Patient WP5
The rapid force decrease within the first 2 months can only be explained by implant subsidence. The gradual force increase after two postoperative years suggests an anterior displacement in the upper body’s centre of mass due to an increase in the kyphosis angle. Unfortunately that patient was not available for a second rasterstereographic measurement. Fusion was confirmed radiologically at the eighth postoperative month.
General discussion
Until now, it was generally assumed that the implant forces decrease within the first postoperative year due to fusion of the adjacent vertebra and then remain nearly constant. The different loading patterns for the five patients show that this is often not the case. The maximum implant load also does not necessarily occur within the first postoperative weeks but may sometimes occur several years later. This has to be taken into account for many situations, e.g. when designing spinal implants.
Surprisingly, throughout the whole postoperative period, walking caused a nearly constant force offset relative to standing. We had expected a nearly constant force ratio for these exercises. Walking has only a minor effect on the in vivo measured loads in the spinal fixators because the axial stiffness of both the VBR and the bone at that level is much higher than the bending stiffness of the spinal fixators [17–19]. Thus, the load increase during this exercise is mainly shared between the VBR and the surrounding bone.
The rapid force decrease found in patients WP3 and WP5 can only be explained by VBR subsidence. However, subsidence could not be detected on standard X-rays. A small amount is obviously sufficient to strongly reduce the force on the VBR. The bone around the VBR must take over most of the load increase because due to the small amount of subsidence, only a minor part can be shared by the posterior implant, which has a low bending stiffness [17]. This implies that for the patients in this study, the implant subsidence was not accompanied by macroscopic bone damage.
The magnitude of the VBR loads varied strongly from patient to patient. Previous measurements with instrumented internal spinal fixation devices also revealed a large variation in the load magnitude [8]. Sato et al. [3] measured the intradiscal pressure in eight healthy volunteers aged 22–29 years. The pressure in the non-degenerated disc, L4–L5, varied between 215 and 754 kPa for upright standing. A much smaller range is usually expected in such a homogeneous group. The spinal loads obviously depend on several parameters, which are all difficult to control.
Load measurements using telemeterised implants have the great advantage that they allow repeated measurements over a long period of time. In patient WP1, for example, the load while standing was measured 199 times in 22 sessions (Table 1). Other methods, such as the intradiscal pressure measurement, usually permit only one session of measurements. Thus, they just deliver singular results. As our measurements have shown, loads may vary strongly not only within a session but also with time. This is in agreement with a previous study on internal spinal fixation devices [8].
The current study has the limitation that the measurements with this unique technique could be performed only in a small cohort of five patients that were older than 60 years at the time of surgery.
In summary, the temporal course of the resultant VBR force varies strongly from patient to patient. On average, the force decreases slightly over the postoperative time compared to the first 2 months. For walking, there is nearly a constant force offset relative to standing. How the loads are distributed among the two implants, the added bone material, and the non-removed bone depends on several local factors. The desired course of implant load with a continuous decrease within the first postoperative year is clearly not often achieved due to the complexity of the mechanical and biological factors involved. This has to be taken into account when designing spinal fusion implants and also during fusion surgery.
References
White AA 3rd, Panjabi MM (1990) Clinical biomechanics of the spine. J.B.Lippincott Company, Philadelphia-Toronto
Nachemson A (1966) The load on lumbar disks in different positions of the body. Clin Orthop 45:107–122
Sato K, Kikuchi S, Yonezawa T (1999) In vivo intradiscal pressure measurement in healthy individuals and in patients with ongoing back problems. Spine 24:2468–2474
Wilke H-J, Neef P, Caimi M, Hoogland T, Claes LE (1999) New in vivo measurements of pressures in the intervertebral disc in daily life. Spine 24:755–762
Elfstrom G, Nachemson A (1973) Telemetry recordings of forces in the Harrington distraction rod: a method for increasing safety in the operative treatment of scoliosis patients. Clin Orthop 93:158–172
Dreischarf M, Bergmann G, Wilke HJ, Rohlmann A (2010) Different arm positions and the shape of the thoracic spine can explain contradictory results in the literature about spinal loads for sitting and standing. Spine (Phila Pa 1976) 35:2015–2021. doi:10.1097/BRS.0b013e3181d55d52
Rohlmann A, Claes LE, Bergmann G, Graichen F, Neef P, Wilke HJ (2001) Comparison of intradiscal pressures and spinal fixator loads for different body positions and exercises. Ergonomics 44:781–794. doi:10.1080/00140130120943
Rohlmann A, Graichen F, Weber U, Bergmann G (2000) 2000 Volvo Award winner in biomechanical studies: monitoring in vivo implant loads with a telemeterized internal spinal fixation device. Spine (Phila Pa 1976) 25:2981–2986
Rohlmann A, Graichen F, Bender A, Kayser R, Bergmann G (2008) Loads on a telemeterized vertebral body replacement measured in three patients within the first postoperative month. Clin Biomech (Bristol, Avon) 23:147–158. doi:10.1016/j.clinbiomech.2007.09.011
Rohlmann A, Hinz B, Bluthner R, Graichen F, Bergmann G (2010) Loads on a spinal implant measured in vivo during whole-body vibration. Eur Spine J 19:1129–1135. doi:10.1007/s00586-010-1346-5
Rohlmann A, Zander T, Graichen F, Bergmann G (2013) Lifting up and laying down a weight causes high spinal loads. J Biomech 46:511–514. doi:10.1016/j.jbiomech.2012.10.022
Rohlmann A, Gabel U, Graichen F, Bender A, Bergmann G (2007) An instrumented implant for vertebral body replacement that measures loads in the anterior spinal column. Med Eng Phys 29:580–585. doi:10.1016/j.medengphy.2006.06.012
Magerl F, Aebi M, Gertzbein SD, Harms J, Nazarian S (1994) A comprehensive classification of thoracic and lumbar injuries. Eur Spine J 3:184–201
Graichen F, Arnold R, Rohlmann A, Bergmann G (2007) Implantable 9-channel telemetry system for in vivo load measurements with orthopedic implants. IEEE Trans Biomed Eng 54:253–261. doi:10.1109/TBME.2006.886857
Rohlmann A, Zander T, Bergmann G (2006) Effects of fusion-bone stiffness on the mechanical behavior of the lumbar spine after vertebral body replacement. Clin Biomech (Bristol, Avon) 21:221–227. doi:10.1016/j.clinbiomech.2005.10.012
Schwab F, Lafage V, Boyce R, Skalli W, Farcy JP (2006) Gravity line analysis in adult volunteers: age-related correlation with spinal parameters, pelvic parameters, and foot position. Spine 31:E959–E967
Rohlmann A, Graichen F, Bergmann G (2000) Influence of load carrying on loads in internal spinal fixators. J Biomech 33:1099–1104
Rohlmann A, Bergmann G, Graichen F (1997) Loads on an internal spinal fixation device during walking. J Biomech 30:41–47
Rohlmann A, Bergmann G, Graichen F (1999) Loads on internal spinal fixators measured in different body positions. Eur Spine J 8:354–359
Acknowledgments
Funding for this study was obtained from the Deutsche Forschungsgemeinschaft (Ro 581/18-1) and the Deutsche Arthrose-Hilfe, Frankfurt. The authors greatly appreciate the friendly cooperation of their patients. We thank Dr. A. Bender, J. Dymke, and S. Mahmoud for technical assistance, Dr. Ch. Heyde, Dr. R. Kayser, and Dr. U. Weber for their medical support and Dr. H. Mellerowicz, Helios Klinikum Emil von Behring, for providing the Formetric system.
Conflict of interest
The authors have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rohlmann, A., Dreischarf, M., Zander, T. et al. Monitoring the load on a telemeterised vertebral body replacement for a period of up to 65 months. Eur Spine J 22, 2575–2581 (2013). https://doi.org/10.1007/s00586-013-3057-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-013-3057-1